CHAPTER 59 Fundamentals of Obstetric Anesthesia
1 What are the cardiovascular adaptations to pregnancy?
The major cardiovascular adaptations to pregnancy are summarized in Table 59-1. During pregnancy cardiac examination reveals a shift of the apex cephalad and to the left. By the second half of pregnancy the third heart sound can commonly be detected on auscultation, and a fourth heart sound can be heard in up to 16% of patients. A grade I–II systolic murmur can often be heard secondary to increased blood flow. Chest x-ray film usually reveals an enlarged cardiac silhouette.
| Oxygen consumption | Increase 30%–40% |
2 What hematologic changes accompany pregnancy?
Table 59-2 summarizes the hematologic changes of pregnancy. Plasma volume increases from 40 to 70 ml/kg near term, and blood volume increases by 1000 to 1500 ml. The relative anemia of pregnancy is caused by a relatively slower rise in red blood cell mass compared to plasma volume. Maternal anemia, usually the result of iron deficiency, occurs when the hemoglobin falls below 10 g or the hematocrit is <30%.
| Plasma volume |
PTT, Partial thromboplastin time; PT, prothrombin time.
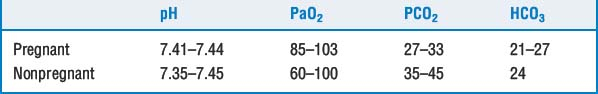
3 What pulmonary and respiratory changes occur with pregnancy?
Table 59-3 summarizes the respiratory changes of pregnancy. Pregnancy leads to capillary engorgement and edema of the respiratory tract. The mucosa also becomes friable, which may lead to bleeding with manipulation or trauma. These changes in the airway and the enlarged breasts of the pregnant patient make laryngoscopy difficult. Adding to the problem, the increased oxygen consumption and decreased functional residual capacity (FRC) make the laboring patient more prone to hypoxia and rapid desaturation during apneic periods.
| Minute ventilation | 50% increase (can go up to 140% of pre pregnancy values in first stage of unmedicated labor and up to 200% in the second stage) |
| Alveolar ventilation | 70% increase |
| Tidal volume | 40% increase |
| Oxygen consumption | 20% increase |
| Respiratory rate | 15% increase |
| Dead space | No change |
| Lung compliance | No change |
| Residual volume | 29% decrease |
| Vital capacity | No change |
| Total lung capacity | 5% decrease |
| Functional residual capacity | 15%–20% decrease |
| FEV1 | No change |
FEV1, Forced expiratory volume in 1 second.
13 How quickly do the physiologic alterations of pregnancy return to normal after delivery?
 FRC and residual volume rapidly return to normal. Many of the pulmonary changes caused by mechanical compression by the gravid uterus resolve quickly. Alveolar ventilation returns to baseline by 4 weeks postpartum, and there is a rise in maternal PCO2 as the progesterone levels decrease.
FRC and residual volume rapidly return to normal. Many of the pulmonary changes caused by mechanical compression by the gravid uterus resolve quickly. Alveolar ventilation returns to baseline by 4 weeks postpartum, and there is a rise in maternal PCO2 as the progesterone levels decrease.15 What are the three stages of labor?
 Stage 1. Cervical dilation and effacement. It begins with the onset of regular, painful contractions and ends when dilation of the cervix is complete (or 10 cm). The latent phase is characterized by slow cervical dilation and effacement. The active phase is defined as the period of progressive cervical dilation, which usually begins around 4 to 5 cm.
Stage 1. Cervical dilation and effacement. It begins with the onset of regular, painful contractions and ends when dilation of the cervix is complete (or 10 cm). The latent phase is characterized by slow cervical dilation and effacement. The active phase is defined as the period of progressive cervical dilation, which usually begins around 4 to 5 cm.17 What factors influence uteroplacental perfusion?
 Aortocaval compression: When lying supine, the gravid uterus compresses the abdominal aorta, decreasing uteroplacental perfusion (UPP).
Aortocaval compression: When lying supine, the gravid uterus compresses the abdominal aorta, decreasing uteroplacental perfusion (UPP).18 How should hypotension associated with spinal anesthesia be treated in a cesarean section or laboring patient?
19 What is the role of intravenous fluid preloading before regional anesthesia for cesarean delivery?
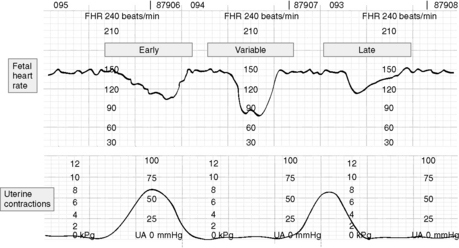
22 What is the significance of fetal heart rate decelerations?
 Early decelerations in FHR are caused by head compressions (vagal stimulation), are uniform in shape, begin near the onset of a uterine contraction with its nadir at the same time as the peak of the contraction, and are benign.
