Procedure 6 Surgical Treatment of de Quervain Tendovaginitis
![]() See Video 3: Release of First Dorsal Compartment for de Quervain Tendovaginitis
See Video 3: Release of First Dorsal Compartment for de Quervain Tendovaginitis
Examination/Imaging
Clinical Examination
 The patient has tenderness over the radial styloid and may have triggering of the thumb extensor tendons. The following two tests can be done to confirm the presence of de Quervain disease.
The patient has tenderness over the radial styloid and may have triggering of the thumb extensor tendons. The following two tests can be done to confirm the presence of de Quervain disease.
 The examiner must evaluate for and rule out other causes of radial wrist pain. They include thumb basal joint arthritis, scaphoid fracture, Wartenberg syndrome (compression of the superficial sensory branch of the radial nerve between the extensor carpi radialis longus [ECRL] and brachioradialis [BR]), intersection syndrome (tendinitis at the crossing over of the APL and EPB muscle bellies over the ECRL and extensor carpi radialis brevis [ECRB]), scaphotrapeziotrapezoid (STT) arthritis, and Preiser disease (avascular necrosis of the scaphoid).
The examiner must evaluate for and rule out other causes of radial wrist pain. They include thumb basal joint arthritis, scaphoid fracture, Wartenberg syndrome (compression of the superficial sensory branch of the radial nerve between the extensor carpi radialis longus [ECRL] and brachioradialis [BR]), intersection syndrome (tendinitis at the crossing over of the APL and EPB muscle bellies over the ECRL and extensor carpi radialis brevis [ECRB]), scaphotrapeziotrapezoid (STT) arthritis, and Preiser disease (avascular necrosis of the scaphoid).
Surgical Anatomy
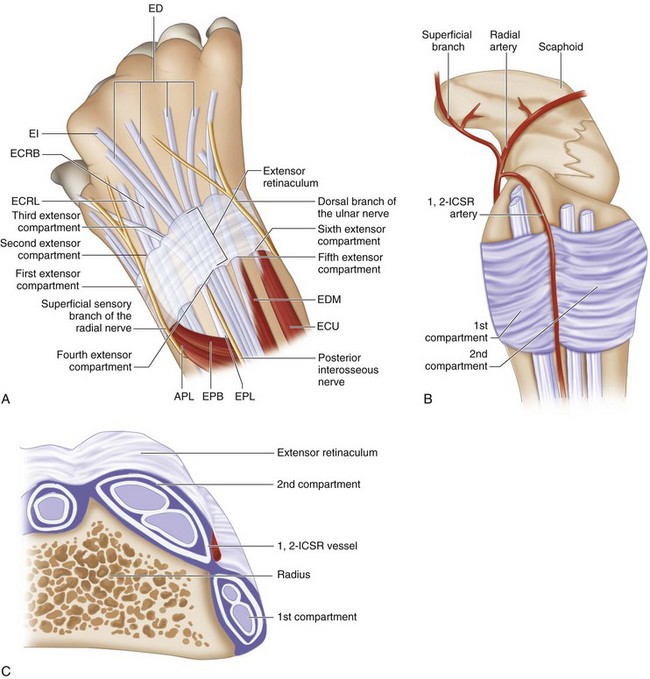
 Six extensor compartments have been described over the dorsum of the wrist (Fig. 6-3A).
Six extensor compartments have been described over the dorsum of the wrist (Fig. 6-3A).
 The first dorsal compartment is involved in de Quervain tendovaginitis. It contains two tendons, the APL and the EBP (Fig. 6-3B and C). The APL tendon has multiple slips. The APL tendon is more radial and volar, whereas the EPB tendon is ulnar and dorsal. In up to 40% of subjects, there may be a separate subsheath for each of the two tendons.
The first dorsal compartment is involved in de Quervain tendovaginitis. It contains two tendons, the APL and the EBP (Fig. 6-3B and C). The APL tendon has multiple slips. The APL tendon is more radial and volar, whereas the EPB tendon is ulnar and dorsal. In up to 40% of subjects, there may be a separate subsheath for each of the two tendons.
 The first dorsal compartment is about 2 cm long, with the floor formed by a groove on the radial surface of the radial styloid. The walls are formed by tough intercompartmental connective tissue septa extending from the bony floor to the roof, or extensor retinaculum.
The first dorsal compartment is about 2 cm long, with the floor formed by a groove on the radial surface of the radial styloid. The walls are formed by tough intercompartmental connective tissue septa extending from the bony floor to the roof, or extensor retinaculum.
 The radial artery is volar to the first compartment but is closely related to the floor of the distal end of the first compartment near the radial styloid on its way to the anatomic snuff from a volar to dorsal direction.
The radial artery is volar to the first compartment but is closely related to the floor of the distal end of the first compartment near the radial styloid on its way to the anatomic snuff from a volar to dorsal direction.
