TOPIC 6 Renal, metabolic and endocrine systems
Assessment of renal function: Serological tests
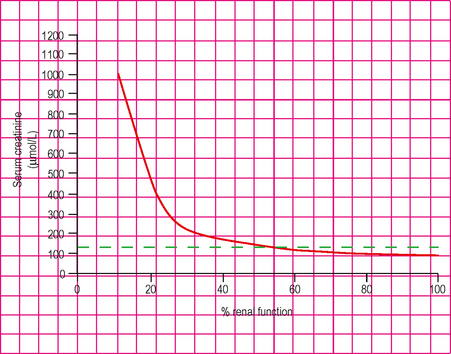
Test: Serum creatinine
Abnormalities and management principles
Renal failure/impairment
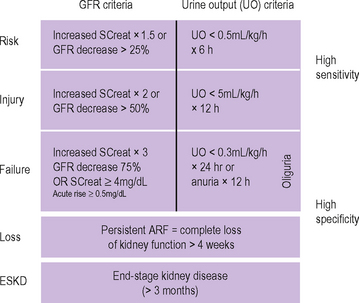
Fig. 6.2 The RIFLE criteria for classification of renal dysfunction.
(Adapted from Bellomo et al. (2004) Crit Care Med 8:R204-R212, with permission.)
Acute renal failure
| Classification | Example of causes | |
|---|---|---|
| ‘Pre-renal’ | Pre-renal failure causing renal hypoperfusion and acute tubular necrosis | |
Chronic renal failure
| Intrinsic causes | Obstructive causes |
|---|---|
| Diabetic nephropathy | Post-obstructive nephropathy |
| Chronic glomerulonephritis | Nephrolithiasis |
| Renovascular disease | Multiple myeloma |
| Chronic reflux nephropathy | |
| Polycystic kidney disease | |
| Amyloidosis | |
| Post-acute renal failure | |
| Chronic interstitial nephritis | |
| Analgesic nephropathy |
Test: Serum urea measurement
Interpretation
Physiological principles
Assessment of renal function: urinalysis
Test: urine dipstick
Abnormalities and management principles
A few causes of an abnormal urine dipstick are listed in Table 6.3.
| Finding | Causes |
|---|---|
| Glycosuria | Diabetes mellitus |
| Tubular dysfunction | |
| Pregnancy | |
| Proteinuria | Glomerular dysfunction, e.g. pre-eclamptic toxaemia |
| Orthostatic proteinuria (benign; occurs after prolonged standing) | |
| Fever | |
| Severe exercise | |
| Lower urinary tract infection | |
| Nephrotic syndrome | |
| High pH | Distal renal tubular acidosis (renal bicarbonate losses) |
| Low specific gravity | Diabetes insipidus |
| Red cells | Rhabdomyolysis |
| Urinary tract infection | |
| Glomerulonephritis | |
| Leucocytes | Urinary tract infection |
| Nitrites | Gram-negative bacterial urinary tract infection |
| Bilirubin/increased urobilinogen | Conjugated bilirubin appears in presence of obstructive jaundice |
Test: Urine microscopy
Abnormalities and management principles
| Finding | Causes |
|---|---|
| Red cells | Glomerular bleeding or dysfunction |
| Infection | |
| Traumatic catheterization | |
| White cells | Infection |
| Some cases of glomerular disease | |
| Some cases of interstitial nephritis | |
| Crystals | Renal calculi |
| Gout (uric acid crystals) | |
| Casts | |
| Hyaline casts | Normal |
| Granular casts | Nonspecific |
| Tubular cell casts | Acute tubular necrosis or interstitial nephritis |
| Red cell casts | Glomerulonephritis or glomerular bleeding |
| Leucocyte casts | Acute tubular necrosis or pyelonephritis |
Test: Laboratory assay of urine sodium, osmolality, urea, creatinine and specific gravity
Interpretation
Physiological principles
Normal ranges
| Investigation | Prerenal oliguria | Acute tubular necrosis |
|---|---|---|
| Urine sodium (mmol/L) | <20 | >40 |
| Specific gravity | >1.020 | <1.010 |
| Urine osmolality (mosmol/kg) | >500 | <350 |
| Urine: plasma osmolality ratio | >2 | <1.1 |
| Urine: plasma urea ratio | >20 | <10 |
| Urine: plasma creatinine ratio | >40 | <20 |
| Fractional sodium excretion* | <<1% | >1% |
* Percentage of sodium filtered at the glomerulus (normally 1000 mmol/hour), which actually appears in the urine (normally 6 mmol/hour; i.e. 0.6%).
Assessment of renal function: Measurement of glomerular filtration rate
Test: Radioisotope assay
Interpretation
Test: Inulin clearance
Physiological principles
Assessment of renal function: Radiological
Serological measurement of electrolytes
Test: Serum sodium measurement
Indications
Interpretation
Physiological principles
Abnormalities and management principles
Hyponatraemia
Causes
Hyponatraemia may be divided into three categories:
Assessment of total body fluid status and the measurement of urinary sodium are both crucial to identifying the cause of hyponatraemia. Causes of ‘real’ hyponatraemia may be classified as in Table 6.6.
| Urine sodium (mmol/L) | Eu or hypervolaemia with oedema | Hypovolaemia |
|---|---|---|
| >20 |
Clinical features
Hypernatraemia
The causes of hypernatraemia can be classified as in Table 6.7, paying attention to the urinary sodium concentration.
| Urine sodium | Examples |
|---|---|
| >20 mmol – true hypernatraemia | Iatrogenic (e.g. administration of hypertonic saline or sodium bicarbonate solutions) |
| Cushing’s syndrome | |
| Conn’s syndrome (hyperaldosteronism) | |
| <20 mmol – sodium depletion with greater water depletion | Renal loss from osmotic diuresis (e.g. hyperglycaemia, uraemia, administration of mannitol) |
| <10 mmol – sodium depletion with more severe water depletion | Adrenocortical insufficiency |
| Increase in insensible losses – e.g. from sweating or suppurating wounds | |
| Diarrhoea and vomiting | |
| Variable urinary sodium – pure water depletion | Renal water loss from diabetes insipidus |
| Dehydration from insufficient water intake |
Limitations and complications
Serum sodium measurement can be inaccurate in uraemia or hyperbilirubinaemia.
