Procedure 59 Pyrocarbon Implant Arthroplasty of the Proximal Interphalangeal and Metacarpophalangeal Joints
![]() See Video 42: Pyrocarbon Implant Arthroplasty (Proximal Interphalangeal Joint)
See Video 42: Pyrocarbon Implant Arthroplasty (Proximal Interphalangeal Joint)
See Video 43: Pyrocarbon Implant Arthroplasty (Metacarpophalangeal Joint)
Indications
 Painful osteoarthritis of the proximal interphalangeal (PIP) and metacarpophalangeal (MCP) joints is found.
Painful osteoarthritis of the proximal interphalangeal (PIP) and metacarpophalangeal (MCP) joints is found.
 The patient should understand that normal full motion of the joint cannot be restored; therefore, surface replacement arthroplasty should be performed when the arthritic pain has become intolerable.
The patient should understand that normal full motion of the joint cannot be restored; therefore, surface replacement arthroplasty should be performed when the arthritic pain has become intolerable.
Surgical Anatomy
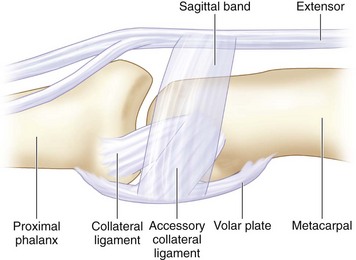
 The MCP joints of the fingers are condylar joints (Fig. 59-1), and specific MCP pyrocarbon implants are designed to mirror the anatomic construct. At the MCP joint, excellent soft tissue support and stability provided by the intermetacarpal ligaments give its stable construct. The best indication for pyrocarbon implant arthroplasty is an osteoarthritic MCP joint. Unfortunately, this situation is not often encountered. We generally do not recommend placing pyrocarbon implants in the rheumatoid hand because of the lack of adequate ligamentous support.
The MCP joints of the fingers are condylar joints (Fig. 59-1), and specific MCP pyrocarbon implants are designed to mirror the anatomic construct. At the MCP joint, excellent soft tissue support and stability provided by the intermetacarpal ligaments give its stable construct. The best indication for pyrocarbon implant arthroplasty is an osteoarthritic MCP joint. Unfortunately, this situation is not often encountered. We generally do not recommend placing pyrocarbon implants in the rheumatoid hand because of the lack of adequate ligamentous support.
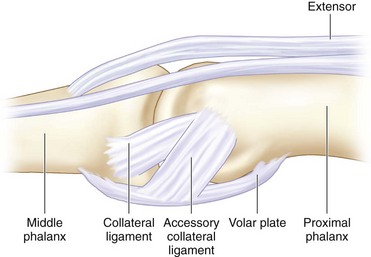
 The PIP joints for the fingers are ginglymoid joints that function essentially as hinge joints (Fig. 59-2). Destruction of the PIP joints often weakens the soft tissue support around the joints and may not be sufficiently tight to stabilize the pyrocarbon implants.
The PIP joints for the fingers are ginglymoid joints that function essentially as hinge joints (Fig. 59-2). Destruction of the PIP joints often weakens the soft tissue support around the joints and may not be sufficiently tight to stabilize the pyrocarbon implants.
 Preserving bone and collateral ligament origins and insertions helps stabilize the arthroplasty.
Preserving bone and collateral ligament origins and insertions helps stabilize the arthroplasty.
Exposures
MCP Joint Approach
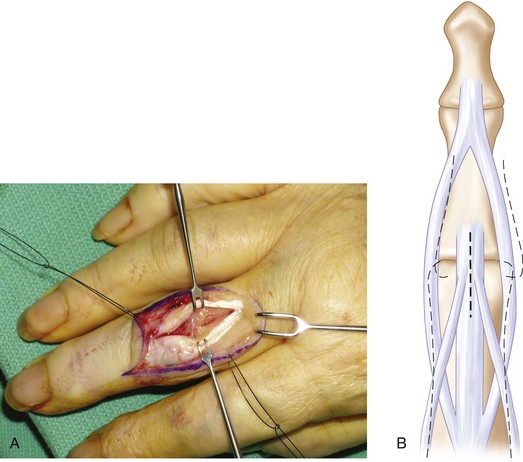
 A dorsal lazy S-shaped incision is made over the MCP joint for single joint replacement (Fig. 59-3A and B).