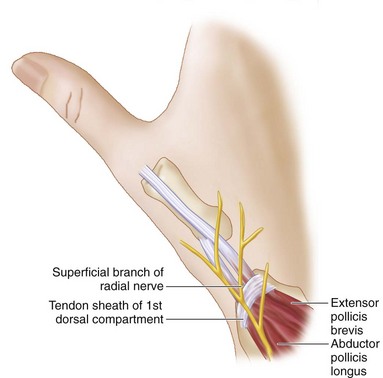
 The radial sensory nerve has several branches in the subcutaneous tissue superficial to the extensor retinaculum. Most complications during this operation are a result of traction injury of this nerve, leading to persistent pain at the incision site (Fig. 6-4).
The radial sensory nerve has several branches in the subcutaneous tissue superficial to the extensor retinaculum. Most complications during this operation are a result of traction injury of this nerve, leading to persistent pain at the incision site (Fig. 6-4).
Exposures
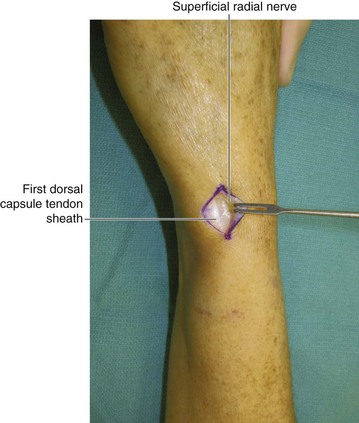
 A 3-cm longitudinal chevron incision is made extending proximally from the radial styloid over the first compartment (Fig. 6-5). As soon as the deep portion of the dermis is opened, gentle blunt dissection with a scissors should be used to expose the extensor retinaculum over the first dorsal compartment. The skin flaps can then be gently elevated to fully expose the first compartment.
A 3-cm longitudinal chevron incision is made extending proximally from the radial styloid over the first compartment (Fig. 6-5). As soon as the deep portion of the dermis is opened, gentle blunt dissection with a scissors should be used to expose the extensor retinaculum over the first dorsal compartment. The skin flaps can then be gently elevated to fully expose the first compartment.
Pearls
The scissors should be spread in a longitudinal direction to avoid injury to the longitudinally oriented branches of the superficial radial nerve.
The nerve should be identified and protected. It is best to avoid dissection of the nerve, but where required, a thick cuff of perineural fat should be maintained to prevent adhesions of the nerve to the skin or the scar (Fig. 6-6).
Procedure
Step 1
 The first dorsal compartment is opened along its entire length with a no. 15 scalpel blade (Fig. 6-7). One should inspect the compartment for presence of any subsheaths, which should be individually released (Fig. 6-8).
The first dorsal compartment is opened along its entire length with a no. 15 scalpel blade (Fig. 6-7). One should inspect the compartment for presence of any subsheaths, which should be individually released (Fig. 6-8).
 Any hypertrophic synovium should be excised.
Any hypertrophic synovium should be excised.
 Release is visually confirmed and verified by taking the thumb through a full range of motion (Fig. 6-9).
Release is visually confirmed and verified by taking the thumb through a full range of motion (Fig. 6-9).
Postoperative Care and Expected Outcomes
 The patient should wear the gentle compression dressing for several days followed by liberalization of movement as the wound heals.
The patient should wear the gentle compression dressing for several days followed by liberalization of movement as the wound heals.
 The majority of patients (>90%) should have nearly immediate relief of symptoms after release of the first compartment. If symptoms persist, one must consider inadequate release of unrecognized subsheaths within the first compartment.
The majority of patients (>90%) should have nearly immediate relief of symptoms after release of the first compartment. If symptoms persist, one must consider inadequate release of unrecognized subsheaths within the first compartment.
 Occasionally patients with prolonged symptoms and stiffness may require progressive therapy for active and passive motion and progressive strengthening. This can begin immediately after surgery.
Occasionally patients with prolonged symptoms and stiffness may require progressive therapy for active and passive motion and progressive strengthening. This can begin immediately after surgery.
 If a patient develops a sensitive scar, desensitization therapy should be recommended with close clinical follow-up.
If a patient develops a sensitive scar, desensitization therapy should be recommended with close clinical follow-up.
Ahuja NK, Chung KC. Fritz de Quervain, MD (1868-1940): stenosing tendovaginitis at the radial styloid process. J Hand Surg [Am]. 2004;29:1164-1170.
Ta KT, Eidelman D, Thomson G. Patient satisfaction and outcomes of surgery for de Quervain’s tenosynovitis. J Hand Surg [Am]. 1999;23:1071-1077.
Weiss AC, Akelman E, Tabatabi M. Treatment of de Quervain’s disease. J Hand Surg [Am]. 1994;19:595-598.
Witt J, Pess G, Gelberman RH. Treatment of de Quervain tenosynovitis: a prospective study of the results of injection of steroids and immobilization in a splint. J Bone Joint Surg [Am]. 1991;73:219-222.