Procedure 65 Arthroscopic Treatment for Septic Arthritis
Indications
 Arthroscopic synovectomy has been shown to be beneficial in patients with symptomatic, refractory reactive arthritis.
Arthroscopic synovectomy has been shown to be beneficial in patients with symptomatic, refractory reactive arthritis.
 Arthroscopy allows for not only continuous irrigation of joint space but also débridement of infected material.
Arthroscopy allows for not only continuous irrigation of joint space but also débridement of infected material.
Examination/Imaging
Clinical Examination
 Examine the entire wrist for swelling, redness, warmth, and pain.
Examine the entire wrist for swelling, redness, warmth, and pain.
 The range-of-motion examination will produce exquisite pain with both active and passive motion.
The range-of-motion examination will produce exquisite pain with both active and passive motion.
 Hematogenous spread will manifest with systemic signs of infection, which may include fever, chills, tachycardia, and diaphoresis.
Hematogenous spread will manifest with systemic signs of infection, which may include fever, chills, tachycardia, and diaphoresis.
 Evaluation with laboratory tests should be done and should include white blood cell count (WBC), erythrocyte sedimentation rate, and C-reactive protein levels.
Evaluation with laboratory tests should be done and should include white blood cell count (WBC), erythrocyte sedimentation rate, and C-reactive protein levels.
 Joint fluid can be obtained at the initiation of the procedure and should be evaluated with Gram staining, culture and sensitivity, WBC count, and crystal analysis.
Joint fluid can be obtained at the initiation of the procedure and should be evaluated with Gram staining, culture and sensitivity, WBC count, and crystal analysis.
Surgical Anatomy
 Structures to be identified and marked are Lister tubercle, articular margins, and the radius and ulna.
Structures to be identified and marked are Lister tubercle, articular margins, and the radius and ulna.
 Tendons that should be identified are the extensor digitorum communis (EDC), the extensor digiti minimi (EDM), and the extensor carpi ulnaris (ECU).
Tendons that should be identified are the extensor digitorum communis (EDC), the extensor digiti minimi (EDM), and the extensor carpi ulnaris (ECU).
 Portal sites 3-4, 4-5, radial and ulna midcarpal, and 6U are marked before starting the procedure.
Portal sites 3-4, 4-5, radial and ulna midcarpal, and 6U are marked before starting the procedure.
Positioning
 A sterile traction tower is used to suspend the elbow flexed at 90 degrees.
A sterile traction tower is used to suspend the elbow flexed at 90 degrees.
 The index and long finger are placed in finger traps, and a 10-lb weight is applied through the traction tower (Fig. 65-1).
The index and long finger are placed in finger traps, and a 10-lb weight is applied through the traction tower (Fig. 65-1).
 A gravity inflow system is used instead of the typical infusion pump system to help decrease the chance of disseminating infected fluid into the surrounding soft tissue structures.
A gravity inflow system is used instead of the typical infusion pump system to help decrease the chance of disseminating infected fluid into the surrounding soft tissue structures.
 An arthroscope, 30-degree angled lens, camera, and full radius joint shaver setup are needed for this procedure.
An arthroscope, 30-degree angled lens, camera, and full radius joint shaver setup are needed for this procedure.
Exposures
 Extremity exsanguination is generally contraindicated because of the joint infection. In some situations a tourniquet may be used to allow better visualization of the wrist joint. If a tourniquet is used, the arm is elevated to let the blood drain before tourniquet inflation.
Extremity exsanguination is generally contraindicated because of the joint infection. In some situations a tourniquet may be used to allow better visualization of the wrist joint. If a tourniquet is used, the arm is elevated to let the blood drain before tourniquet inflation.
 The anatomic landmarks are identified before starting the procedure. The portal sites are then marked, which are the radiocarpal, 3-4, 6R, 6U, and radial and ulna midcarpal portals.
The anatomic landmarks are identified before starting the procedure. The portal sites are then marked, which are the radiocarpal, 3-4, 6R, 6U, and radial and ulna midcarpal portals.
 The 6R portal is located by palpating the ECU tendon. The portal is made just radial to the tendon.
The 6R portal is located by palpating the ECU tendon. The portal is made just radial to the tendon.
 The 3-4 portal is located by palpating the concavity between the extensor pollicis longus and EDC tendons just distal to Lister tubercle in line with the radial border of the long finger (Fig. 65-2).
The 3-4 portal is located by palpating the concavity between the extensor pollicis longus and EDC tendons just distal to Lister tubercle in line with the radial border of the long finger (Fig. 65-2).
 The radial midcarpal portal is located about 1 cm distal to the 3-4 portal, and the ulna midcarpal portal is located about 1 cm distal to the 6R portal in line with the midaxis of the ring finger.
