Procedure 62 Trapeziectomy and Abductor Pollicis Longus Suspensionplasty
![]() See Video 46: Abductor Pollicis Longus Suspension Arthroplasty for Basal Joint Arthritis
See Video 46: Abductor Pollicis Longus Suspension Arthroplasty for Basal Joint Arthritis
Examination/Imaging
Clinical Examination
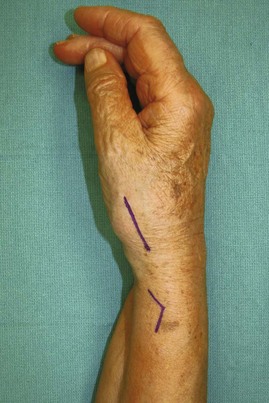
 The patient’s thumb metacarpal base may exhibit a dorsoradial prominence secondary to subluxation from ligamentous laxity (Fig. 62-1).
The patient’s thumb metacarpal base may exhibit a dorsoradial prominence secondary to subluxation from ligamentous laxity (Fig. 62-1).
 The patient’s thumb should be evaluated for tenderness along the TMC joint.
The patient’s thumb should be evaluated for tenderness along the TMC joint.
 The carpometacarpal (CMC) grind test is performed with axial compression, flexion, extension, and circumduction of the TMC joint, which should elicit crepitus and pain.
The carpometacarpal (CMC) grind test is performed with axial compression, flexion, extension, and circumduction of the TMC joint, which should elicit crepitus and pain.
 The patient’s thumb metacarpophalangeal (MCP) joint should be assessed during pinch for hyperextensibility. If unaddressed, the suspensionplasty will be stressed by obligatory metacarpal adduction. This hyperextensibility can be corrected with MCP joint capsulodesis or fusion if the deformity is severe.
The patient’s thumb metacarpophalangeal (MCP) joint should be assessed during pinch for hyperextensibility. If unaddressed, the suspensionplasty will be stressed by obligatory metacarpal adduction. This hyperextensibility can be corrected with MCP joint capsulodesis or fusion if the deformity is severe.
 The patient should be evaluated for carpal tunnel syndrome, which may coexist in up to 43% of patients with TMC arthritis. Concomitant carpal tunnel release should be performed in these patients because trapeziectomy alone does not sufficiently increase carpal tunnel volume.
The patient should be evaluated for carpal tunnel syndrome, which may coexist in up to 43% of patients with TMC arthritis. Concomitant carpal tunnel release should be performed in these patients because trapeziectomy alone does not sufficiently increase carpal tunnel volume.
 An Allen test should be performed because the procedure typically requires mobilization of and potential injury to the radial artery.
An Allen test should be performed because the procedure typically requires mobilization of and potential injury to the radial artery.
 The patient should also be evaluated for concomitant trigger thumb.
The patient should also be evaluated for concomitant trigger thumb.
Imaging
 Posteroanterior, oblique, and lateral radiographs of the hand should be obtained to evaluate the extent of arthritis, osteophyte formation, joint loss, and joint subluxation (Fig. 62-2A to C).
Posteroanterior, oblique, and lateral radiographs of the hand should be obtained to evaluate the extent of arthritis, osteophyte formation, joint loss, and joint subluxation (Fig. 62-2A to C).
 The Eaton classification is a staging system based on radiographic findings only and often does not correlate with the patient’s symptoms. Some patients with severe arthritis may have minimal pain. Treatment should be based on the patient’s symptoms and, most important, on the amount of pain in the arthritic joint.
The Eaton classification is a staging system based on radiographic findings only and often does not correlate with the patient’s symptoms. Some patients with severe arthritis may have minimal pain. Treatment should be based on the patient’s symptoms and, most important, on the amount of pain in the arthritic joint.
 A stress view of the TMC joint is obtained by having the patient press the thumb tips together while obtaining a 30-degree posteroanterior view centered on the thumbs to assess joint space loss and subluxation. Stress view is only obtained in stage I disease for patients with symptomatic joint laxity.
A stress view of the TMC joint is obtained by having the patient press the thumb tips together while obtaining a 30-degree posteroanterior view centered on the thumbs to assess joint space loss and subluxation. Stress view is only obtained in stage I disease for patients with symptomatic joint laxity.
 Partial resection of the trapezoid should be performed if degenerative changes are present between the trapezoid and the scaphoid.
