Procedure 61 Trapeziometacarpal Ligament Reconstruction
![]() See Video 45: Thumb CMC Joint Beak Ligament Reconstruction Using the FCR Tendon
See Video 45: Thumb CMC Joint Beak Ligament Reconstruction Using the FCR Tendon
Examination/Imaging
Clinical Examination
 The clinician should stress the trapeziometacarpal (TMC) joint and note any instability and laxity. The extent of ligament rupture (partial versus complete) allows varying degrees of hypermobility. Although hypermobility may be present bilaterally, greater excursion and symptomatic hypermobility should be evident on the affected side.
The clinician should stress the trapeziometacarpal (TMC) joint and note any instability and laxity. The extent of ligament rupture (partial versus complete) allows varying degrees of hypermobility. Although hypermobility may be present bilaterally, greater excursion and symptomatic hypermobility should be evident on the affected side.
Imaging
 A lateral and pronated anteroposterior radiograph should be obtained to evaluate any existing joint disease and to identify the more commonly seen Bennett fracture-dislocation.
A lateral and pronated anteroposterior radiograph should be obtained to evaluate any existing joint disease and to identify the more commonly seen Bennett fracture-dislocation.
 A stressed anteroposterior radiograph of the bilateral thumbs with radial margins pressed together can help elucidate the degree of capsule laxity and presents both thumb joints for comparison (Fig. 61-1).
A stressed anteroposterior radiograph of the bilateral thumbs with radial margins pressed together can help elucidate the degree of capsule laxity and presents both thumb joints for comparison (Fig. 61-1).
Surgical Anatomy
 The TMC joint is a biconcave saddle-shaped joint that provides motion in several planes to allow thumb flexion, extension, abduction, adduction, and opposition.
The TMC joint is a biconcave saddle-shaped joint that provides motion in several planes to allow thumb flexion, extension, abduction, adduction, and opposition.
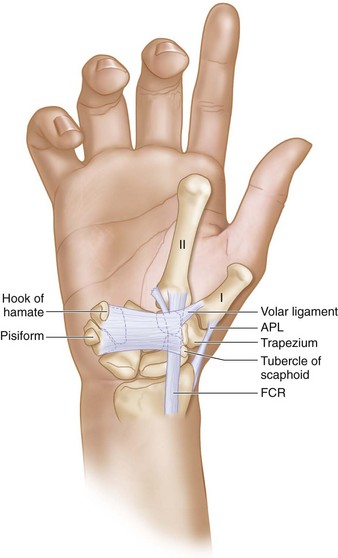
 The volar oblique (beak) ligament inserts volarly onto the trapezium from its confluence with articular cartilage on the beak of the thumb metacarpal and is considered the primary stabilizer of the TMC joint. It serves as the main restraint against dorsal translation of the metacarpal on the trapezium (Fig. 61-2).
The volar oblique (beak) ligament inserts volarly onto the trapezium from its confluence with articular cartilage on the beak of the thumb metacarpal and is considered the primary stabilizer of the TMC joint. It serves as the main restraint against dorsal translation of the metacarpal on the trapezium (Fig. 61-2).
 The thin and less well-defined dorsal ligament is reinforced by an expansion of the insertion of the abductor pollicis longus (APL) tendon onto the dorsal-radial aspect of the metacarpal.
The thin and less well-defined dorsal ligament is reinforced by an expansion of the insertion of the abductor pollicis longus (APL) tendon onto the dorsal-radial aspect of the metacarpal.
 The radial artery traverses the anatomic snuffbox and overlies the dorsal capsule of the carpometacarpal (CMC) joint.
The radial artery traverses the anatomic snuffbox and overlies the dorsal capsule of the carpometacarpal (CMC) joint.
 The abductor pollicis longus (APL) and extensor pollicis brevis (EPB) tendons are within the first extensor compartment.
The abductor pollicis longus (APL) and extensor pollicis brevis (EPB) tendons are within the first extensor compartment.
 The radial sensory nerve becomes subcutaneous after exiting through the interval between the brachioradialis and extensor carpi radialis longus (ECRL) muscles.
The radial sensory nerve becomes subcutaneous after exiting through the interval between the brachioradialis and extensor carpi radialis longus (ECRL) muscles.
