CASE 6
Jason, a 6-year-old boy who lives on a farm, has convinced his parents that he should be allowed to take care of the chicks that are in the hay loft area of the barn. He is intrigued with this brood of chicks and spends hours just lying down in the hay to watch them or dragging hay over to their nest. When he is not in the barn, Jason is “helping” his mother with the new garden. After several weeks of this regimen, Jason started having difficulty breathing and seemed to “always be coughing.” The parents took him to their family physician, who had already treated Jason for a severe diaper rash (Candida albicans) when he was an infant and over the past few years for numerous severe bacterial infections.
The physician ordered several tests, including a complete blood cell count and differential, total serum immunoglobulins, immunization antigen titer, T cell function test, and a bronchoalveolar lavage to use for culture. The white blood cell count showed a mild leukocytosis, but the differential indicated a normal percentage of each cell type. Total IgG was normal for the pediatric population (see Appendix), as was the antibody titer to immunization antigens. T cell function was normal. An inquiry into Jason’s family revealed that he had three older sisters and two brothers, none of whom had presented with clinical symptoms analogous to those for which Jason’s parents had sought medical attention. How would you proceed?
QUESTIONS FOR GROUP DISCUSSION
RECOMMENDED APPROACH
Implications/Results of Laboratory Investigation
Laboratory tests revealed a mild elevation in white blood cell count, normal differential, normal serum immunoglobulins, and normal B cell and T cell function tests. These tests rule out obvious B cell and T cell development disorders (see Cases 2 and 3). It is reasonable to conclude that Jason’s infections are not due to defects in adaptive immunity. As well, because the complete blood cell count and differential were normal, a deficiency in development of cell population(s) in the innate immune system can also be ruled out.
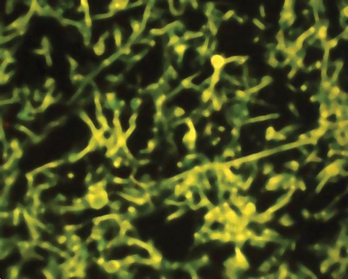
Culture indicated an infection with Aspergillus fumigatus. Infection is generally acquired from breathing in Aspergillus conidia (spores), which are widely distributed in nature, including hay lofts and garden soil. In immunocompromised individuals these infections can give rise to aspergillosis (Fig. 6-1). Individuals with normal numbers and function of phagocytes and CD4+ T cells can usually overcome these infections
DIAGNOSIS
Jason was diagnosed with chronic granulomatous disease. Because some NADPH oxidase defects are X linked, the flow cytometry test for NADPH oxidase activity was extended to Jason’s mother, sisters, and brothers. Only his 12-year-old brother showed evidence for defective NADPH oxidase function. Interestingly, blood cells from his mother and one sister showed mixed populations of neutrophils, with about 50% exhibiting a normal respiratory burst and 50% not doing so. Females carry two X chromosomes, one of which is randomly inactivated in all cells. Therefore, females who are carriers but do not express the disease have a mutated gene on only one X chromosome. A normal gene is expressed in about half the cells and a defective gene in the other half. Thus “functionally normal” females (carriers) are, in fact, genetic mosaics.
ETIOLOGY: CHRONIC GRANULOMATOUS DISEASE
Chronic granulomatous disease (CGD), one of the more common immunodeficiencies that affects innate immunity, is characterized by the absence of a respiratory burst and associated ROIs due to a defective subunit in the multi-subunit NADPH oxidase enzyme complex. In the resting phagocyte, some of the subunits are distributed in the plasma membrane; others are in the cytosol. Phagocytosis triggers subunit assembly on the phagocytic vacuole, a respiratory burst, and production of ROIs (see Fig. 4-1).