Procedure 66 Arthroscopic Ganglionectomy
Indications
Examination/Imaging
Clinical Examination
 Ganglions are the most common tumors of the hand and represent about 50% to 70% of all soft-tissue hand tumors. Ganglions are more prevalent in females and usually appear between the second and fifth decades of life. Dorsal wrist ganglions are by far the most common cyst and account for 60% to 70% of all hand and wrist ganglions. The origin of the dorsal ganglion, with rare exception, arises over the junction of the dorsal capsule with the scapholunate intraosseous ligament. Angelides and Wallace stated that the transition between the dorsal capsule and the scapholunate interosseous ligament can serve as a duct with a one-way valve mechanism. The main cyst is usually located directly over the scapholunate ligament. However, the cyst may occur anywhere between the extensor tendons and can be connected to the ligament through a long pedicle. Palpation of the mass usually reveals the extent of the cyst in the direction of the pedicle. Transillumination or aspiration confirms the diagnosis preoperatively.
Ganglions are the most common tumors of the hand and represent about 50% to 70% of all soft-tissue hand tumors. Ganglions are more prevalent in females and usually appear between the second and fifth decades of life. Dorsal wrist ganglions are by far the most common cyst and account for 60% to 70% of all hand and wrist ganglions. The origin of the dorsal ganglion, with rare exception, arises over the junction of the dorsal capsule with the scapholunate intraosseous ligament. Angelides and Wallace stated that the transition between the dorsal capsule and the scapholunate interosseous ligament can serve as a duct with a one-way valve mechanism. The main cyst is usually located directly over the scapholunate ligament. However, the cyst may occur anywhere between the extensor tendons and can be connected to the ligament through a long pedicle. Palpation of the mass usually reveals the extent of the cyst in the direction of the pedicle. Transillumination or aspiration confirms the diagnosis preoperatively.
 Open excision of the dorsal ganglion is a time-proven procedure with a low recurrence rate. However, open excision of an occult ganglion frequently requires blunt dissection to identify the ganglion, which may lead to increased scarring and decreased range of motion. Arthroscopic excision allows precise identification of the stock and excision with potentially less scarring.
Open excision of the dorsal ganglion is a time-proven procedure with a low recurrence rate. However, open excision of an occult ganglion frequently requires blunt dissection to identify the ganglion, which may lead to increased scarring and decreased range of motion. Arthroscopic excision allows precise identification of the stock and excision with potentially less scarring.
Imaging
 Radiographs of the involved region are usually unremarkable. Although plain radiographs are usually unremarkable, they may be helpful in evaluating additional pathologic changes to the wrist, including static wrist instability.
Radiographs of the involved region are usually unremarkable. Although plain radiographs are usually unremarkable, they may be helpful in evaluating additional pathologic changes to the wrist, including static wrist instability.
 Arthrograms may show communication of the wrist joint with the cyst via a one-way valve mechanism.
Arthrograms may show communication of the wrist joint with the cyst via a one-way valve mechanism.
 Magnetic resonance imaging (MRI) may be helpful in detection of an occult dorsal ganglion. MRI evaluation is potentially helpful when additional intra-articular pathologic changes are suspected.
Magnetic resonance imaging (MRI) may be helpful in detection of an occult dorsal ganglion. MRI evaluation is potentially helpful when additional intra-articular pathologic changes are suspected.
Surgical Anatomy
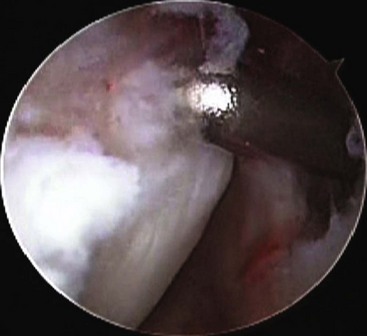
 Typically, the cyst appears between the extensor pollicis longus and the extensor digitorum communis tendons. Arthroscopically, the pearl or the origin of the ganglion stalk from the distal portion of the scapholunate interosseous ligament is identified with the arthroscope in the 4-5 or 6R portals. (Fig. 66-1 shows an arthroscopic view of the scapholunate ligament.) The cyst is seen about two thirds of the time.