Early decelerations in FHR are caused by head compressions (vagal stimulation), are uniform in shape, begin near the onset of a uterine contraction with its nadir at the same time as the peak of the contraction, and are benign. Variable decelerations are caused by umbilical cord compression and are nonuniform in shape. They are abrupt in onset and cessation. The decrease is >15 beats/min. They last longer than 15 seconds but less than 2 minutes. Although they usually do not reflect fetal acidosis, repetitive variable decelerations can lead to fetal hypoxia and acidosis.
Variable decelerations are caused by umbilical cord compression and are nonuniform in shape. They are abrupt in onset and cessation. The decrease is >15 beats/min. They last longer than 15 seconds but less than 2 minutes. Although they usually do not reflect fetal acidosis, repetitive variable decelerations can lead to fetal hypoxia and acidosis. Late decelerations are caused by uteroplacental insufficiency. They are uniform in shape. The onset and return to baseline are gradual. They often begin just after the onset of a contraction, with their nadir and recovery after the peak and recovery of the contraction. These decelerations are associated with maternal hypotension, hypertension, diabetes, preeclampsia, or intrauterine growth retardation. These are ominous patterns and indicate that the fetus is unable to maintain normal oxygenation and pH in the face of decreased blood flow.
Late decelerations are caused by uteroplacental insufficiency. They are uniform in shape. The onset and return to baseline are gradual. They often begin just after the onset of a contraction, with their nadir and recovery after the peak and recovery of the contraction. These decelerations are associated with maternal hypotension, hypertension, diabetes, preeclampsia, or intrauterine growth retardation. These are ominous patterns and indicate that the fetus is unable to maintain normal oxygenation and pH in the face of decreased blood flow.The treatment for nonreassuring neonatal heart rate changes involves administering oxygen to the mother, maintaining maternal blood pressure, and placing the parturient in the left uterine displacement position (Figure 59-1).
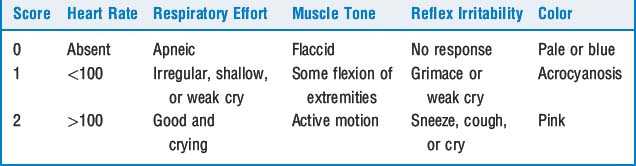
23 What is the Apgar score?
The Apgar score is the most widely accepted and used system to evaluate the neonate, determine which neonates need resuscitation, and measure the success of resuscitation (Table 59-5). The score evaluates heart rate, respiratory effort, muscle tone, reflex irritability, and color, with heart rate and respiratory effort being the most important criteria. Each variable is given a score of 0 to 2, for a total score of 10. The Apgar score is measured at 1 and 5 minutes and then at 10 and 20 minutes as resuscitative efforts are continued. A score of 0 to 3 indicates a severely depressed neonate, whereas a score of 7 to 10 is considered normal.
24 Describe the management of the pregnant patient undergoing nonobstetric surgery
KEY POINTS: Fundamentals of Obstetric Anesthesia 
1. American College of Obstetricians and Gynecologists. Obstetric analgesia and anesthesia. ACOG Practice Bulletin No. 36. 2002.
2. Conklin K.A. Physiologic changes of pregnancy. In Chesnut D.H., editor: Obstetric anesthesia: principles and practice, ed 3, St. Louis: Mosby, 2004.
3. Cooper D.W., Carpenter M., Mowbray P., et al. Fetal and maternal effects of phenylephrine and ephedrine during spinal anesthesia for cesarean delivery. Anesthesiology. 2002;97:1582-1590.
4. Cyna A.M., Andrew M., Emmett R.S., et al. Techniques for preventing hypotension during spinal anaesthesia for caesarean section. Cochrane Database Syst Rev. 4, 2006. CDOO2251
5. Lee A., Ngan Kee W.D., Gin T. Prophylactic ephedrine prevents hypotension during spinal anesthesia for cesarean delivery but does not improve neonatal outcome: a quantitative systematic review. Can J Anaesth. 2002;49:588-599.
6. Macones G.A., Hankins G.D., Spong C.Y., et al. The 2008 National Institute of Child Health and Human Development workshop report on electronic fetal monitoring: update on definitions, interpretation, and research guidelines. Obstet Gynecol. 2008;112:661-666.
7. Practice Guidelines for Obstetric Anesthesia. an updated report by the American Society of Anesthesiologists. www.asahq.org. Task Force on Obstetric Anesthesia (last amended on October 18, 2006)