CHAPTER 6
Cervical Sprain or Strain
Definition
Cervical sprain or strain typically refers to acute pain arising from injured soft tissues of the neck, including muscles, tendons, and ligaments. The most common event leading to such injuries is motor vehicle collision. The mechanism of injury is complex. During a rear-end motor vehicle collision, the initial head and neck acceleration lags behind vehicular acceleration. Eventually, head and neck acceleration reaches up to 21⁄2 times the maximum car acceleration, which subsequently results in dramatic deceleration at end range of motion of the neck [1,2]. Whereas such injury can also result in fracture, disc, or neurologic injury, cervical strain or sprain, by definition, excludes these entities.
Although these other entities need to be excluded from the differential diagnosis, recent evidence implicates the zygapophyseal joints as a source of neck pain after whiplash injury. Specifically, in a randomized controlled trial in which the medial branches of the cervical dorsal rami were blocked with local anesthetic or treated with saline, it was shown that 60% of patients with whiplash injury had complete neck pain relief after injection of local anesthetic compared with no relief by injection of placebo [3].
Many factors have been associated with worse outcome in acceleration-deceleration injuries involving motor vehicles. Older women tend to have a worse prognosis than that of younger women and men in general. In addition, poor education and a history of prior neck pain are prognostic factors for worse pain in women. Low family income, history of prior neck pain, and lack of awareness of head position in the crash are associated with a poor prognosis in men [4]. Additional crash-related factors associated with a worse outcome include occupancy in a truck, being a passenger, colliding with a moving object, and getting hit head-on or perpendicularly [5]. A high intensity of neck pain, a decreased onset of latency of the initial pain, and radicular symptoms are also prognostic of worse outcomes [6]. Because many of these injuries result in initiation of litigation by patients, this too is a poor prognostic indicator.
Other causes include sleeping in awkward positions, lifting or pulling heavy objects, and repetitive motions involving the head and neck.
Estimates exist that 1 million whiplash injuries each year are due to motor vehicle collisions. The annual incidence varies worldwide, but in North America and western Europe, the incidence is likely to be at least 300 per 100,000 inhabitants [6].
Symptoms
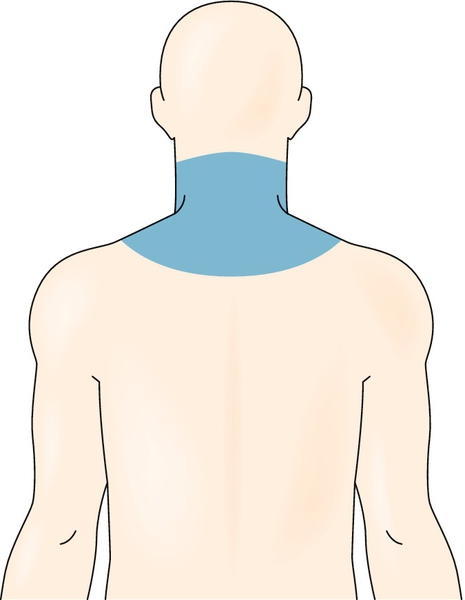
The most common presentation of patients with cervical strain or sprain is nonradiating neck pain (Fig. 6.1). Patients will also complain of neck stiffness, fatigue, and worsening of symptoms with cervical range of motion. The pain often extends into the trapezius region or interscapular region. Headache, probably the most common associated symptom, originates in the occiput region and radiates frontally. Increased irritability and sleep disturbances are common. Paresthesias, radiating arm pain, dysphagia, visual symptoms, auditory symptoms, and dizziness may be reported [7,8]. Whereas an isolated cervical sprain or strain injury should be without these symptoms, there is the possibility of concomitant neurologic or bone injury. If these symptoms are present, alternative diagnoses should be suspected. Myelopathic symptoms, such as bowel and bladder dysfunction, which suggest a different diagnosis that is more serious, must be investigated.