The radial midcarpal portal is located about 1 cm distal to the 3-4 portal, and the ulna midcarpal portal is located about 1 cm distal to the 6R portal in line with the midaxis of the ring finger.
Procedure
Step 1
 Inflow is initially placed through the 6U portal. The joint is inflated.
Inflow is initially placed through the 6U portal. The joint is inflated.
 A skin incision is made with a no. 11 blade scalpel at the 3-4 portal site. Only the skin should be incised, and the blade should be carried distally while the skin is retracted proximally with the thumb.
A skin incision is made with a no. 11 blade scalpel at the 3-4 portal site. Only the skin should be incised, and the blade should be carried distally while the skin is retracted proximally with the thumb.
 A blunt curved hemostat should be used to dissect down to the wrist joint capsule using a spread and push technique. Care should be taken to avoid damaging the dorsal sensory nerves and the superficial veins that run in a longitudinal fashion (Fig. 65-3).
A blunt curved hemostat should be used to dissect down to the wrist joint capsule using a spread and push technique. Care should be taken to avoid damaging the dorsal sensory nerves and the superficial veins that run in a longitudinal fashion (Fig. 65-3).
 To stay parallel to the articular surface, the trocar is angled 10 degrees proximally with respect to the volar inclination.
To stay parallel to the articular surface, the trocar is angled 10 degrees proximally with respect to the volar inclination.
 Entry into the joint capsule should be done in a controlled fashion using gentle pressure on a blunt trocar (Fig. 65-4).
Entry into the joint capsule should be done in a controlled fashion using gentle pressure on a blunt trocar (Fig. 65-4).
Step 1 Pearls
When introducing the blunt trocar, care must be taken not to plunge into the joint space. A controlled entrance is necessary to avoid injury to the internal structures.
The radioscaphocapitate, long radiolunate, triangular fibrocartilage complex, lunotriquetral interosseous ligament, ulnolunate ligament, and ulnotriquetral ligament can all be viewed from the 3-4 portal.
Inflow is provided through the 6U portal and outflow through the arthroscopic cannula. This allows for greater flow of fluid to irrigate the joint (Fig. 65-5).
Step 1 Pitfalls
Inflow through the arthroscope cannula does not provide sufficient irrigation of the joint because of the small space between the arthroscope and the cannula.
Visualization to the synovitis can be initially difficult. Be patient.
Visualization is key. Advance the arthroscope ulnarly near the 6R portal. Insert the shaver and start making room in the joint.
Step 2
 An 18-gauge needle is inserted into the joint under visualization with the arthroscope in the 3-4 portal.
An 18-gauge needle is inserted into the joint under visualization with the arthroscope in the 3-4 portal.
 A skin incision is made with a no. 11 blade scalpel at the 6R portal site. Only the skin should be incised, and the blade should be carried distally while the skin is retracted proximally.
A skin incision is made with a no. 11 blade scalpel at the 6R portal site. Only the skin should be incised, and the blade should be carried distally while the skin is retracted proximally.
 Once again, care should be taken to avoid damaging the superficial sensory nerves and veins when using a curved hemostat to dissect down to the joint capsule.
Once again, care should be taken to avoid damaging the superficial sensory nerves and veins when using a curved hemostat to dissect down to the joint capsule.
 Entry into the joint with a blunt trocar is made in a neutral position, instead of in an angled fashion.
Entry into the joint with a blunt trocar is made in a neutral position, instead of in an angled fashion.
 The 6R portal will be the working portal and will be used for the motorized shaver and suction.
The 6R portal will be the working portal and will be used for the motorized shaver and suction.
Step 3: Radiocarpal Evaluation
 The radiocarpal joint should be examined in a systematic fashion.
The radiocarpal joint should be examined in a systematic fashion.
 Beginning in a radial to ulnar fashion, the articular surfaces of the scaphoid, lunate, and triquetrum should be evaluated. Care should be taken to thoroughly examine the surfaces for cartilage erosion or wear.
Beginning in a radial to ulnar fashion, the articular surfaces of the scaphoid, lunate, and triquetrum should be evaluated. Care should be taken to thoroughly examine the surfaces for cartilage erosion or wear.
 Next, the scapholunate, lunotriquetral, and radiocarpal ligaments should be examined. The ligaments should be carefully evaluated for laxity, step-offs, and tears.
Next, the scapholunate, lunotriquetral, and radiocarpal ligaments should be examined. The ligaments should be carefully evaluated for laxity, step-offs, and tears.
 After evaluating those ligaments, the articular surface of the radius and the TFCC should be evaluated. Attention should be paid to any tears centrally or in the periphery or the articular disk.