A dorsal lazy S-shaped incision is made over the MCP joint for single joint replacement (Fig. 59-3A and B).
 If there is no subluxation of the extensor mechanism, it can be split in the midline to expose the joint capsule. We prefer to incise the radial sagittal band to expose the joint so that the extensor tendon is not disrupted (Fig. 59-3C). The incised sagittal band should be imbricated to centralize the extensor mechanism at the conclusion of the procedure.
If there is no subluxation of the extensor mechanism, it can be split in the midline to expose the joint capsule. We prefer to incise the radial sagittal band to expose the joint so that the extensor tendon is not disrupted (Fig. 59-3C). The incised sagittal band should be imbricated to centralize the extensor mechanism at the conclusion of the procedure.
PIP Joint Approach
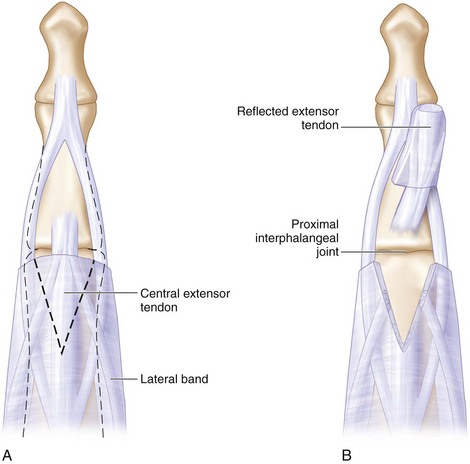
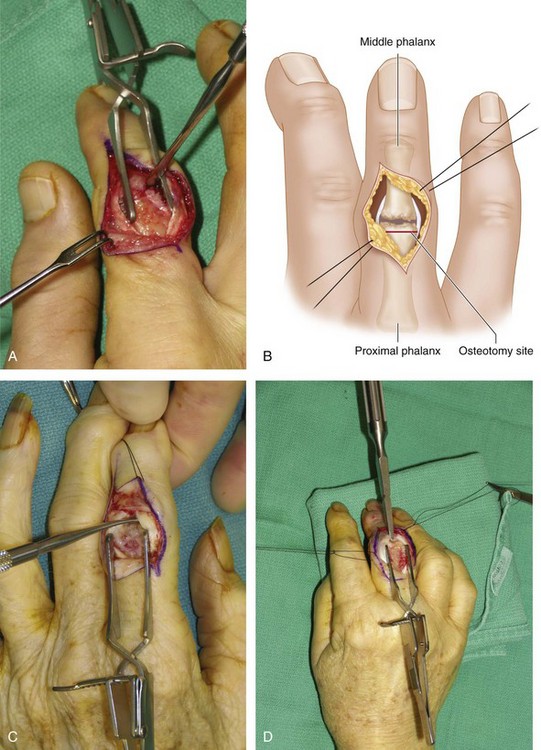
 The PIP joint is approached using a lazy S-shaped incision (Fig. 59-4), which provides wide exposure of the joint.
The PIP joint is approached using a lazy S-shaped incision (Fig. 59-4), which provides wide exposure of the joint.
 Two incisions may be used to expose the extensor mechanism.
Two incisions may be used to expose the extensor mechanism.
Procedure
PIP Joint Arthroplasty
Step 1
 The manufacturer’s manual recommends placing the starter awl first to make the tunnel ready for broaching. However, the osteoarthritic PIP joint is usually very tight, and getting precise placement of the awl is difficult. We have modified this key step by making a freehand cut of the head of the proximal phalanx first, which will fully expose the medullary cavity for precise broaching. Experience is necessary to avoid too much head resection, cutting just at the distal neck of the proximal phalanx (Fig. 59-7A to D).