Physical Examination
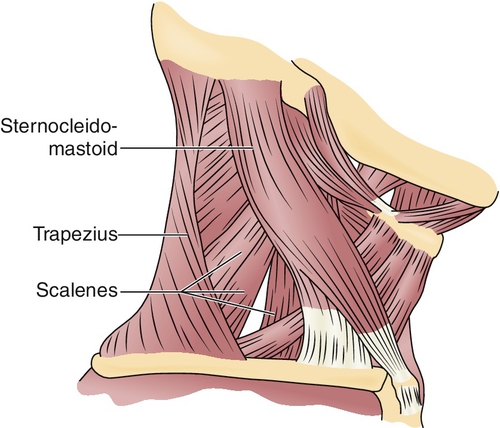
The primary finding in a cervical sprain or strain injury is decreased or painful cervical range of motion. This may be accompanied by tenderness of the cervical paraspinal, trapezius, occiput, or anterior cervical (i.e., sternocleidomastoid) muscles (Fig. 6.2).
A thorough neurologic examination should be performed to rule out myelopathic or radicular processes. In an isolated cervical sprain injury, the neurologic examination findings should be normal.
The result of the neurocompression test, in which the patient is asked to rotate and extend the head, thereby reducing the neuroforaminal space, should be negative with cases of cervical sprain or strain.
Functional Limitations
Restricted range of motion of the cervical spine may contribute to difficulty with daily activities, such as driving. Patients often complain of neck fatigue, heaviness, and pain with static cervical positions, such as reading and working at the computer. Sleep may be affected as well.
Diagnostic Studies
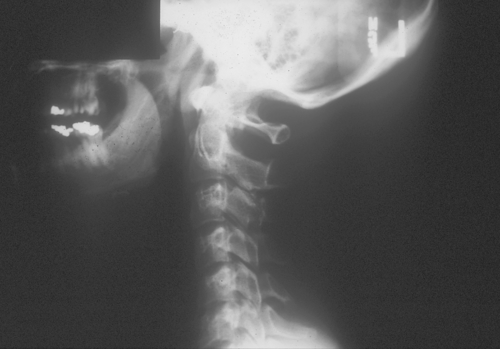
It is generally accepted that radiographs to exclude fracture should be obtained in patients involved in a traumatic event and who have altered consciousness, are intoxicated, or exhibit cervical tenderness and focal neurologic signs with decreased range of motion on physical examination [9]. Although the clinician may commonly see straightening of the cervical lordosis on the lateral cervical radiograph, this is thought to be related to spasm of the paracervical musculature and bears no other significance (Fig. 6.3).
Studies such as magnetic resonance imaging scans, computed tomographic scans, and electrodiagnostics are typically used to rule out alternative or coexisting entities. All of these studies will have normal findings in cases of cervical sprain or strain.
Treatment
Initial
Initial interventions used in patients with cervical sprain or strain have not been fully scientifically tested. Education of the patient is essential to minimize iatrogenic disability and cost of health care resources [10], and it is critical for a realistic expectation of resolution of symptoms. In most cases, symptoms will resolve within 4 to 6 weeks. In some cases, however, resolution of symptoms may be delayed up to 6 months.
It is reasonable to recommend relative rest within the first 24 hours of injury. The detriments of prolonged bed rest and the use of cervical collars have been clearly described, and these “treatments” may, in fact, promote disability [11]. The short-term use of nonsteroidal anti-inflammatory drugs, muscle relaxants, and analgesic medications on a judicious basis is accepted to promote early return to activity [12]. Muscle relaxants or low-dose tricyclic antidepressants (nortriptyline or amitriptyline, beginning with 10 to 25 mg at bedtime) are also used to help restore sleep in the patient for whom this is an issue. However, in the acute period, the addition of cyclobenzaprine to ibuprofen did not provide any added benefit in terms of improving pain scores [13].
High-dose intravenous methylprednisolone within 8 hours of the whiplash injury has been studied and was shown to be associated with decreased pain at 1 week after injury and fewer total sick days taken at 6 months. However, larger trials are needed to further evaluate the cost-benefit ratio for this treatment [14].