Typically, the cyst appears between the extensor pollicis longus and the extensor digitorum communis tendons. Arthroscopically, the pearl or the origin of the ganglion stalk from the distal portion of the scapholunate interosseous ligament is identified with the arthroscope in the 4-5 or 6R portals. (Fig. 66-1 shows an arthroscopic view of the scapholunate ligament.) The cyst is seen about two thirds of the time.
 Attenuation or laxity of the scapholunate interosseous ligament may be seen with the arthroscope in the 3-4 portal and radiocarpal space, or widening of the scapholunate may be seen with the arthroscope in the radial midcarpal portal.
Attenuation or laxity of the scapholunate interosseous ligament may be seen with the arthroscope in the 3-4 portal and radiocarpal space, or widening of the scapholunate may be seen with the arthroscope in the radial midcarpal portal.
Positioning
 The patient is positioned in the traction tower with about 10 pounds of traction.
The patient is positioned in the traction tower with about 10 pounds of traction.
 The wrist is slightly flexed to make it easier to insert the arthroscope and arthroscopic instrumentation.
The wrist is slightly flexed to make it easier to insert the arthroscope and arthroscopic instrumentation.
 Small joint instrumentation with a 2.7-mm or smaller arthroscope is used.
Small joint instrumentation with a 2.7-mm or smaller arthroscope is used.
 Small joint shavers are used as well. Large joint instrumentation is not recommended for the wrist.
Small joint shavers are used as well. Large joint instrumentation is not recommended for the wrist.
 A wrist traction tower helps provide traction to the wrist and stabilizes the forearm. If this is not available, the wrist can be suspended in a shoulder traction tower, although the forearm is not stabilized, and the wrist will be at neutral position.
A wrist traction tower helps provide traction to the wrist and stabilizes the forearm. If this is not available, the wrist can be suspended in a shoulder traction tower, although the forearm is not stabilized, and the wrist will be at neutral position.
 Another option, if the traction tower is not available, is to suspend the wrist horizontally over the hand table. Finger traps may be used with a weight placed at the end of the table to help suspend the wrist. This helps stabilize the forearm, but the wrist will be in neutral position for the procedure.
Another option, if the traction tower is not available, is to suspend the wrist horizontally over the hand table. Finger traps may be used with a weight placed at the end of the table to help suspend the wrist. This helps stabilize the forearm, but the wrist will be in neutral position for the procedure.
Exposures
 Inflow is provided through a needle using the 6U portal (Fig. 66-2).
Inflow is provided through a needle using the 6U portal (Fig. 66-2).
 The arthroscope is placed in the 4-5 or 6R portal to look across the wrist to identify the stalk of the ganglion. (Fig. 66-3 shows the arthroscope placed in the 6R portal, and inflow is maintained using the 6U portal.)
The arthroscope is placed in the 4-5 or 6R portal to look across the wrist to identify the stalk of the ganglion. (Fig. 66-3 shows the arthroscope placed in the 6R portal, and inflow is maintained using the 6U portal.)
 The stalk of the ganglion will be identified at the junction of the scapholunate interosseous ligament to the dorsal capsule (Fig. 66-4).
The stalk of the ganglion will be identified at the junction of the scapholunate interosseous ligament to the dorsal capsule (Fig. 66-4).
 An 18-gauge needle is then inserted directly through the back of the ganglion into the radiocarpal space, as viewed arthroscopically with a scope in the 4-5 or 6R portal.
An 18-gauge needle is then inserted directly through the back of the ganglion into the radiocarpal space, as viewed arthroscopically with a scope in the 4-5 or 6R portal.
Pearls
The ganglion cyst is usually located distal to the standard 3-4 portal. Because of this, the needle is at about a 45-degree angle to the dorsum of the hand, which allows it to enter through the cyst and then into the radiocarpal space.
It is occasionally helpful to turn the lights down in the operating room theater; the lights from the arthroscope will transilluminate the sack of the ganglion cyst. This can aid in placing the needle.
Pitfalls
It is important to know the normal structures of the wrist and not to mistake them for pathologic changes.
Wrist arthroscopy portals must be precise. If a portal is off by just 1 to 2 mm, it can potentially cause intra-articular damage to the wrist and significantly impair visualization.
In fractures or in acute trauma, the wrist may be swollen. In this case, it is important to palpate and identify the bony landmarks because the extensor tendons are not palpable.