Test: Serum potassium measurement
Interpretation
Abnormalities and management principles
Hypokalaemia
Classification of the causes of hypokalaemia can be made according to the urinary potassium excretion and plasma renin activity (Table 6.8).
| Potassium excretion <30 mmol/day | Potassium excretion >30 mmol/day with low plasma renin activity | Potassium excretion >30 mmol/day with high plasma renin activity |
|---|---|---|
Hyperkalaemia
Causes of hyperkalaemia can be divided into those that result from increased intake, decrease output or transcellular movement into the plasma (Table 6.9).
| Increased intake | Decreased renal output | Movement of potassium out of cells |
|---|---|---|
Clinical features
Limitations and complications
Test: Serum magnesium
Interpretation
Abnormalities and management principles
Hypomagnesaemia
Hypomagnesaemia is often found in association with hypocalcaemia and hypokalaemia (Table 6.10). It may be asymptomatic, but may present with the following clinical features:
| Cause | Examples |
|---|---|
| Gastrointestinal loss | Diarrhoea and vomiting; malabsorption syndromes; malnutrition; small bowel disorders; chronic alcoholism |
| Acute pancreatitis (magnesium sumps form in areas of fatty necrosis) | |
| Renal loss | Loop and thiazide diuretics; acute alcohol intake; diabetic ketoacidosis; hypercalcaemia |
| Loop of Henle disorders | Acute tubular necrosis; renal transplantation; post-obstructive diuresis |
| Nephrotoxicity | Amphotericin B; aminoglycosides; ciclosporin A; cisplatin; pentamidine; digoxin |
| Other | SIADH; hyperaldosteronism |
Hypermagnesaemia
True hypermagnesaemia is rare. It is usually due to renal insufficiency or exogenous ingestion (Table 6.11).
| Cause | Examples |
|---|---|
| Renal | Renal failure of any aetiology |
| Exogenous administration | Purgatives (e.g. magnesium sulphate) |
| Antacids (e.g. magnesium trisilicate) | |
| Therapeutic magnesium infusions/enemas | |
| Drugs | Lithium |
| Theophylline toxicity | |
| Other | Adrenal insufficiency |
Clinical features of hypermagnesaemia may occur at levels greater than 3–4 mmol/L and include:
Treatment with intravenous calcium may temporarily reverse toxic effects.
Test: Serum calcium
How it is done
Interpretation
Physiological principles
Hypocalcaemia
| Decreased calcium absorption | Hyperphosphataemia (causing reduced ionized calcium levels) | Miscellaneous |
|---|---|---|
Limitations and complications
Test: Serum phosphate
Interpretation
Abnormalities and management principles
Hyperphosphataemia
Clinical features
Test: Serum chloride
Abnormalities and management principles
Hyperchloraemia
Test: Serum lactate
Interpretation
Management principles
Test: Serum bicarbonate
Investigation of salt and water disturbance
Test: Serum osmolality
Interpretation
Abnormalities and management principles
Syndrome of inappropriate ADH secretion (SIADH)
Diabetes insipidus (DI)
Assessment of thyroid function
Test: Serum thyroid hormones measurement
Interpretation
Abnormalities and management principles
Hyperthyroidism
Causes
| Cardiovascular | Dyspnoea; atrial fibrillation; high-output cardiac failure |
| Musculoskeletal | Proximal myopathy, periodic paralysis; osteoporosis; hypercalcaemia |
| Blood | Leucopenia; microcytic anaemia |
Hypothyroidism
Causes
| General | Serous effusions (ascites, pleural, pericardial or joint effusions); hypothermia |
| Cardiovascular | Hypercholestrolaemia and ischaemic heart disease; bradycardia; cardiomegaly |
| ECG changes include low-voltage complexes and T wave flattening/inversion | |
| Respiratory | Hypoventilation |
| Musculoskeletal | Muscular chest pain; muscular cramps; raised creatinine kinase |
| Blood | Macrocytic anaemia; microcytic anaemia in context of menorrhagia in women |
Assessment of glycaemic control
Test: Serum glucose
Abnormalities and management principles
Chronic hyperglycaemia
Acute hyperglycaemia
Acute hypoglycaemia
Test: Glycosylated haemoglobin (HbA1C)
Investigation of the hypothalamic–pituitary axis
Test: Short synacthen test
Abnormalities
The causes of adrenocortical insufficiency may be divided into:
Adrenal insufficiency as demonstrated by an inadequate increment in serum cortisol in response to a short synacthen test may result in a variety of clinical, biochemical and haematological abnormalities. The clinical features differ in acute and chronic adrenocortical insufficiency (Table 6.20).
Table 6.20 Acute versus chronic adrenocortical insufficiency
| Acute | Chronic |
|---|---|
| Clinical features |
Measurement of hormones: Phaeochromocytoma
Test: Plasma and urine catecholamines and their metabolites
How it is done
Interpretation
Physiological principles
Management principles
Resection of phaeochromocytomas involves careful anaesthetic preparation.