CHAPTER 64
Baker Cyst
Darren Rosenberg, DO; Joao E.D. Amadera, MD, PhD
Definition
Baker cyst, the most common cyst in the posterior knee, was first described more than a century and a half ago by Adams [1] and later by Baker [2]. It affects approximately 19% of asymptomatic adults (especially adults older than 50 years) [3] and 6.3% of children [4]. It is more common in boys and in children with arthritic knees or hypermobility syndrome [5]. Two age incidence peaks exist: 4 to 7 years and 35 to 70 years [6,7]. Three factors are key to the formation of Baker cyst: (1) communication between the knee joint and popliteal bursae, (2) one-way valve effect, and (3) unequal pressure between the joint and bursae during varying angles of knee movement [7].
Chronic irritation in the knee joint may increase production of synovial fluid, which may flow from the knee joint into the bursae under higher intra-articular pressure until the one-way valve formed by the gastrocnemius-soleus complex “closes,” trapping the fluid in one of the popliteal bursae. This bursa then distends and forms a palpable mass, more commonly in the posteromedial aspect of the popliteal fossa [8]. Anatomically, the lack of supporting structures in this area may predispose this region of the popliteal space to cyst formation [8]. Most commonly, the source of this chronic irritation is an inflammatory or degenerative joint disease, such as rheumatoid arthritis or osteoarthritis. Furthermore, conditions like infectious arthritis, polyarthritis, villonodular synovitis, connective tissue diseases, chondromalacia patellae, and persistent capsulitis are also commonly associated with Baker cysts [9,10]. In a study of 40 patients with radiographic evidence of primary osteoarthritis of the knee, 22% had Baker cyst diagnosed by ultrasonography [11]. Popliteal cysts are associated with meniscal tears in 71% to 82% of the cases, anterior cruciate ligament insufficiency in 30%, and degenerative cartilage lesions in 30% to 60% of the cases [9,10]. Noncommunicating cysts are rare in adults, often have no associated knee disease, and may be primary bursal enlargements from repeated trauma to the bursa itself related to muscle activation. Direct trauma is the most common cause of these cysts in children [4].
Symptoms
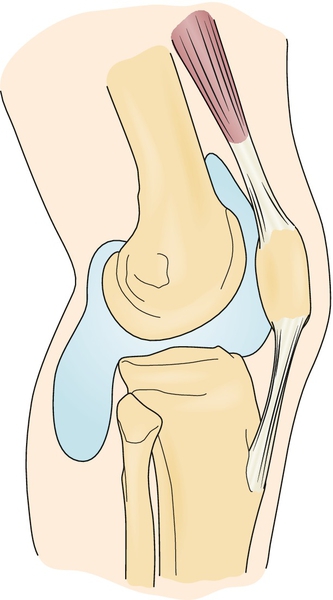
Baker cysts are often nonpainful and may be manifested as a fluctuant mass in the popliteal fossa (Fig. 64.1). Typical symptoms, if present, include swelling, pain, and stiffness exacerbated by activity such as walking. Symptoms are most readily elicited when knee flexion compresses the fluid-filled cyst, although knee extension may also cause tension on the cyst by the extended gastrocnemius-soleus muscles. The mass is often accompanied by leg swelling or diffuse calf tenderness. Numbness and tingling in the posterior aspect of the calf and plantar aspect of the foot may be present if there is neural or vascular involvement.
Physical Examination
Baker cysts are often visible or at least palpable along the medial aspect of the popliteal fossa. The cyst may be identified with the patient prone with the knee first extended and then flexed while the popliteal fossa is inspected and palpated. The round, smooth, fluctuant, and often tender cyst will be firm on palpation with knee extension and may soften or disappear with 45 degrees of knee flexion, a phenomenon known as Foucher sign [12]. The cyst can extend into the thigh or leg, or it can have multiple satellites along the calf and even into the foot. These satellite cysts may or may not be connected to the primary cyst through channels. When a joint effusion accompanies the cyst, it is worthwhile to search for the source of chronic irritation. Examine the knee’s range of motion, test for ligamentous laxity, and evaluate for potential patellofemoral pain and meniscal tears [9]. Furthermore, because of the proximity of the sciatic nerve and its branches to the popliteal region where cysts may be present, in rare cases nerve compression may be manifested as decreased sensation along the plantar aspect of the foot and muscle atrophy in the tibialis posterior, flexor digitorum longus, and flexor hallucis longus [13–15].
Functional Limitations
The degree of impairment produced by the cyst depends on its size and amount of tenderness. Baker cysts are usually painless and limit movement minimally, if at all, unless there is an underlying meniscal injury. However, larger cysts may be associated with moderate limitations in physical activity, particularly walking.
