Procedure 64 Diagnostic Wrist Arthroscopy
![]() See Video 48: Diagnostic Wrist Arthroscopy
See Video 48: Diagnostic Wrist Arthroscopy
Indications
 Patients who have objective mechanical pathology of the wrist
Patients who have objective mechanical pathology of the wrist
Examination/Imaging
Clinical Examination
 Arthroscopy has revolutionized the practice of hand surgery by providing the capability to examine and treat intra-articular abnormalities. Development of wrist arthroscopy is a natural transition from the successful application of arthroscopy of the larger joints. Wrist arthroscopy has seen considerable growth since Whipple reported the original description of the technique he developed for reviewing the intra-articular anatomy of the joints.
Arthroscopy has revolutionized the practice of hand surgery by providing the capability to examine and treat intra-articular abnormalities. Development of wrist arthroscopy is a natural transition from the successful application of arthroscopy of the larger joints. Wrist arthroscopy has seen considerable growth since Whipple reported the original description of the technique he developed for reviewing the intra-articular anatomy of the joints.
 A spectrum of injuries is seen in patients with interosseous ligament tears. The interosseous ligament stretches, partially tears, and develops into a full-thickness tear. Patients with scapholunate instability complain of point tenderness directly over the dorsum of the scapholunate ligament. Swelling may be seen localized in this area, and patients may have a positive Watson maneuver. The latter is performed by pushing the tubercle of the scaphoid dorsally with radial wrist deviation. Patients with lunotriquetral interosseous instability complain of point tenderness directly over the dorsum of the lunotriquetral interval. Patients may have a positive shuck test, in which anterior-posterior translation is felt between the lunate and triquetrum, causing point tenderness. A squeeze test consists of radial ulnar compression of the wrist between the thumb and index finger of the examiner. Patients with lunotriquetral instability will complain of pain at the lunotriquetral interval.
A spectrum of injuries is seen in patients with interosseous ligament tears. The interosseous ligament stretches, partially tears, and develops into a full-thickness tear. Patients with scapholunate instability complain of point tenderness directly over the dorsum of the scapholunate ligament. Swelling may be seen localized in this area, and patients may have a positive Watson maneuver. The latter is performed by pushing the tubercle of the scaphoid dorsally with radial wrist deviation. Patients with lunotriquetral interosseous instability complain of point tenderness directly over the dorsum of the lunotriquetral interval. Patients may have a positive shuck test, in which anterior-posterior translation is felt between the lunate and triquetrum, causing point tenderness. A squeeze test consists of radial ulnar compression of the wrist between the thumb and index finger of the examiner. Patients with lunotriquetral instability will complain of pain at the lunotriquetral interval.
 Patients with injury to the TFCC complain of pain at the head of the ulna or the prestyloid recess.
Patients with injury to the TFCC complain of pain at the head of the ulna or the prestyloid recess.
 Patients with fractures of the scaphoid are tender in the snuffbox.
Patients with fractures of the scaphoid are tender in the snuffbox.
 Patients with fractures of the distal radius have generalized swelling around the wrist and are tender to palpation over the distal radius.
Patients with fractures of the distal radius have generalized swelling around the wrist and are tender to palpation over the distal radius.
Imaging
 Multiview radiographs of the wrist on posterior-anterior and lateral planes are mandatory to evaluate for intra-articular pathology.
Multiview radiographs of the wrist on posterior-anterior and lateral planes are mandatory to evaluate for intra-articular pathology.
 Partial tears of the interosseous ligaments are rarely detected on plain radiographs, although dynamic instability may be identified on plain radiographs with dynamic views. Magnetic resonance imaging (MRI) has improved in detecting interosseous injuries. If interosseous ligament injuries are suspected, MRI arthrography is strongly recommended over MRI imaging alone to increase the accuracy of detecting interosseous ligament injuries.
Partial tears of the interosseous ligaments are rarely detected on plain radiographs, although dynamic instability may be identified on plain radiographs with dynamic views. Magnetic resonance imaging (MRI) has improved in detecting interosseous injuries. If interosseous ligament injuries are suspected, MRI arthrography is strongly recommended over MRI imaging alone to increase the accuracy of detecting interosseous ligament injuries.
 Patients with ulnar abutment and central tears of the TFCC can be identified on plain radiographs for patients with a markedly positive ulnar wrist in neutral rotation on radiography.