Procedure
Step 1
 The wrist is suspended in 10 pounds of traction in a traction tower. Inflow is provided through a needle using the 6U portal. (Fig. 66-5 shows the outline of the ganglion marked.) The arthroscope is placed in the 6R portal. A needle is placed through the sac of the ganglion to enter the radiocarpal space.
The wrist is suspended in 10 pounds of traction in a traction tower. Inflow is provided through a needle using the 6U portal. (Fig. 66-5 shows the outline of the ganglion marked.) The arthroscope is placed in the 6R portal. A needle is placed through the sac of the ganglion to enter the radiocarpal space.
 The needle is seen entering the radiocarpal space through the sac of the ganglion with the arthroscope in the 6R portal.
The needle is seen entering the radiocarpal space through the sac of the ganglion with the arthroscope in the 6R portal.
 Notice the oblique path of the needle toward the more distally located ganglion to enter the radiocarpal space. The skin only is incised to make the portal.
Notice the oblique path of the needle toward the more distally located ganglion to enter the radiocarpal space. The skin only is incised to make the portal.
Step 1 Pitfalls
The sac of the ganglion cyst should be outlined with a marking pen before the reduction of the inflow through the 6U portal. This is to help note its location before the wrist becomes swollen from any fluid extravasation.
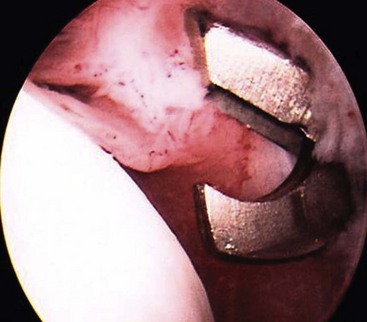
The shaver is introduced through the distal 3-4 portal into the radiocarpal space (Fig. 66-6).
An approximately 1-cm full-thickness defect of the dorsal capsule is then created with the shaver (Fig. 66-7).
This defect is at the junction of the dorsal capsule and the scapholunate interosseous ligament.
A small punch may also be used to create the capsular defect (Fig. 66-8).
Step 2
 The shaver is introduced through the distal 3-4 portal into the radiocarpal space (see Fig. 66-6).
The shaver is introduced through the distal 3-4 portal into the radiocarpal space (see Fig. 66-6).
 An approximately 1-cm full-thickness defect of the dorsal capsule is then created with the shaver (see Fig. 66-7).
An approximately 1-cm full-thickness defect of the dorsal capsule is then created with the shaver (see Fig. 66-7).
 This defect is at the junction of the dorsal capsule and the scapholunate interosseous ligament.
This defect is at the junction of the dorsal capsule and the scapholunate interosseous ligament.
 A small punch may also be used to create the capsular defect (see Fig. 66-8).
A small punch may also be used to create the capsular defect (see Fig. 66-8).
Step 2 Pearls
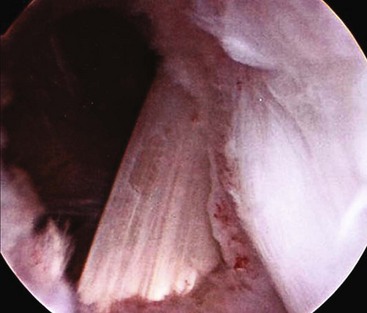
It is important to visualize the dorsal extensor tendons after the full-thickness defect has been created. Once the tendons are seen, this ensures that a full-thickness defect is made.
The tendon usually identified is the extensor carpi radialis brevis, although the tendons of the extensor digitorum communis may be identified as well (Fig. 66-9).
It is sometimes helpful to place the wrist at neutral or in slight extension if it is difficult to visualize in the dorsal capsule at its junction with the scapholunate interosseous ligament. This helps relax the dorsal capsule to improve visualization.
Step 2 Pitfalls
Small joint instrumentation is used. A standard small shaver is not very aggressive compared with its larger counterparts, although it would be difficult, although not impossible, to shave through an entire extensor tendon. Caution is needed.
With a small joint punch, it would similarly be difficult to create a full-thickness defect in the overlying extensor tendons. However, it is important to visualize directly what the shaver or the punch contacts.
As one shaves the dorsal capsule, occasionally fluid from the cyst will be seen entering the joint. This will have a yellow, oily configuration.
Once the defect has been made, it is important to palpate the cyst to confirm that it has been decompressed.
After decompression of the ganglion cyst, the wrist is then evaluated for any additional disease through the radiocarpal and midcarpal portals.