Diagnostic Studies
Plain films of the knee can be used to diagnose underlying degenerative joint disease but are rarely necessary to diagnose Baker cyst. Ultrasonography distinguishes solid from cystic masses and is therefore especially helpful in detecting Baker cysts when extensive joint deformities, such as those present with rheumatoid arthritis, obscure the cyst [16]. Furthermore, ultrasonography is an economical and helpful method of differentiating thrombophlebitis from Baker cysts if there is diagnostic uncertainty. Arthrography, through the injection of contrast dye into the knee joint or bursa, may clearly demonstrate the enlarged bursal structure. In addition, computed tomography may differentiate cysts from lipomas and malignant neoplasms and may show noncommunicating cysts or cysts that are not in the typical locations. Magnetic resonance imaging outlines the anatomy of the entire joint and is a sensitive test to identify Baker cyst as well as its likely cause. Magnetic resonance imaging also helps in ruling out suspected solid tumors and defining pathologic changes for possible surgical excision. On magnetic resonance imaging, Baker cysts appear as well-circumscribed masses with low signal intensity on T1-weighted images and high signal intensity on T2-weighted images (Fig. 64.2). Ultrasonography and magnetic resonance imaging are the two most common radiologic methods for evaluation of suspected Baker cysts, each with its strengths and drawbacks [17]. Testing of the erythrocyte sedimentation rate may also be helpful if an inflammatory process is suspected. In cases in which there is doubt about the cyst’s etiology, analysis and culture of aspirated fluid can help differentiate between infectious, inflammatory, and mechanical processes.

Treatment
Initial
Intervention is needed only when a Baker cyst is symptomatic. The simplest treatment is to aspirate the fluid because aspiration collapses the cyst, and the symptoms consequently disappear. However, treatment of the cyst alone may not be adequate, and treatment of the underlying joint disease may be necessary. Ice and anti-inflammatory agents (nonsteroidal anti-inflammatory drugs) can reduce the inflammatory effusions produced by degenerative joint disease. Quadriceps strengthening exercises can be used for an associated patellofemoral syndrome. In some cases, venous sclerosants are used to prevent recurrence [12]. The cysts tend to involute spontaneously in children.
Rehabilitation
Rehabilitation may include compression and range of motion exercises as a means of decreasing swelling in addition to physical modalities (such as ice) and pharmacotherapy (such as nonsteroidal anti-inflammatory drugs, mentioned before). Furthermore, in cases of degenerative joint disease, cruciate ligament tears, and meniscal injuries, resistance exercises to maintain and to improve lower extremity muscle strength may be helpful. A comprehensive rehabilitation program may lead to progress in gait and in function to perform daily activities.
Procedures
Needle aspiration of the cyst is the most effective therapy, and provided the predisposing cause of the cyst resolves, it generally results in improvement of symptoms and function. Furthermore, if knee joint effusion is present, joint aspiration, accompanied by intra-articular corticosteroid injection, may be beneficial. In cases of noncommunicating cysts, corticosteroid injection directly into the cyst may help decrease swelling. The effect of this intervention may be followed serially through ultrasonography [18]. On the other hand, there is evidence that direct cyst infiltration with steroids has better results in patients with knee osteoarthritis compared with intra-articular injection [19]. The possibility of a vascular malformation must be eliminated either by auscultation of the mass with a stethoscope to listen for bruits or by palpation of it to feel for a pulse before cyst aspiration [20]. In addition, imaging techniques such as ultrasonography may assist in detecting cysts.
Surgery
Surgical excision is attempted only after all other methods have failed and the cyst is sufficiently large and remains symptomatic [21]. In the past, open excision was an option if the cyst remained symptomatic, but the associated recurrence rate was high (up to 63%) [22]. On occasion, surgery was necessary to correct the underlying pathologic process (e.g., arthroscopic surgery for meniscal tears or total knee replacement for intractable degenerative joint disease). Because of that, arthroscopic treatment of popliteal cysts has been the current option. Recently, the arthroscopic approach has been used to simultaneously correct both the valvular opening, by reestablishing a normal bidirectional communication, and the associated intra-articular disease responsible for the persistence of the cyst. Also, large open wounds can be avoided [23,24].
Potential Disease Complications
The most common complications of Baker cysts are dissection into the calf and rupture, leading to calf, ankle, and foot ecchymoses [12]. When the cyst ruptures, it produces a “pseudothrombophlebitis syndrome,” meaning that it results in intense calf pain and swelling without associated deep venous thrombosis. Less commonly, Baker cyst produces compartment syndrome [25], peripheral neuropathy [13,14], or lower extremity claudication [26]. Rarely, if the cyst is infected, it can result in septic arthritis of the knee if an intra-articular–bursal communication exists [27]. Moreover, a possible sequela of Baker cysts may be intramuscular dissection, both distally [28] and less commonly proximally [29].
Potential Treatment Complications
Analgesics and nonsteroidal anti-inflammatory drugs have well-known side effects that most commonly affect the gastric, hepatic, and renal systems. Aspiration can result in recurrence, infection, bleeding, and neurovascular compromise. Surgery can result in local neurovascular complications and recurrence of the cysts [22,30].