Patients with ulnar abutment and central tears of the TFCC can be identified on plain radiographs for patients with a markedly positive ulnar wrist in neutral rotation on radiography.
Surgical Anatomy
 The wrist is the labyrinth of eight carpal bones. Multiple articular surfaces with intrinsic and extrinsic ligaments and the TFCC form a perplexing joint that continuously challenges physicians with an array of diagnoses. Wrist arthroscopy allows direct visualization of the cartilage surfaces, carpal bones, and ligaments using bright light and magnification.
The wrist is the labyrinth of eight carpal bones. Multiple articular surfaces with intrinsic and extrinsic ligaments and the TFCC form a perplexing joint that continuously challenges physicians with an array of diagnoses. Wrist arthroscopy allows direct visualization of the cartilage surfaces, carpal bones, and ligaments using bright light and magnification.
 The scapholunate interosseous ligament is best seen with the arthroscope in the 3-4 portal. The lunotriquetral interval is best seen with the arthroscope in the 4-5 or 6R portals owing to its more distal location. The scapholunate interval as seen from the midcarpal space should be tight and congruent. There should be no step-off or separation. The lunotriquetral interval may have slight play between the lunate and the triquetrum. An approximately 1-mm distal step-off of the triquetrum may be seen.
The scapholunate interosseous ligament is best seen with the arthroscope in the 3-4 portal. The lunotriquetral interval is best seen with the arthroscope in the 4-5 or 6R portals owing to its more distal location. The scapholunate interval as seen from the midcarpal space should be tight and congruent. There should be no step-off or separation. The lunotriquetral interval may have slight play between the lunate and the triquetrum. An approximately 1-mm distal step-off of the triquetrum may be seen.
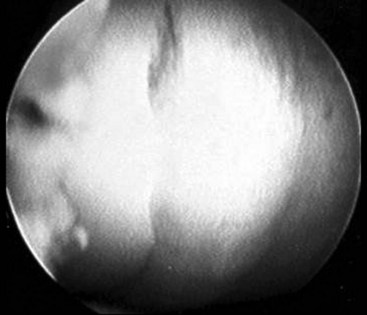
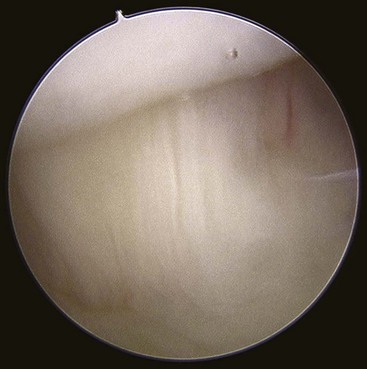
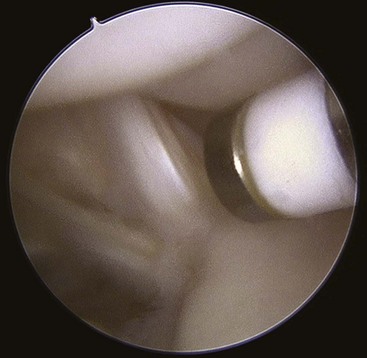
 Geissler defined an arthroscopic classification for interosseous ligament injury. A spectrum of injury is seen throughout this ligament. The ligament stretches and then tears, usually in a volar to dorsal direction. This arthroscopic classification is based on evaluation of the interosseous ligament from both the radiocarpal and midcarpal spaces. (Fig. 64-1 shows arthroscopic view of a normal scapholunate ligament.)
Geissler defined an arthroscopic classification for interosseous ligament injury. A spectrum of injury is seen throughout this ligament. The ligament stretches and then tears, usually in a volar to dorsal direction. This arthroscopic classification is based on evaluation of the interosseous ligament from both the radiocarpal and midcarpal spaces. (Fig. 64-1 shows arthroscopic view of a normal scapholunate ligament.)
Exposures
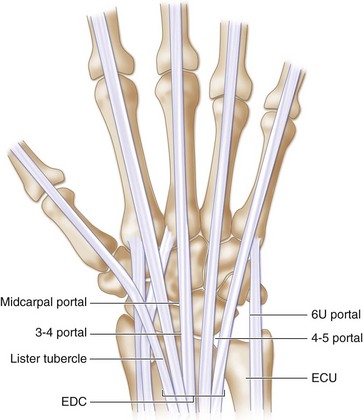
 Wrist arthroscopy portals are made according to the space to which they correspond with respect to the extensor compartments (Fig. 64-6).