The manufacturer’s manual recommends placing the starter awl first to make the tunnel ready for broaching. However, the osteoarthritic PIP joint is usually very tight, and getting precise placement of the awl is difficult. We have modified this key step by making a freehand cut of the head of the proximal phalanx first, which will fully expose the medullary cavity for precise broaching. Experience is necessary to avoid too much head resection, cutting just at the distal neck of the proximal phalanx (Fig. 59-7A to D).
Step 2
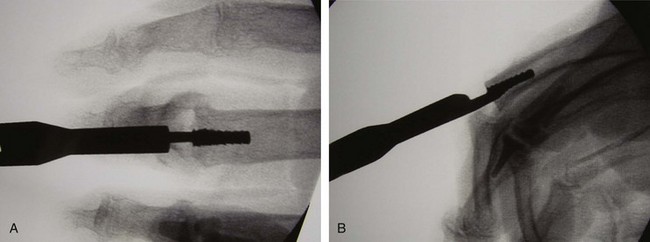
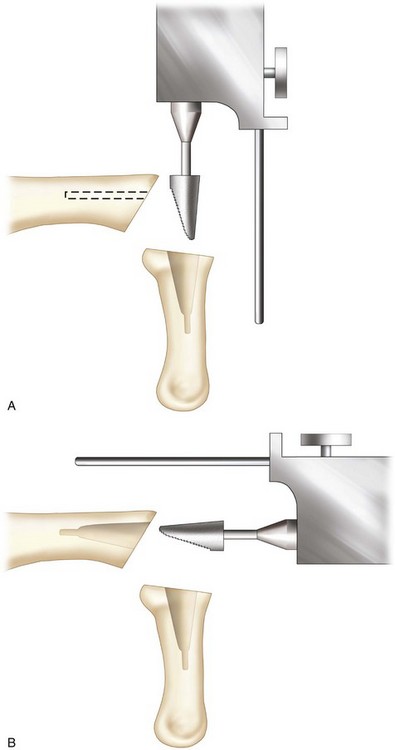
 A series of broaches are sequentially inserted into the proximal phalanx, starting with a no. 10 broach and increasing to the largest broach that can be accommodated within the medullary canal. The broach must be fully inserted into the medullary canal to fully accommodate the implant, which can be confirmed fluoroscopically (Fig. 59-8A and B).
A series of broaches are sequentially inserted into the proximal phalanx, starting with a no. 10 broach and increasing to the largest broach that can be accommodated within the medullary canal. The broach must be fully inserted into the medullary canal to fully accommodate the implant, which can be confirmed fluoroscopically (Fig. 59-8A and B).
Step 3
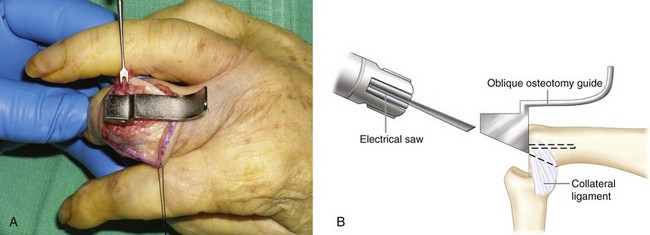
 An oblique cutting guide is then placed into the cut proximal phalanx to complete the volar oblique osteotomy (Fig. 59-9A and B). The proximal phalanx is now ready to accommodate the trial proximal phalanx implant. The pyrocarbon implant is press-fit, and cement is not used.
An oblique cutting guide is then placed into the cut proximal phalanx to complete the volar oblique osteotomy (Fig. 59-9A and B). The proximal phalanx is now ready to accommodate the trial proximal phalanx implant. The pyrocarbon implant is press-fit, and cement is not used.
Step 3 Pearls
The PIP pyrocarbon implant components can be mixed one size up or one size down. For example, a no. 30 proximal implant may fit with a no. 20 distal implant, and vice versa.