Partial resection of the trapezoid should be performed if degenerative changes are present between the trapezoid and the scaphoid.
Surgical Anatomy
 The anterior oblique (beak) ligament inserts volarly onto the trapezium from its confluence with articular cartilage on the beak of the thumb metacarpal.
The anterior oblique (beak) ligament inserts volarly onto the trapezium from its confluence with articular cartilage on the beak of the thumb metacarpal.
 The radial artery traverses the anatomic snuffbox and overlies the dorsal capsule of the CMC joint.
The radial artery traverses the anatomic snuffbox and overlies the dorsal capsule of the CMC joint.
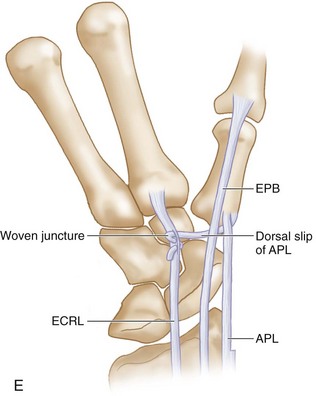
 The abductor pollicis longus (APL) and extensor pollicis brevis (EPB) tendons are within the first extensor compartment.
The abductor pollicis longus (APL) and extensor pollicis brevis (EPB) tendons are within the first extensor compartment.
 The radial sensory nerve becomes subcutaneous after exiting through the interval between the brachioradialis and extensor carpi radialis longus (ECRL) muscles.
The radial sensory nerve becomes subcutaneous after exiting through the interval between the brachioradialis and extensor carpi radialis longus (ECRL) muscles.
 The flexor carpi radialis (FCR) tendon traverses the volar and ulnar aspect of the trapezium.
The flexor carpi radialis (FCR) tendon traverses the volar and ulnar aspect of the trapezium.
Exposures
Pearls
The dorsal approach provides easy access to the trapezium.
For the trapeziectomy, one must identify and protect four structures: radial sensory nerve branches, radial artery, EPL tendon, and APL tendon.
Retract the EPL ulnarly and the APL radially and identify the radial artery, which will be located deep to the fatty tissue between these structures.
Procedure
Step 1
 The distal skin incision is made extending from 1 to 2 cm distal to the TMC joint to the radial styloid proximally.
The distal skin incision is made extending from 1 to 2 cm distal to the TMC joint to the radial styloid proximally.
 The proximal skin incision is made over the course of the first extensor compartment tendons after the trapeziectomy has been completed.
The proximal skin incision is made over the course of the first extensor compartment tendons after the trapeziectomy has been completed.
Step 1 Pearls
The EPL is identified at the ulnar aspect of the anatomic snuffbox.
The radial sensory nerve branches should be mobilized and retracted.
Perforating vessels from the radial artery to the dorsal capsule should be cauterized as the artery is mobilized and retracted ulnarly to gain access to the joint capsule.
Step 2
 Sharply incise the TMC joint capsule and elevate the capsular flaps radially and ulnarly to expose the scaphotrapezial joint, the trapezium, and the thumb metacarpal base (Fig. 62-4).
Sharply incise the TMC joint capsule and elevate the capsular flaps radially and ulnarly to expose the scaphotrapezial joint, the trapezium, and the thumb metacarpal base (Fig. 62-4).
Step 3
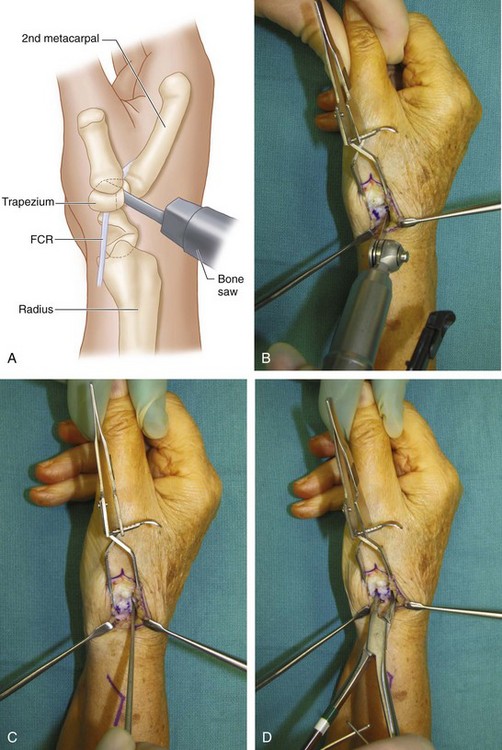
 An oscillating saw is used to cut the trapezium into three pieces (Figs. 62-5A and B), and an osteotome is then used to fracture the bone into separate pieces (Fig. 62-5C). Trapeziectomy is performed with a rongeur (Fig. 62-5D). If scaphotrapezoid arthritis is present, partial proximal trapezoidal resection is performed such that axial loading produces no contact between the scaphoid and trapezoid.