Wrist arthroscopy portals are made according to the space to which they correspond with respect to the extensor compartments (Fig. 64-6).
 The traditional portal is the 3-4 portal. This portal is made between the third and fourth dorsal compartments of the wrist. The 3-4 portal is located by palpating Lister tubercle by advancing the finger about 1 cm distal until the soft spot is noted over the dorsal lip of the radius. The 3-4 portal is in line with the radial border of the long finger. (Fig. 64-7 shows the thumb being used to palpate between the third and fourth dorsal compartments to identify the 3-4 portal space.) When the wrist is injected with arthroscopy fluid from the 6U portal, a bubble of swelling is typically noted over the 3-4 portal region. This further helps locate the 3-4 portal.
The traditional portal is the 3-4 portal. This portal is made between the third and fourth dorsal compartments of the wrist. The 3-4 portal is located by palpating Lister tubercle by advancing the finger about 1 cm distal until the soft spot is noted over the dorsal lip of the radius. The 3-4 portal is in line with the radial border of the long finger. (Fig. 64-7 shows the thumb being used to palpate between the third and fourth dorsal compartments to identify the 3-4 portal space.) When the wrist is injected with arthroscopy fluid from the 6U portal, a bubble of swelling is typically noted over the 3-4 portal region. This further helps locate the 3-4 portal.
 The 4-5 portal is located by rolling the finger over the palpable fourth compartment and then finding the soft spot opposite the 3-4 portal on the ulnar aspect of the fourth compartment. As a general rule, the 4-5 portal lies slightly more proximal than the 3-4 portal because of the radial inclination of the distal radius. The 4-5 portal is a typical working portal that is in line with the midaxis of the ring metacarpal.
The 4-5 portal is located by rolling the finger over the palpable fourth compartment and then finding the soft spot opposite the 3-4 portal on the ulnar aspect of the fourth compartment. As a general rule, the 4-5 portal lies slightly more proximal than the 3-4 portal because of the radial inclination of the distal radius. The 4-5 portal is a typical working portal that is in line with the midaxis of the ring metacarpal.
 The 6R and 6U portals are named according to their positions relative to the extensor carpi ulnaris tendon, with the 6R portal being radial and the 6U portal being ulnar to the tendon. The 6R portal is a typical working portal, and the 6U portal is typically used for inflow of fluid into the wrist. (Fig. 64-8 shows inflow through 6U, 6R being used as a working portal, and 3-4 being used as the arthroscope portal.)
The 6R and 6U portals are named according to their positions relative to the extensor carpi ulnaris tendon, with the 6R portal being radial and the 6U portal being ulnar to the tendon. The 6R portal is a typical working portal, and the 6U portal is typically used for inflow of fluid into the wrist. (Fig. 64-8 shows inflow through 6U, 6R being used as a working portal, and 3-4 being used as the arthroscope portal.)
 The 1-2 portal is made along the dorsal aspect of the snuffbox. By making this portal along the dorsal aspect, it prevents injury to the radial artery.
The 1-2 portal is made along the dorsal aspect of the snuffbox. By making this portal along the dorsal aspect, it prevents injury to the radial artery.
 The radial midcarpal portal is made 1 cm distal to the 3-4 portal. This portal gives good visualization of the midcarpal space. The ulnar midcarpal portal is made 1 cm distal to the 4-5 portal. Typically, there is more room in the ulnar midcarpal portal than the radial midcarpal portal. If the surgeon has difficulty entering the midcarpal space in the radial midcarpal portal, the ulnar midcarpal portal should be used because it has easier access.
The radial midcarpal portal is made 1 cm distal to the 3-4 portal. This portal gives good visualization of the midcarpal space. The ulnar midcarpal portal is made 1 cm distal to the 4-5 portal. Typically, there is more room in the ulnar midcarpal portal than the radial midcarpal portal. If the surgeon has difficulty entering the midcarpal space in the radial midcarpal portal, the ulnar midcarpal portal should be used because it has easier access.
 The STT portal is made just ulnar to the EPL tendon. This portal is best made with the arthroscope in the radial midcarpal portal, and a spinal needle is used to identify the exact location.
The STT portal is made just ulnar to the EPL tendon. This portal is best made with the arthroscope in the radial midcarpal portal, and a spinal needle is used to identify the exact location.