The middle phalanx can be difficult to broach to a larger size. Therefore, the size of the distal component is often one size down from the proximal component.
Step 5
Procedure
MCP Joint Arthroplasty
Step 1
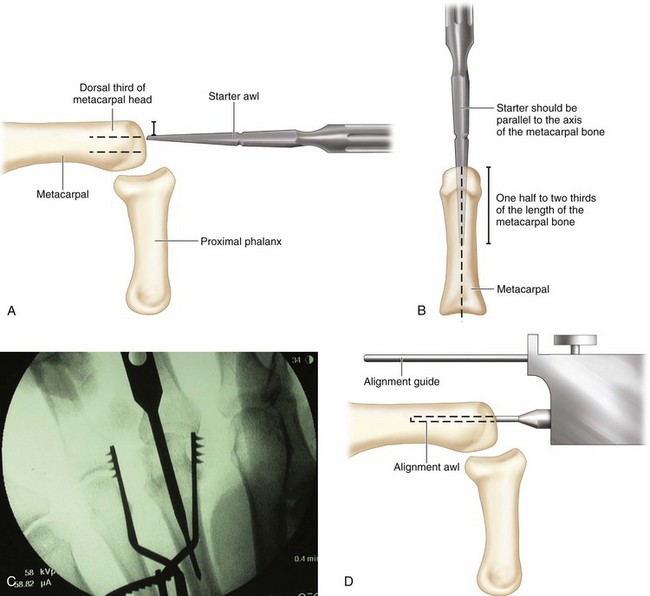
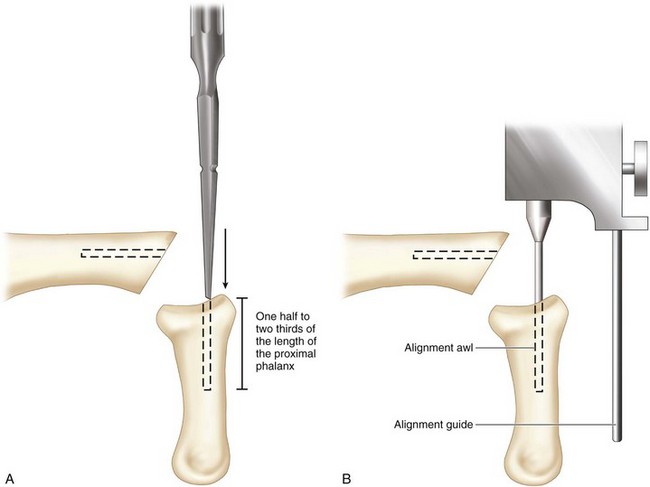
 The sequence of steps for the MCP joint arthroplasty is similar to that for PIP joint arthroplasty. A starter awl enters the metacarpal head one third of the distance from the dorsal cortex and slightly ulnar to the midline and can be advanced to one half or two thirds of the metacarpal bone length (Fig. 59-11A to D). The implant fits the anatomic shape of the head of the metacarpal, and the cam design of the implant requires the center of axis to enter one third from the dorsal cortex. The proximal implant has a condylar shape, and its stem will reside more dorsally from the midaxis of the joint.
The sequence of steps for the MCP joint arthroplasty is similar to that for PIP joint arthroplasty. A starter awl enters the metacarpal head one third of the distance from the dorsal cortex and slightly ulnar to the midline and can be advanced to one half or two thirds of the metacarpal bone length (Fig. 59-11A to D). The implant fits the anatomic shape of the head of the metacarpal, and the cam design of the implant requires the center of axis to enter one third from the dorsal cortex. The proximal implant has a condylar shape, and its stem will reside more dorsally from the midaxis of the joint.
Step 1 Pearls
Radial positioning of the metacarpal component should be avoided because this will further increase the radial deviating moment arm and contribute to ulnar drift. Fluoroscopy must be used liberally to ensure that all the instruments are in the precise location to permit perfect seating of the implant.