Rehabilitation
No rehabilitation approach has been proved unequivocally effective, although early mobilization and return to function is the key to successful rehabilitation. An early course of mobilization combined with home exercise in the acute phase of recovery is effective in minimizing disability. Cervical manipulation, massage, and mobilization on a limited basis are geared toward correction of segmental restrictions and restoration of normal range of motion. Such approaches have been shown to be more effective than passive modalities with regard to range of motion and reduction of pain [15]. Therapeutic modalities such as ultrasound and electrical stimulation can be tried for pain control but have no proven efficacy for long-term recovery. In addition, cervical traction done either manually (by a physical therapist) or with a mechanical unit (prescribed for home use) may be tried if there are no contraindications (i.e., fracture). Educational videos that make recommendations about posture, return to activity, exercise, and pain relief methods may help reduce rates of persistent symptoms at 6 months after injury [16].
Strengthening and stretching exercises for muscles with a tendency for tightness should be used in conjunction with the aforementioned techniques. Muscle imbalances must be addressed, and weak muscle groups such as the scapular stabilizers (middle-lower trapezius, serratus anterior, and levator scapulae) should be strengthened. This is typically done after muscles with a tendency for tightness (upper trapezius, sternocleidomastoid, scalenes, latissimus dorsi, and pectoralis major and minor) are stretched [17]. Cumulative data suggest that such an approach to cervical sprain injuries produces both long- and short-term benefits [9]. The overall treatment goal is to achieve an independent, customized home exercise program so that the patient can become active in his or her treatment [17]. An exercise protocol targeting shoulder and neck muscle strength and endurance was effective in decreasing chronic neck pain and disability in 180 female police officers [18].
Evaluation of the home or work environment by an occupational therapist can also be of benefit. Specifically, ergonomic alterations, such as the use of a telephone headrest and document holders, may aid in recovery.
Procedures
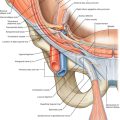
Trigger point injections are a reasonable adjunct to decrease pain so that patients may participate in physical therapy. A meta-analysis in 2010 stated that lidocaine injections into myofascial trigger points appear to be effective [19]. The upper trapezius, scalenes, and semispinalis capitis are the most common muscles to develop trigger points after acceleration-deceleration injuries. Other trigger points tend to arise in the splenius capitis, longus capitis, and longus colli after such injuries [20].
Botulinum toxin injections were initially thought to be effective for chronic cervical pain causing headaches [21]; however, there is more recent evidence that botulinum toxin A is not superior to saline injection for chronic mechanical neck pain [19].
Facet injections, epidural injections, and cervical traction may be instituted for conditions such as cervical radiculopathy and facet syndrome.
Surgery
Surgery is not indicated.
Potential Disease Complications
Similar to other grade I soft tissue strains, this injury will heal within 6 weeks. As such, there are no significant complications because this is not a permanent injury. There is research to suggest that the initial level of pain and degree of loss of cervical spine range of motion directly correlate with a poorer prognosis [22]. In addition, older age, lower educational achievement, part-time employment, preexisting neck or low back pain, and previous whiplash injury are associated with a significantly worse outcome. Of note, continuing litigation is associated with more severe pain [23].
Potential Treatment Complications
Analgesics and nonsteroidal anti-inflammatory drugs have well-known side effects that most commonly affect the gastric, hepatic, and renal systems. Muscle relaxants and low-dose tricyclic antidepressants can cause sedation. Overly aggressive manipulation or manipulation done when there is a concomitant unidentified injury (i.e., fracture) may result in serious injury. Injections are rarely associated with infection and allergic reactions to the medications used.
Interestingly, there is a correlation between the patient’s perception of the severity of the initial injury and the expectations for recovery [24]. It is for that reason that patient education is a significant focus in the treatment of cervical strain, and therefore lack of education may have negative effects. Thus far, a meta-analysis in 2012 has not shown scientifically that education is truly beneficial [25].