Pearls
The key to making a wrist arthroscopy portal is to pull the skin against the tip of a no. 11 blade. Blunt dissection is then carried down to the level of the joint capsule. The arthroscope is introduced with a blunt trocar to avoid injury to the articular cartilage. (Fig. 64-9 shows blunt tip of arthroscope trocar.) Before committing to a skin incision, an 18-gauge needle is used to identify the exact location of the portal. If the portal location is too proximal or distal, the needle will not pass freely into the joint. (Fig. 64-10 shows an 18-gauge needle being used to help identify the correct place for the 3-4 portal.)
Keep in mind the slope of the distal radius and the radial inclination. The initial needle, as it is passed into the joint, should have about a 10-degree tilt from dorsal to volar to parallel the slope of the distal radius.
The 4-5 and 6R portals should be slightly proximal to the 3-4 portals following the inclination of the distal radius.
Both the radiocarpal and midcarpal spaces should be evaluated when wrist arthroscopy is performed.
Occasionally, dry arthroscopy is performed. In this manner, the arthroscope is introduced into the radiocarpal space without irrigation fluid. This is done to confirm a preoperative diagnosis in which the operative plan is eventually to open the wrist joint. In this manner, fluid extravasation into the soft tissues is limited, and the anatomy is not distorted.
Pitfalls
It is important to know the normal structures of the wrist and not to mistake them for pathologic changes.
Wrist arthroscopy portals must be precise. If a portal is off by just 1 to 2 mm, it can potentially cause intra-articular damage to the wrist and significantly impair visualization.
In fractures or in acute trauma, the wrist may be swollen. In this manner, it is important to palpate and identify the bony landmarks because the extensor tendons would not be palpable.
Procedure
Step 1
 The wrist is suspended with about 10 pounds of traction in a traction tower (Fig. 64-11).
The wrist is suspended with about 10 pounds of traction in a traction tower (Fig. 64-11).
 Slight flexion of the wrist makes it easier for entry for the arthroscopic instrumentation.
Slight flexion of the wrist makes it easier for entry for the arthroscopic instrumentation.
 Traction is provided through finger traps to the index and long fingers (see Fig. 64-12).
Traction is provided through finger traps to the index and long fingers (see Fig. 64-12).
Step 1 Pearls
Towels are placed under the arm and forearm between the tower and the patient. This helps to avoid any potential abrasion of the skin from the metal traction tower (Fig. 64-12).
If a traction tower is not available, the wrist may be suspended overhead through finger traps and a shoulder traction apparatus.
If this is not available, the wrist may be placed in a horizontal position with finger traps and weights hanging over the end of the hand table.
Step 1 Pitfalls
It is important to assess the temperature of the traction tower before wrist arthroscopy. If the tower has been used repeatedly, it may become very hot because it is sterilized and potentially can burn the patient.
If the traction tower apparatus is hot, it can be cooled off by placing it in a basin filled with irrigation fluid.
Step 2
 Inflow can be provided either through the 6U portal or through the arthroscopic cannula.
Inflow can be provided either through the 6U portal or through the arthroscopic cannula.
 Because of the small size of the arthroscopic cannula, it is recommended that inflow be provided through a separate inflow portal such as 6U.
Because of the small size of the arthroscopic cannula, it is recommended that inflow be provided through a separate inflow portal such as 6U.
 Outflow is provided through the arthroscopic cannula.
Outflow is provided through the arthroscopic cannula.
 An additional viewing portal is the 3-4 portal. The working portal is traditionally the 4-5 or 6R.
An additional viewing portal is the 3-4 portal. The working portal is traditionally the 4-5 or 6R.
Step 2 Pearls
The 3-4 portal is most easily identified by rolling the tip of the thumb fingernail over the dorsal lip of the distal radius.
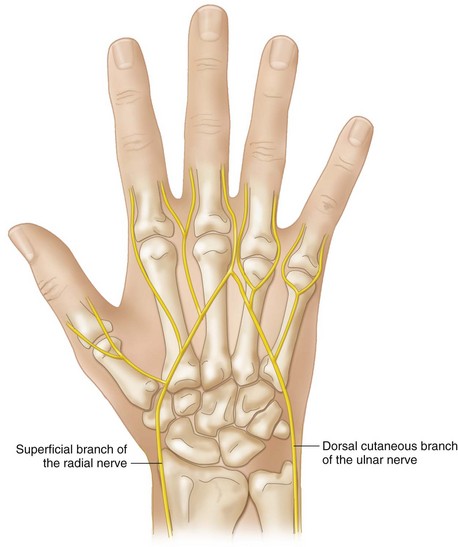
Arthroscopy portals may be made in the horizontal or longitudinal direction depending on the surgeon’s preference. A horizontal incision may be potentially more cosmetic, although it may have a high risk for injury to the extensor tendons or dorsal cutaneous nerves. It is important not to insert the knife blade too deeply to avoid injury to these structures.
