CASE 63

History: No patient history is available.
1. Which should be included in the differential diagnosis for pericardial thickening? (Choose all that apply.)
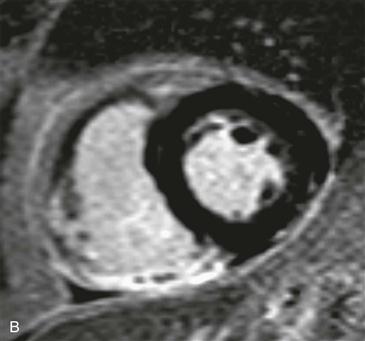
2. What sequence and imaging plane are shown in Fig. A?
A. Inversion recovery late gadolinium enhancement MRI, short-axis view
B. Inversion recovery late gadolinium enhancement MRI, four-chamber view
C. Cine steady-state free precession (SSFP), short-axis view
D. Cine SSFP, four-chamber view
3. Which of the following is a postcardiac injury syndrome?
D. Hypoplastic left heart syndrome
4. What would be the most likely presentation for this patient?
ANSWERS
Reference
Wessman DE, Stafford CM. The postcardiac injury syndrome: case report and review of the literature. South Med J. 2006;99(3):309–314.
Cross-Reference
Cardiac Imaging: The REQUISITES, ed 3, pp 267, 272.
Comment
Epidemiology
Postcardiac injury syndromes can be seen after myocardial infarction, cardiac surgery, percutaneous intervention, radiofrequency ablation, and pacemaker insertion. Dressler syndrome occurs days to months after myocardial infarction and is thought to be an autoantibody response to normal cardiac tissue exposed after the insult. At the present time, Dressler syndrome occurs in less than 1% of patients after myocardial infarction. This decreased incidence is thought to be due to earlier reperfusion and the antiinflammatory effects of cardiac drugs given after myocardial infarction.
Imaging Findings and Treatment
Advanced imaging is infrequently performed to diagnose this condition. The most common finding is pericardial thickening with enhancement (Figs. A and B). Additional findings associated with Dressler syndrome include exudative pericardial and pleural effusions. The prognosis is good because patients respond favorably to nonsteroidal antiinflammatory drugs (NSAIDs) and corticosteroids. Feared complications of postcardiac injury syndromes are graft occlusion after coronary artery bypass graft surgery and hemorrhagic cardiac tamponade in the setting of anticoagulation therapy. One small study showed that NSAIDs, corticosteroids, and aspirin reduced the risk of graft occlusion from 86% to 16%.