An oscillating saw is used to cut the trapezium into three pieces (Figs. 62-5A and B), and an osteotome is then used to fracture the bone into separate pieces (Fig. 62-5C). Trapeziectomy is performed with a rongeur (Fig. 62-5D). If scaphotrapezoid arthritis is present, partial proximal trapezoidal resection is performed such that axial loading produces no contact between the scaphoid and trapezoid.
Step 3 Pearls
The orientation of the saw cuts should be parallel to the course of the FCR tendon to avoid injury to this tendon as it passes volar to the trapezium at its proximal radial corner.
Traction on the thumb helps facilitate exposure of the trapezium.
There will be a substantial amount of osteophyte attaching to the volar joint capsule and the thenar muscle. All the osteophytes must be excised using both the scalpel and the rongeur.
In certain situations in which the interval between the trapezium and the scaphoid is blurred because of severe degenerative changes, it is useful to obtain a view using the fluoroscopy to be sure the correct bone is removed. It is conceivably possible to remove a portion of the distal scaphoid if not careful.
After trapeziectomy, traction should be exerted on the index and long fingers to assess the scaphotrapezoid joint.
Step 4
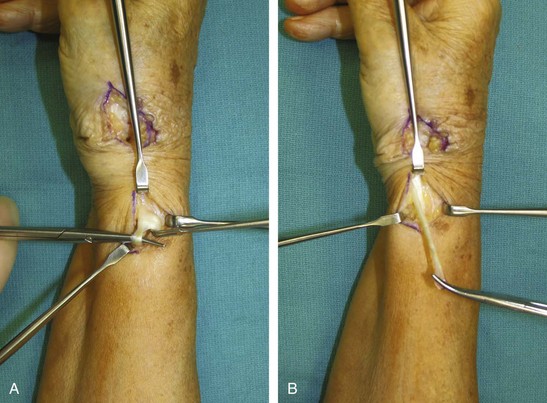
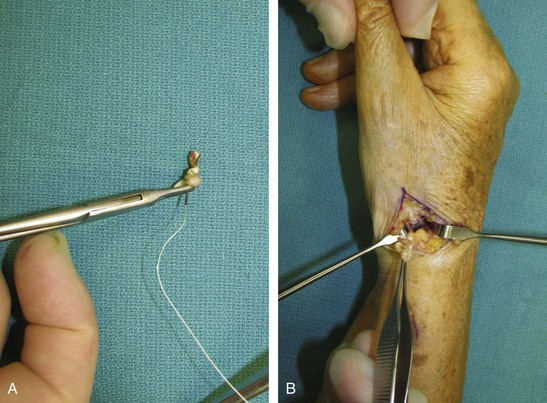
 Identify and release the first extensor compartment (Fig. 62-6). Identify the musculotendinous junction of the APL, divide the most radial slip of the APL at this junction (Fig. 62-7A), and begin to split it distally to its insertion on the base of the thumb metacarpal (Fig. 62-7B).
Identify and release the first extensor compartment (Fig. 62-6). Identify the musculotendinous junction of the APL, divide the most radial slip of the APL at this junction (Fig. 62-7A), and begin to split it distally to its insertion on the base of the thumb metacarpal (Fig. 62-7B).