After evaluating those ligaments, the articular surface of the radius and the TFCC should be evaluated. Attention should be paid to any tears centrally or in the periphery or the articular disk.
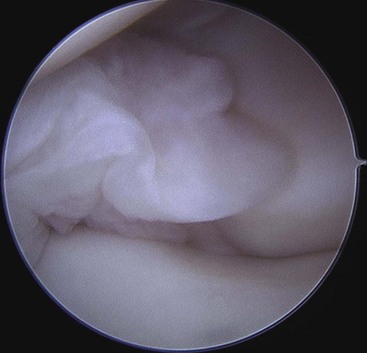
 When synovitis, debris, or loculations are encountered, they should be débrided with the shaver as completely as possible (Fig. 65-6).
When synovitis, debris, or loculations are encountered, they should be débrided with the shaver as completely as possible (Fig. 65-6).
 It is easier to shave the reactive synovitis from the ulnar side of the wrist with the arthroscope in the 3-4 portal and the shaver in the 6R portal.
It is easier to shave the reactive synovitis from the ulnar side of the wrist with the arthroscope in the 3-4 portal and the shaver in the 6R portal.
 The instruments are then reversed, and the radial synovitis is débrided with the shaver in the 3-4 portal and the arthroscope in the 6R portal.
The instruments are then reversed, and the radial synovitis is débrided with the shaver in the 3-4 portal and the arthroscope in the 6R portal.
Step 4: Midcarpal Evaluation
 After the proximal radiocarpal joint space has been thoroughly evaluated, the midcarpal space should be examined.
After the proximal radiocarpal joint space has been thoroughly evaluated, the midcarpal space should be examined.
 The radial midcarpal and ulnar midcarpal portals are accessed in a fashion similar to that of the proximal portals.
The radial midcarpal and ulnar midcarpal portals are accessed in a fashion similar to that of the proximal portals.
 The radial midcarpal portal is used as the visualization portal, and the ulnar midcarpal portal is used as the working portal.
The radial midcarpal portal is used as the visualization portal, and the ulnar midcarpal portal is used as the working portal.
 The distal articular surface of the capitate is easily viewed and should be examined first.
The distal articular surface of the capitate is easily viewed and should be examined first.
 Next, the proximal row bones should be evaluated by inspecting the distal articular surfaces of the scaphoid, lunate, and triquetrum.
Next, the proximal row bones should be evaluated by inspecting the distal articular surfaces of the scaphoid, lunate, and triquetrum.
 The scapholunate and lunotriquetral ligaments and joints are evaluated for laxity, step-offs, tears, or widening.
The scapholunate and lunotriquetral ligaments and joints are evaluated for laxity, step-offs, tears, or widening.
 The Geissler classification system is useful in grading and describing any ligamentous injuries between the proximal row of carpal bones.
The Geissler classification system is useful in grading and describing any ligamentous injuries between the proximal row of carpal bones.
 The ulnar-sided synovitis is débrided with the arthroscope in the radial midcarpal portal and the shaver in the ulna midcarpal portal.
The ulnar-sided synovitis is débrided with the arthroscope in the radial midcarpal portal and the shaver in the ulna midcarpal portal.
 The instruments are then reversed, and the radial synovitis is débrided with the shaver in the radial midcarpal portal and the arthroscope in the ulna midcarpal portal.
The instruments are then reversed, and the radial synovitis is débrided with the shaver in the radial midcarpal portal and the arthroscope in the ulna midcarpal portal.
Postoperative Care and Expected Outcomes
 The skin incision can be either left open or loosely approximated with Steri-Strips.
The skin incision can be either left open or loosely approximated with Steri-Strips.
 The wrist can be placed in a volar resting splint or can be placed in a soft dressing.
The wrist can be placed in a volar resting splint or can be placed in a soft dressing.
 Depending on the clinical scenario, postoperative intravenous antibiotics should be continued and tailored based on the Gram stain and culture and sensitivity results.
Depending on the clinical scenario, postoperative intravenous antibiotics should be continued and tailored based on the Gram stain and culture and sensitivity results.
 Digital range-of-motion exercises are started immediately.
Digital range-of-motion exercises are started immediately.
 Wrist range of motion and strengthening are initiated as tolerated.
Wrist range of motion and strengthening are initiated as tolerated.
Birman MV, Strauch RJ. Management of the septic wrist. J Hand Surg [Am]. 2011;36:324-326.
Goldenberg DL, Brandt KD, Cohen AS, Cathcart ES. Treatment of septic arthritis: comparison of needle aspiration and surgery as initial modes of joint drainage. Arthritis Rheum. 1975;18:83-90.
Sammer D, Shin A. Comparison of arthroscopic and open treatment of septic arthritis of the wrist. J Bone Joint Surg [Am]. 2010;92:107-113.