CASE 62
History: A patient presents with chest pain.
1. What are the causes of acute aortic syndrome? (Choose all that apply.)
A. Aneurysm
B. Dissection
2. What is the most likely cause of this patient’s abnormality?
B. Dissection
3. What is the cause of a penetrating aortic ulcer?
A. Infection
B. Trauma
C. Iatrogenic
4. What is the most appropriate management?
A. No treatment
B. Antihypertensive medication
D. Surgery
ANSWERS
Reference
Reddy GP, Gunn M, Mitsumori LM, et al. Multislice CT and MRI of the thoracic aorta. In: Webb WR, Higgins CB, eds. Thoracic imaging: pulmonary and cardiovascular radiology. ed 2 Philadelphia: Lippincott Williams & Wilkin; 2010.
Cross-Reference
Cardiac Imaging: The REQUISITES, ed 3, pp 377–379.
Comment
Etiology, Pathology, and Management
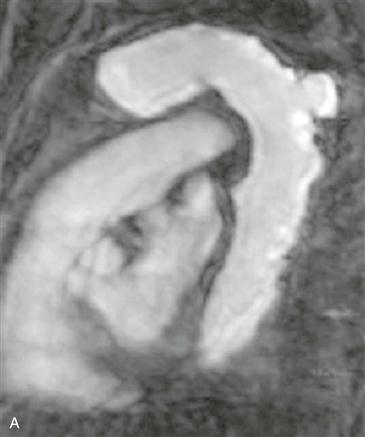
An aortic pseudoaneurysm can be due to a penetrating atherosclerotic ulcer, infection, trauma (deceleration injury—although this is an unusual location), or iatrogenic injury. Pseudoaneurysms are characterized by disruption of one or more layers of the vessel wall, whereas true aneurysms have intact walls. Because pseudoaneurysms are characterized by disruption of one or more layers of the arterial wall, they are at risk for rupture, and management usually involves surgical resection.
Imaging
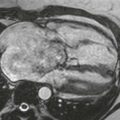
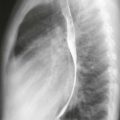
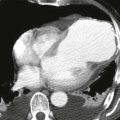
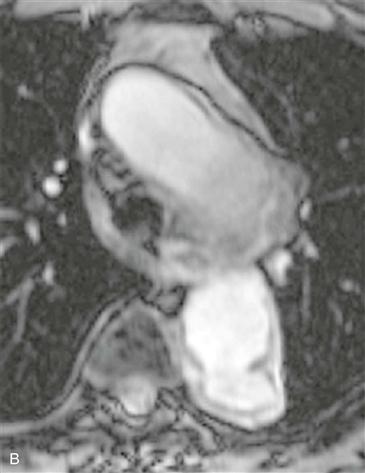
CT and MRI can be used to establish the diagnosis of a thoracic aortic aneurysm. Disruption of the wall is difficult to identify by imaging examination. If the outpouching has a relatively narrow ostium (<50% of the aneurysm diameter), it is likely a pseudoaneurysm (Figs. A and B), whereas an aneurysm with a wide ostium is likely to be a true aneurysm.
Acute Aortic Syndrome
There are three diseases that are classically considered to be a part of the acute aortic syndrome: aortic dissection, intramural hematoma, and penetrating aortic ulcer. Some authors propose including three additional entities: aortitis, intimal tear from trauma, and intraluminal aortic thrombus. Acute aortic syndrome diseases are classified under the Stanford system. Stanford type A lesions involve the ascending aorta and generally are treated surgically or endovascularly with stent grafts. Stanford type B lesions do not involve the ascending aorta and generally are managed medically unless complications develop.