CHAPTER 60 Obstetric Analgesia and Anesthesia
1 What are the most commonly used parenteral opioids for labor analgesia? Which side effects are of special concern to the parturient?
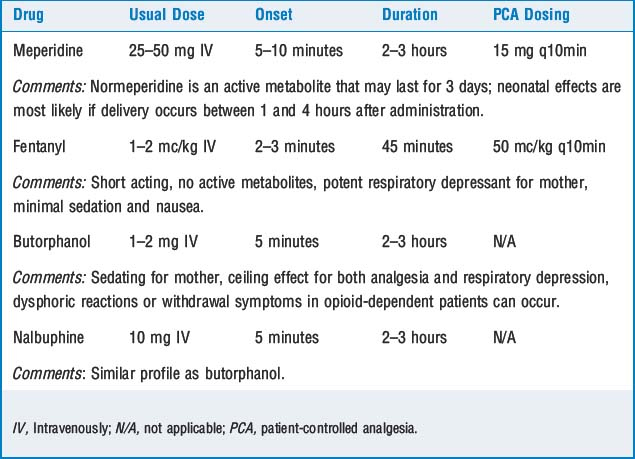
Table 60-1 summarizes commonly used parenteral opioids and their side effects. In general, intravenous medications help the parturient tolerate labor pain but do not provide complete analgesia. The incidence of side effects and efficacy of analgesia are dose dependent. Maternal sedation and nausea are common. Opioids easily cross the placenta and may cause a decrease in fetal heart rate variability. In addition, intravenous opioids may cause neonatal respiratory depression and neurobehavioral changes.
2 What advantages does PCA offer over conventional intermittent bolus dosing?
Patient-controlled analgesia (PCA) has been associated with greater patient satisfaction, less risk of maternal respiratory depression, less need for antiemetic use, and better pain relief despite lower drug doses. PCA is especially useful if epidural anesthesia is contraindicated or not available. The most experience has been gained with meperidine and fentanyl using the regimens noted in Table 60-1.
5 Discuss the importance of a test dose and suggest an epidural test dose regimen. When and why is this regimen used?
6 What are the characteristics of the ideal local anesthetic for use in labor? Discuss the three most common local anesthetics used in obstetric anesthesia. How does epinephrine affect the action of local anesthetics?
8 Name three methods for administering epidural analgesia. State the concerns associated with each
 Intermittent injection requires that the catheter be checked for migration into the subarachnoid space or a blood vessel via aspiration and a repeat test dose. After multiple injections the patient may develop intense motor blockade.
Intermittent injection requires that the catheter be checked for migration into the subarachnoid space or a blood vessel via aspiration and a repeat test dose. After multiple injections the patient may develop intense motor blockade. Epidural analgesia may also be maintained by continuous infusion of dilute local anesthetic (with or without added opioid). The benefits of this method include:
Epidural analgesia may also be maintained by continuous infusion of dilute local anesthetic (with or without added opioid). The benefits of this method include:
 The patient should be assessed regularly for adequacy of analgesia and lack of motor blockade. The infusion pump should be different from that of intravenous infusion lines, and infusion tubing should be free of side ports to minimize the chance of accidental injection of other substances into the epidural space.
The patient should be assessed regularly for adequacy of analgesia and lack of motor blockade. The infusion pump should be different from that of intravenous infusion lines, and infusion tubing should be free of side ports to minimize the chance of accidental injection of other substances into the epidural space. With patient-controlled epidural anesthesia (PCEA), the patient may deliver small incremental doses in addition to a programmed background infusion to control the level of analgesia. PCEA usually results in greater patient satisfaction and less total dosage of drug than other techniques. As with a continuous infusion, the patient should be checked frequently for degree of analgesia and motor blockade.
With patient-controlled epidural anesthesia (PCEA), the patient may deliver small incremental doses in addition to a programmed background infusion to control the level of analgesia. PCEA usually results in greater patient satisfaction and less total dosage of drug than other techniques. As with a continuous infusion, the patient should be checked frequently for degree of analgesia and motor blockade.9 Discuss the complications of epidural anesthesia and their treatments
 Give the patient 100% oxygen and intubate if necessary (to oxygenate, hyperventilate, and protect the airway).