 The flexor carpi radialis (FCR) tendon is the most radial tendon palpable on the volar aspect of the wrist and is located just ulnar to the radial artery. The palmaris longus tendon, when present, is ulnar to the FCR tendon.
The flexor carpi radialis (FCR) tendon is the most radial tendon palpable on the volar aspect of the wrist and is located just ulnar to the radial artery. The palmaris longus tendon, when present, is ulnar to the FCR tendon.
 The palmar cutaneous branch of the median nerve is located 1 mm ulnar to the FCR tendon.
The palmar cutaneous branch of the median nerve is located 1 mm ulnar to the FCR tendon.
Exposures
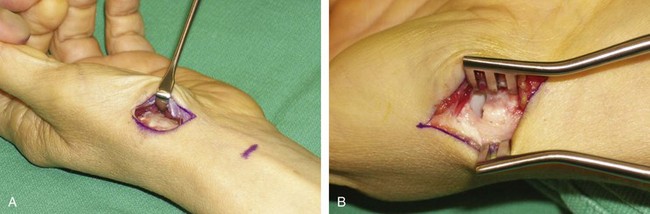
 This procedure requires the following incisions.
This procedure requires the following incisions.
Procedure
Step 1
 Identify the radial edge of the thenar musculature at its insertion onto the metacarpal and elevate the muscle extraperiosteally to expose the metacarpal base, TMC joint, and trapezium (Fig. 61-4).
Identify the radial edge of the thenar musculature at its insertion onto the metacarpal and elevate the muscle extraperiosteally to expose the metacarpal base, TMC joint, and trapezium (Fig. 61-4).
 The interval between the extensor pollicis longus and brevis is developed to expose the dorsal cortex of the metacarpal base.
The interval between the extensor pollicis longus and brevis is developed to expose the dorsal cortex of the metacarpal base.
 A hole is created at the base of the metacarpal from dorsal to volar 1 cm distal to the joint in a plane perpendicular to the axis of the thumbnail using a gouge or small bur. The volar hole should emerge at the apex of the volar beak of the metacarpal.
A hole is created at the base of the metacarpal from dorsal to volar 1 cm distal to the joint in a plane perpendicular to the axis of the thumbnail using a gouge or small bur. The volar hole should emerge at the apex of the volar beak of the metacarpal.
Step 1 Pearls
Although preoperative radiographs may appear normal, these can be deceiving, and degeneration of articular cartilage may be underappreciated. If there is clinical suspicion of articular degeneration, a transverse arthrotomy should be made to visualize the TMC joint surface. The arthrotomy is then closed with 3-0 braided absorbable suture.
Step 2
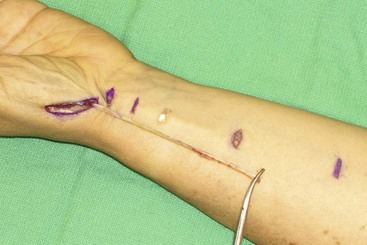
 The FCR tendon is identified at the wrist crease, and the sheath is sharply opened proximally and distally.
The FCR tendon is identified at the wrist crease, and the sheath is sharply opened proximally and distally.
 The radial half of the FCR tendon in the proximal forearm is transected proximally at 6 cm from the wrist crease and separated from the other half of the tendon using two small transverse incisions (Fig. 61-5). At the level of the wrist crease, the FCR is covered by a sheath that needs to be opened to trace the FCR slip close to its insertion at the base of the index metacarpal. The FCR rotates 90 degrees within the sheath; it is important to follow the fibers so that the tendon is not inadvertently transected. One should not slide the scissors through the tendon fibers but rather cut along the fibers to maintain the integrity of the tendon.
The radial half of the FCR tendon in the proximal forearm is transected proximally at 6 cm from the wrist crease and separated from the other half of the tendon using two small transverse incisions (Fig. 61-5). At the level of the wrist crease, the FCR is covered by a sheath that needs to be opened to trace the FCR slip close to its insertion at the base of the index metacarpal. The FCR rotates 90 degrees within the sheath; it is important to follow the fibers so that the tendon is not inadvertently transected. One should not slide the scissors through the tendon fibers but rather cut along the fibers to maintain the integrity of the tendon.