Step 5
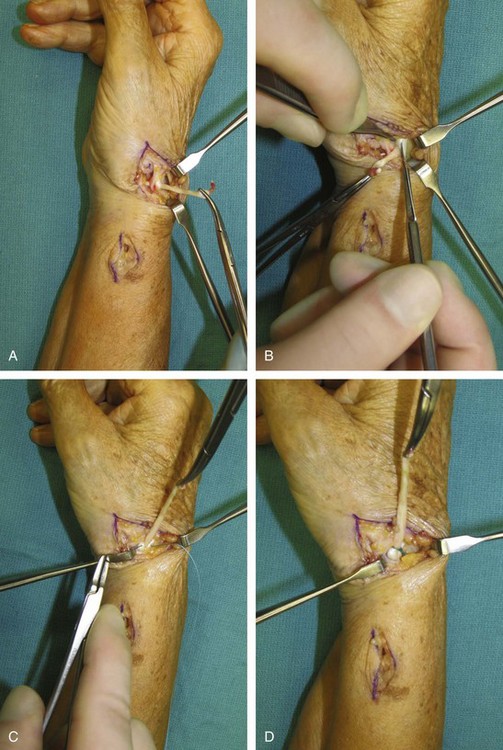
 A hemostat is used to pass the APL tendon subcutaneously and into the arthroplasty space, and the remaining portion is split distally to its insertion at the base of the thumb metacarpal (Fig. 62-8). The ECRL tendon is then identified ulnar and deep to the EPL tendon, inserting into the base of the index metacarpal.
A hemostat is used to pass the APL tendon subcutaneously and into the arthroplasty space, and the remaining portion is split distally to its insertion at the base of the thumb metacarpal (Fig. 62-8). The ECRL tendon is then identified ulnar and deep to the EPL tendon, inserting into the base of the index metacarpal.
Step 6
 The APL tendon is passed volar to the EPL (Fig. 62-9A). A small incision is made in the ECRL tendon, and the APL slip is woven into the ECRL with a tendon passer (Figs. 62-9B and C).
The APL tendon is passed volar to the EPL (Fig. 62-9A). A small incision is made in the ECRL tendon, and the APL slip is woven into the ECRL with a tendon passer (Figs. 62-9B and C).
Step 7
 Tension is set such that the thumb metacarpal base is suspended at the level of the index metacarpal base. The tendon weave is secured with two 3-0 braided permanent horizontal mattress sutures (Fig. 62-9D and E). The remaining tendon is cut, and a 4-0 braided absorbable suture is used to fashion the cut tendon into an accordion-like ball that is placed in the arthroplasty space (Fig. 62-10A and B).
Tension is set such that the thumb metacarpal base is suspended at the level of the index metacarpal base. The tendon weave is secured with two 3-0 braided permanent horizontal mattress sutures (Fig. 62-9D and E). The remaining tendon is cut, and a 4-0 braided absorbable suture is used to fashion the cut tendon into an accordion-like ball that is placed in the arthroplasty space (Fig. 62-10A and B).
Postoperative Care and Expected Outcomes
 A postoperative thumb spica splint is worn for 4 weeks. Sutures are removed at the first postoperative visit (10 to 14 days after surgery) as needed, and scar massage techniques are taught to the patient. (Fig. 62-11 shows postoperative radiographic appearance.)
A postoperative thumb spica splint is worn for 4 weeks. Sutures are removed at the first postoperative visit (10 to 14 days after surgery) as needed, and scar massage techniques are taught to the patient. (Fig. 62-11 shows postoperative radiographic appearance.)
 Four weeks after surgery, hand therapy is begun for passive and active range-of-motion exercises. The splint is worn in between exercises.
Four weeks after surgery, hand therapy is begun for passive and active range-of-motion exercises. The splint is worn in between exercises.
 Six weeks after surgery, light strengthening exercises are begun, and unrestricted passive range of motion is allowed. Splint is worn in between exercises.
Six weeks after surgery, light strengthening exercises are begun, and unrestricted passive range of motion is allowed. Splint is worn in between exercises.
 Eight weeks after surgery, the splint is removed, and heavy strengthening is begun with grip and pinch exercises. Soft neoprene splint is worn as needed.
Eight weeks after surgery, the splint is removed, and heavy strengthening is begun with grip and pinch exercises. Soft neoprene splint is worn as needed.
Chang EY, Chung KC. Outcomes of trapeziectomy with a modified abductor pollicis suspension arthroplasty for the treatment of thumb carpometacarpal joint osteoarthritis. Plast Reconstr Surg. 2008;122:1-12.
Sigfusson R, Lundborg G. Abductor pollicis longus tendon arthroplasty for treatment of arthrosis in the first carpometacarpal joint. Scand J Plast Reconstr Hand Surg. 1991;25:73-77.
Soejima O, Hanamura T, Kikuta T, et al. Suspensionplasty with the abductor pollicis longus tendon for osteoarthritis in the carpometacarpal joint of the thumb. J Hand Surg [Am]. 2006;31:425-428.