Outflow of fluid is through the irrigation tubing connected to the arthroscopic cannula. The irrigation tubing is placed into a basin so that the irrigation fluid does not run out on the operative field or into the surgeon’s lap.
Step 3
 The radiocarpal space is evaluated in a radial to ulnar direction. The extrinsic radioscaphocapitate ligament is seen most radially along its insertion on the radial styloid, and the long radial lunate ligament, which is slightly wider, is just ulnar. (Fig. 64-13 shows the radioscaphocapitate and long radiolunate ligaments.)
The radiocarpal space is evaluated in a radial to ulnar direction. The extrinsic radioscaphocapitate ligament is seen most radially along its insertion on the radial styloid, and the long radial lunate ligament, which is slightly wider, is just ulnar. (Fig. 64-13 shows the radioscaphocapitate and long radiolunate ligaments.)
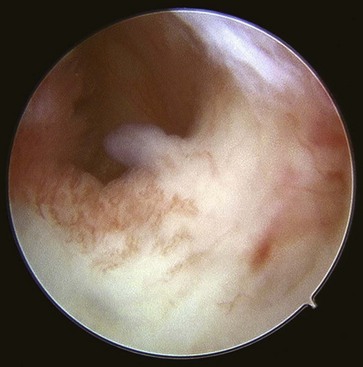
 The radioscapholunate ligament (ligament of Testut) is next seen ulnarly. This is primarily a neurovascular structure (Fig. 64-14).
The radioscapholunate ligament (ligament of Testut) is next seen ulnarly. This is primarily a neurovascular structure (Fig. 64-14).
 The articular disk is identified ulnarly and palpated with a probe in the 6R portal.
The articular disk is identified ulnarly and palpated with a probe in the 6R portal.
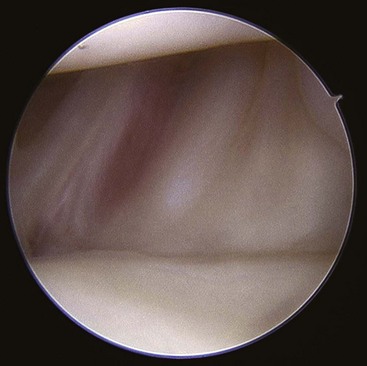
 The ulnar triquetral and ulnar lunate ligaments are best seen with the arthroscope in the 6R portal. (Fig. 64-15 shows the ulnar triquetral ligament.)
The ulnar triquetral and ulnar lunate ligaments are best seen with the arthroscope in the 6R portal. (Fig. 64-15 shows the ulnar triquetral ligament.)
 The lunotriquetral interosseous ligament is best identified with the arthroscope in the 6R portal.
The lunotriquetral interosseous ligament is best identified with the arthroscope in the 6R portal.
Step 3 Pitfalls
The prestyloid recess is viewed arthroscopically as a normal fovea. Do not confuse a peripheral tear to the articular disk with this normal fovea. (Fig. 64-16 shows the prestyloid recess.) A peripheral tear of the TFCC disk usually is dorsal to the fovea.
The pisiform is seen about 60% of the time in normal wrist arthroscopy. This is a normal finding. Do not confuse a normal finding with pathologic changes of the wrist.
Step 4
 A needle is placed in the proposed ideal location for the radial midcarpal portal following diagnostic examination to the radiocarpal space.
A needle is placed in the proposed ideal location for the radial midcarpal portal following diagnostic examination to the radiocarpal space.
 If a free flow of fluid is seen with the inflow through the 6U portal and the needle in the midcarpal space, one should be concerned about an interosseous ligament tear.
If a free flow of fluid is seen with the inflow through the 6U portal and the needle in the midcarpal space, one should be concerned about an interosseous ligament tear.
 The radial midcarpal portal is made after its ideal location is identified with a spinal needle.
The radial midcarpal portal is made after its ideal location is identified with a spinal needle.
 The ulnar midcarpal portal is made by placing a needle into the proposed location under direct visualization with the arthroscope in the radial midcarpal portal.