Step 2
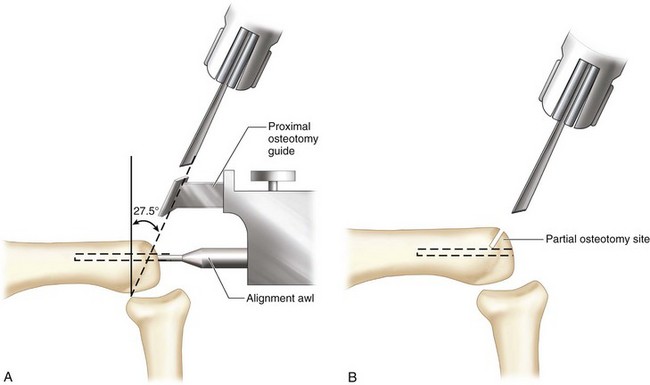
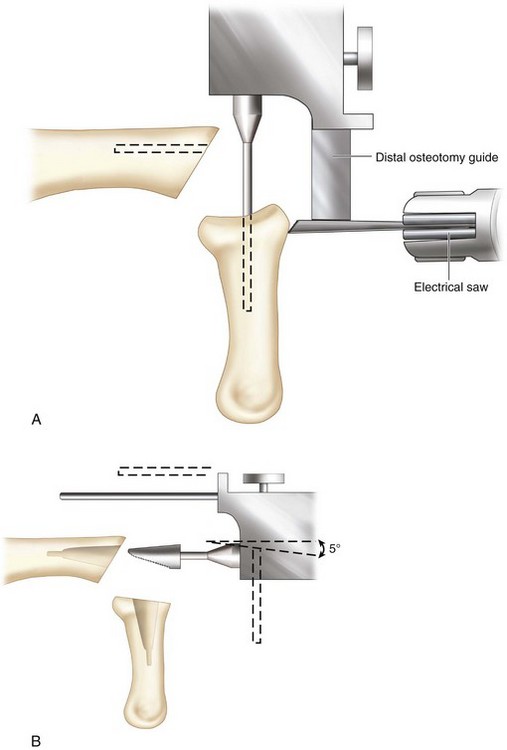
 A proximal osteotomy is made using a proximal osteotomy guide, which has a 27.5-degree distal tilted axial slot for the saw blade (Fig. 59-12A). A conservative osteotomy 1.5 mm distal to the collateral ligament attachment site is recommended to protect the collateral ligaments. The osteotomy is partially made over the dorsal cortex, and complete osteotomy is performed freehand after removal of the alignment guide (Fig. 59-12B).
A proximal osteotomy is made using a proximal osteotomy guide, which has a 27.5-degree distal tilted axial slot for the saw blade (Fig. 59-12A). A conservative osteotomy 1.5 mm distal to the collateral ligament attachment site is recommended to protect the collateral ligaments. The osteotomy is partially made over the dorsal cortex, and complete osteotomy is performed freehand after removal of the alignment guide (Fig. 59-12B).
Step 3
Step 5
 A broach is inserted as described previously (Fig. 59-15A and B). Mismatch is not permitted between the proximal and distal components of the implant in MCP joint pyrocarbon arthroplasty.
A broach is inserted as described previously (Fig. 59-15A and B). Mismatch is not permitted between the proximal and distal components of the implant in MCP joint pyrocarbon arthroplasty.