Step 3
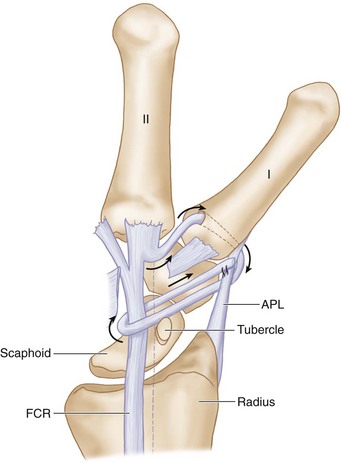
 The free end of the FCR is redirected across the crest of the trapezium to enter the volar portion of the newly created hole at the beak of the thumb metacarpal and drawn dorsally through the metacarpal with the assistance of a wire suture (Figs. 61-6 and 61-7).
The free end of the FCR is redirected across the crest of the trapezium to enter the volar portion of the newly created hole at the beak of the thumb metacarpal and drawn dorsally through the metacarpal with the assistance of a wire suture (Figs. 61-6 and 61-7).
 The TMC joint is reduced under direct vision and held in extension and abduction to seat the metacarpal against the deep facet of the trapezium. It is unnecessary to pin the joint because the tendon is adequate to provide stability to the thumb CMC joint.
The TMC joint is reduced under direct vision and held in extension and abduction to seat the metacarpal against the deep facet of the trapezium. It is unnecessary to pin the joint because the tendon is adequate to provide stability to the thumb CMC joint.
 The tendon is pulled taut and sutured to the dorsal periosteum using a 3-0 braided permanent suture. The tendon is then passed around the metacarpal base deep to the extensor pollicis brevis and APL, through a small split in the intact FCR tendon proximal to its insertion, and finally back across the joint and sutured to the APL tendon using 3-0 braided permanent suture (see Fig. 61-7). Additional 3-0 braided permanent sutures are placed at the junction through the FCR tendon (Fig. 61-8).
The tendon is pulled taut and sutured to the dorsal periosteum using a 3-0 braided permanent suture. The tendon is then passed around the metacarpal base deep to the extensor pollicis brevis and APL, through a small split in the intact FCR tendon proximal to its insertion, and finally back across the joint and sutured to the APL tendon using 3-0 braided permanent suture (see Fig. 61-7). Additional 3-0 braided permanent sutures are placed at the junction through the FCR tendon (Fig. 61-8).
Postoperative Care and Expected Outcomes
 The thumb spica splint is worn for 4 weeks followed by gentle active motion exercises for another 4 weeks. Strengthening is started 8 weeks after surgery.
The thumb spica splint is worn for 4 weeks followed by gentle active motion exercises for another 4 weeks. Strengthening is started 8 weeks after surgery.
 Thumb CMC joint stiffness typically lasts 4 to 6 weeks but may last as long as 4 months.
Thumb CMC joint stiffness typically lasts 4 to 6 weeks but may last as long as 4 months.
 The patient can expect complete or near-complete relief of pain with use of the thumb and minimal or no progression of degenerative arthritis when this surgery is performed before onset of significant articular cartilage degeneration. (Fig. 61-9 shows a late postoperative radiograph.)
The patient can expect complete or near-complete relief of pain with use of the thumb and minimal or no progression of degenerative arthritis when this surgery is performed before onset of significant articular cartilage degeneration. (Fig. 61-9 shows a late postoperative radiograph.)
Eaton RG, Lane LB, Littler JW, Keyser JJ. Ligament reconstruction for the painful thumb carpometacarpal joint: a long-term assessment. J Hand Surg [Am]. 1984;9:692-699.
Freedman DM, Eaton RG, Glickel SZ. Long-term results of volar ligament reconstruction for symptomatic basal joint laxity. J Hand Surg [Am]. 2000;25:297-304.
Takwale VJ, Stanley JK, Shahane SA. Post-traumatic instability of the trapeziometacarpal joint of the thumb: diagnosis and the results of reconstruction of the beak ligament. J Bone Joint Surg [Br]. 2004;86:541-545.