The ulnar midcarpal portal is made by placing a needle into the proposed location under direct visualization with the arthroscope in the radial midcarpal portal.
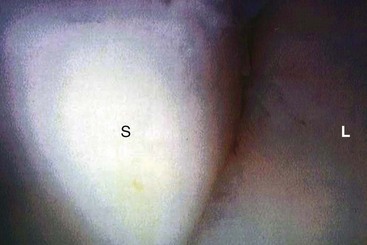
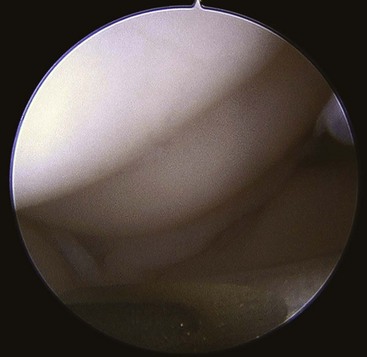
 Any widening or step-off of the scapholunate or lunotriquetral interosseous ligaments is best judged with the arthroscope in the midcarpal portal. (Fig. 64-17 shows midcarpal view of scapholunate ligament, Fig. 64-18 shows normal lunotriquetral interface, and Fig. 64-19 shows abnormal widening at lunotriquetral interface.)
Any widening or step-off of the scapholunate or lunotriquetral interosseous ligaments is best judged with the arthroscope in the midcarpal portal. (Fig. 64-17 shows midcarpal view of scapholunate ligament, Fig. 64-18 shows normal lunotriquetral interface, and Fig. 64-19 shows abnormal widening at lunotriquetral interface.)
 Articular cartilage defects, particularly of the capitate or hamate, are evaluated. (Fig. 64-20 shows arthroscopic view of the capitate and hamate interface.)
Articular cartilage defects, particularly of the capitate or hamate, are evaluated. (Fig. 64-20 shows arthroscopic view of the capitate and hamate interface.)
 These articular cartilage defects are more common in patients with a type II lunate.
These articular cartilage defects are more common in patients with a type II lunate.
 Fractures of the scaphoid are best seen with the arthroscope in the midcarpal space. Fractures of the proximal pole are best visualized with the arthroscope in the ulnar midcarpal portal, and fractures of the waist of the scaphoid are best seen with the arthroscope in the radial midcarpal portal.
Fractures of the scaphoid are best seen with the arthroscope in the midcarpal space. Fractures of the proximal pole are best visualized with the arthroscope in the ulnar midcarpal portal, and fractures of the waist of the scaphoid are best seen with the arthroscope in the radial midcarpal portal.
Step 4 Pearls
When inserting Kirschner wires for provisional fixation of a fracture or pinning acute interosseous ligament injuries, insert the wires in oscillation mode to minimize injury to the cutaneous nerves (Fig. 64-21).
If electrothermal shrinkage is being performed, it is important to monitor the temperature of the wrist arthroscopy fluid as it exits the wrist. The wrist is an extremely small joint, and the fluid can rapidly heat up with a thermal shrinkage probe causing potential burns to the wrist. (Fig. 64-22 shows use of electrothermal shrinkage.)
Postoperative Care and Expected Outcomes
 Postoperative care varies depending on the arthroscopic procedure performed. With traditional and diagnostic wrist arthroscopy, the patient keeps the wounds dry for about 3 days. Showers, not baths, are encouraged for the next 10 days to 2 weeks until the portals seal.
Postoperative care varies depending on the arthroscopic procedure performed. With traditional and diagnostic wrist arthroscopy, the patient keeps the wounds dry for about 3 days. Showers, not baths, are encouraged for the next 10 days to 2 weeks until the portals seal.
 Patients start range of motion of the fingers initially and progress to motion of the wrist and strengthening as tolerated.
Patients start range of motion of the fingers initially and progress to motion of the wrist and strengthening as tolerated.
Chung KC, Zimmerman NB, Travis MT. Wrist arthrography versus arthroscopy: a comparative study of 150 cases. J Hand Surg [Am]. 1996;21:591-594.
Geissler WB, Freeland AE, Weiss APC, Chow JCY. Techniques of wrist arthroscopy. J Bone Joint Surg [Am]. 1999;81:1184-1197.
Johnstone DJ, Thorogood S, Smith WH, Scott TD. A comparison of magnetic resonance imaging and arthroscopy in the investigation of chronic wrist pain. J Hand Surg [Br]. 1997;22:714-718.