Give the patient 100% oxygen and intubate if necessary (to oxygenate, hyperventilate, and protect the airway). Consider administration of intralipid to act as a lipid “sink” to bind the local anesthetic and remove it from the maternal circulation.
Consider administration of intralipid to act as a lipid “sink” to bind the local anesthetic and remove it from the maternal circulation.10 Explain the mechanism of action of intrathecal and epidural opioids. What effect do they have on pain perception, sympathetic tone, sensation, and movement?
11 What opioids are used to provide spinal and epidural analgesia during labor? Name their most common side effects. Do they provide adequate analgesia for labor and delivery when used alone?
The most commonly used neuraxial (spinal and epidural) opioids are fentanyl and sufentanil (Table 60-2). Pruritus, nausea, and vomiting are the most common side effects; delayed respiratory depression is the most serious complication, although very uncommon in this population. Intrathecal or epidural opioids alone may provide adequate relief for the early stages of labor, but they are unreliable in producing adequate analgesia for the active phase of labor. Very high doses of epidural opioids are required, which leads to excessive side effects. Concurrent administration of local anesthetic is necessary for late cervical dilation and delivery of the infant.
TABLE 60-2 Opioids used to Provide Intrathecal (Spinal) Analgesia During Labor
| Drug | Dose |
|---|---|
| Fentanyl | 25 mcg |
| Sufentanil | 5 mcg |
| Morphine | 0.25 mg |
| Meperidine | 10 mg |
12 Is there a cause-and-effect relationship between epidural anesthesia and prolonged labor or operative delivery?
13 Relate the advantages and disadvantages of spinal anesthesia for cesarean section. Which drugs are frequently used in the technique?
Spinal anesthesia produces a dense neural blockade; it is relatively easy to perform, has a rapid onset, and carries no risk of local anesthetic toxicity. The development of small-gauge, noncutting needles has significantly reduced the incidence of postdural-puncture headache (PDPH) to 1% or less. Hypotension can be treated by rapid hydration (1 L colloid or 1 to 2 L crystalloid), positioning to avoid aortocaval compression, and use of phenylephrine (50 to 100 mcg) or ephedrine (5 to 10 mg IV) if blood pressure does not improve with these measures. Commonly used drugs for spinal anesthesia are summarized in Table 60-3.
TABLE 60-3 Drugs used for Spinal Anesthesia for Cesarean Section
| Dose | Duration (minutes) | |
|---|---|---|
| Lidocaine | 75 mg | 45–75 |
| Bupivacaine | 11 mg | 60–120 |
| Tetracaine | 7–10 mg | 90–120 |
| Adjuvant Drugs | ||
| Epinephrine | 200 mcg | |
| Morphine | 0.1–0.3 mg | |
| Fentanyl | 10–25 mcg | |
14 What are the advantages and disadvantages of cesarean section with epidural anesthesia vs. spinal anesthesia? What are the most commonly used local anesthetics?
15 How is combined spinal/epidural anesthesia performed? What are its advantages?
KEY POINTS: Obstetric Analgesia and Anesthesia 
17 What concerns the practitioner when administering general anesthesia for cesarean section? How is it performed?
1. American College of Obstetricians and Gynecologists Committee Opinion 339. Analgesia and cesarean delivery rates. Obstet Gynecol. 2006;107:1487-1488.
2. American College of Obstetricians and Gynecologists Practice Bulletin 36. Obstetric analgesia and anesthesia. Washington, DC: American College of Obstetricians and Gynecologists, 2002.
3. American Society of Anesthesiologists Task Force on Obstetrical Anesthesia. Practice guidelines for obstetrical anesthesia: an updated report. Anesthesiology. 2007;106:843-863.
4. Cyna A.M., Dodd J. Clinical update: obstetric anaesthesia. Lancet. 2007;370:640-642.
5. Simmons S.W., Cyna A.M., Dennis A.T., et al. Combined spinal-epidural versus epidural analgesia in labour. Cochrane Database Syst Rev. 3, 2007. CD003401
6. Weinberg G.L. Current concepts in resuscitation of patients with local anesthetic cardiac toxicity. Reg Anesth Pain Med. 2002;27:568-575.