Step 6
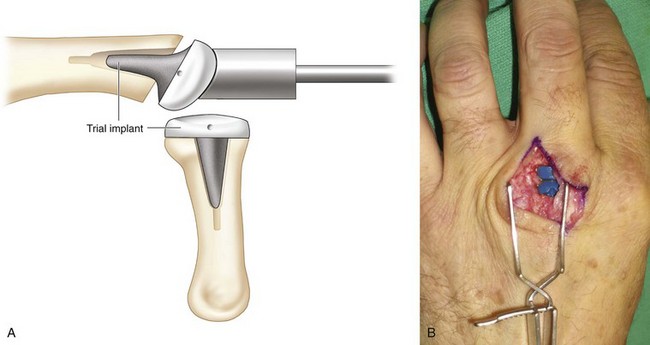
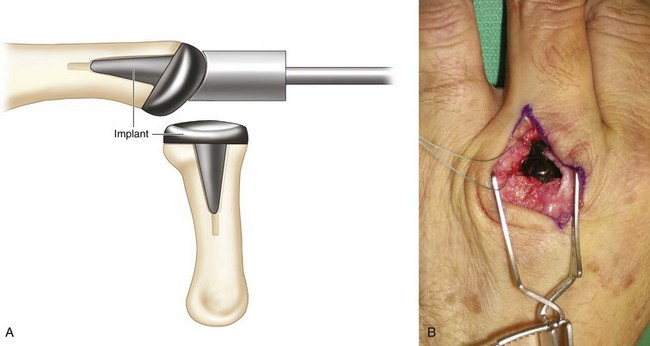
 A trial implant is inserted using a proximal and a distal impactor (Fig. 59-16A and B). The implant is press-fit into the medullary cavity by tapping it in gently (Fig. 59-17A and B).
A trial implant is inserted using a proximal and a distal impactor (Fig. 59-16A and B). The implant is press-fit into the medullary cavity by tapping it in gently (Fig. 59-17A and B).
Postoperative Care and Expected Outcomes
 The joint should be kept in extension for 3 weeks after the operation to consolidate the soft tissue support.
The joint should be kept in extension for 3 weeks after the operation to consolidate the soft tissue support.
 One week after the operation, flexion and extension exercises are started in a dynamic splint. A static resting splint can be worn at night for 2 months after the 3-week exercise program.
One week after the operation, flexion and extension exercises are started in a dynamic splint. A static resting splint can be worn at night for 2 months after the 3-week exercise program.
 Expected outcomes of this procedure include improvement in pain, improved aesthetic appearance of the hand and fingers, increased ability to perform activities of daily living, improved key pinch strength, minimal change in active arc of motion, and minimal improvement in grip strength.
Expected outcomes of this procedure include improvement in pain, improved aesthetic appearance of the hand and fingers, increased ability to perform activities of daily living, improved key pinch strength, minimal change in active arc of motion, and minimal improvement in grip strength.
Case Studies
 Figure 59-19 (A to F) shows the long-term result of a PIP joint pyrocarbon implant arthroplasty in a 53-year-old man with severe osteoarthritis and pain over the left index finger PIP joint limiting motion. The patient refused PIP joint fusion; therefore, a pyrocarbon implant arthroplasty was performed.
Figure 59-19 (A to F) shows the long-term result of a PIP joint pyrocarbon implant arthroplasty in a 53-year-old man with severe osteoarthritis and pain over the left index finger PIP joint limiting motion. The patient refused PIP joint fusion; therefore, a pyrocarbon implant arthroplasty was performed.
 A 70-year-old woman presented with right index finger severe osteoarthritis and pain. She refused PIP joint fusion and opted for a pyrocarbon implant arthroplasty to preserve some motion (Fig. 59-20A). About 18 months after pyrocarbon arthroplasty, she began to experience chronic pain and swelling related to instability and recurrent dislocation of the joint that she was always able to reduce herself (Fig. 59-20B). Because of her persistent symptoms related to the recurrent dislocation, the implant was removed, and a PIP joint fusion was performed. This case illustrates that pyrocarbon arthroplasty can cause long-term problems relating to implant subsidence and dislocation. These complications must be explained carefully to the patient. Because there is no better alternative, and silicone implant for the PIP joint is often associated with joint instability, the pyrocarbon arthroplasty option is still a reasonable solution in lieu of joint fusion.
A 70-year-old woman presented with right index finger severe osteoarthritis and pain. She refused PIP joint fusion and opted for a pyrocarbon implant arthroplasty to preserve some motion (Fig. 59-20A). About 18 months after pyrocarbon arthroplasty, she began to experience chronic pain and swelling related to instability and recurrent dislocation of the joint that she was always able to reduce herself (Fig. 59-20B). Because of her persistent symptoms related to the recurrent dislocation, the implant was removed, and a PIP joint fusion was performed. This case illustrates that pyrocarbon arthroplasty can cause long-term problems relating to implant subsidence and dislocation. These complications must be explained carefully to the patient. Because there is no better alternative, and silicone implant for the PIP joint is often associated with joint instability, the pyrocarbon arthroplasty option is still a reasonable solution in lieu of joint fusion.
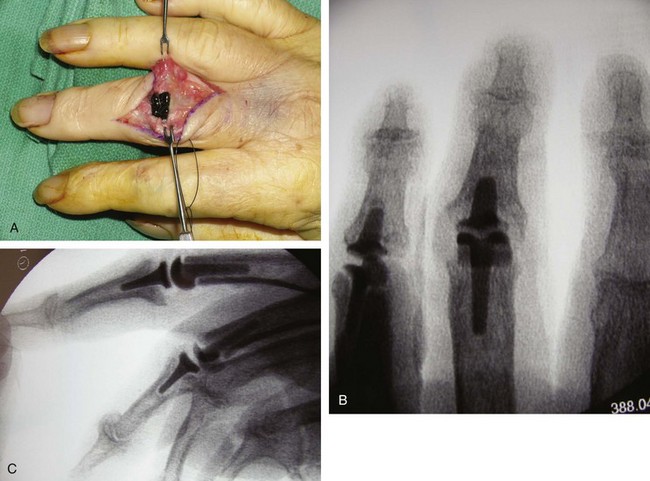
 A 59-year-old woman with a history of severe osteoarthritis of all finger joints presented for pyrocarbon arthroplasty of her right ring finger PIP joint (Fig. 59-21A). Two weeks after the arthroplasty, the joint was dislocated (Fig. 59-21B). The joint was reduced, and an external fixator was used to maintain reduction for 6 weeks (Fig. 59-21C). After removal of the external fixator, the joint was stable and had good motion (Fig. 59-21D). This case illustrates that poor ligamentous support in the PIP joint is unable to maintain joint reduction after implant arthroplasty. The use of an external fixator to reduce the joint permits tightening of the ligament support and can remedy the dislocation complication, if this complication is detected within the first 2 weeks after surgery.
A 59-year-old woman with a history of severe osteoarthritis of all finger joints presented for pyrocarbon arthroplasty of her right ring finger PIP joint (Fig. 59-21A). Two weeks after the arthroplasty, the joint was dislocated (Fig. 59-21B). The joint was reduced, and an external fixator was used to maintain reduction for 6 weeks (Fig. 59-21C). After removal of the external fixator, the joint was stable and had good motion (Fig. 59-21D). This case illustrates that poor ligamentous support in the PIP joint is unable to maintain joint reduction after implant arthroplasty. The use of an external fixator to reduce the joint permits tightening of the ligament support and can remedy the dislocation complication, if this complication is detected within the first 2 weeks after surgery.
Chung KC, Ram AN, Shauver MJ. Outcomes of pyrolytic carbon arthroplasty for the proximal interphalangeal joint. Plast Reconstr Surg. 2009;123:1521-1532.
Cook SD, Beckenbaugh RD, Redondo J, et al. Long-term follow-up of pyrolytic carbon metacarpophalangeal implants. J Bone Joint Surg [Am]. 1999;81:635-648.
Parker W, Moran SL, Hormel KB, et al. Nonrheumatoid metacarpophalangeal joint arthritis. Unconstrained pyrolytic carbon implants: indications, technique, and outcomes. Hand Clin. 2006;22:183-193.
Squitieri L, Chung KC. A systematic review of outcomes and complications of vascularized toe joint transfer, silicone arthroplasty and pyrocarbon arthroplasty for post-traumatic joint reconstruction of the finger. Plast Reconstr Surg. 2008;121:1697-1707.