Procedure 58 Skier’s Thumb
Repair of Acute Thumb Metacarpophalangeal Joint Ulnar Collateral Ligament Injury
![]() See Video 40: Repair of Acute Thumb MCP Joint Ulnar Collateral Ligament Injury
See Video 40: Repair of Acute Thumb MCP Joint Ulnar Collateral Ligament Injury
See Video 41: Thumb Radial Collateral Ligament Repair
Examination/Imaging
Clinical Examination
 In the acute presentation, the patient typically has a swollen painful thumb MCP joint. Occasionally, a lump may be palpated on the ulnar side of the thumb MCP joint, representing the avulsed and retracted UCL stump.
In the acute presentation, the patient typically has a swollen painful thumb MCP joint. Occasionally, a lump may be palpated on the ulnar side of the thumb MCP joint, representing the avulsed and retracted UCL stump.
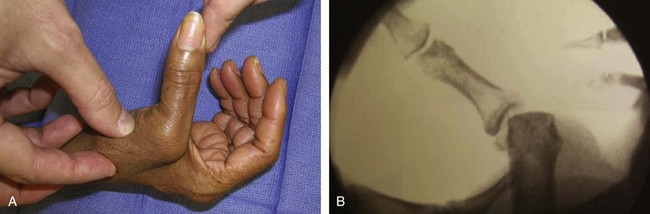
 Stress testing of the UCL is performed by applying a valgus force to the extended MCP joint while holding the head of the metacarpal fixed. If the joint deviates more than 30 degrees total or 15 degrees more than the contralateral uninjured thumb, it represents a complete UCL tear. A significant deviation in extension represents a more comprehensive injury that includes the dorsal capsule in addition to the UCL. A similar deviation of 30 degrees of flexion represents an injury to the UCL in isolation. If it deviates less than 25 degrees, it may represent a ligamentous strain that would be amenable to nonoperative treatment. (Fig. 58-1 shows clinical and fluoroscopic examination demonstrating significant ulnar collateral ligament laxity on stress testing.)
Stress testing of the UCL is performed by applying a valgus force to the extended MCP joint while holding the head of the metacarpal fixed. If the joint deviates more than 30 degrees total or 15 degrees more than the contralateral uninjured thumb, it represents a complete UCL tear. A significant deviation in extension represents a more comprehensive injury that includes the dorsal capsule in addition to the UCL. A similar deviation of 30 degrees of flexion represents an injury to the UCL in isolation. If it deviates less than 25 degrees, it may represent a ligamentous strain that would be amenable to nonoperative treatment. (Fig. 58-1 shows clinical and fluoroscopic examination demonstrating significant ulnar collateral ligament laxity on stress testing.)
Imaging
 Standard anteroposterior and lateral radiographs of the thumb should be obtained to check for an avulsion fracture of the proximal phalanx. Volar subluxation of the proximal phalanx suggesting a dorsal capsular tear that might need repair can be seen on the lateral radiograph. Comparison views of the opposite uninjured thumb can be obtained to ensure that subluxation is pathologic and not due to the patient’s inherent ligamentous laxity.
Standard anteroposterior and lateral radiographs of the thumb should be obtained to check for an avulsion fracture of the proximal phalanx. Volar subluxation of the proximal phalanx suggesting a dorsal capsular tear that might need repair can be seen on the lateral radiograph. Comparison views of the opposite uninjured thumb can be obtained to ensure that subluxation is pathologic and not due to the patient’s inherent ligamentous laxity.
 In the absence of a fracture, radiographic stress testing can be performed to evaluate joint laxity; however, this is not necessary because the clinical examination is usually sufficient. This may require a local anesthetic block in order for the patient to cooperate with the examination (see Fig. 58-1).
In the absence of a fracture, radiographic stress testing can be performed to evaluate joint laxity; however, this is not necessary because the clinical examination is usually sufficient. This may require a local anesthetic block in order for the patient to cooperate with the examination (see Fig. 58-1).
 In rare instances when the clinical examination is equivocal, magnetic resonance imaging or ultrasound can be used to assess the extent of a UCL tear.
In rare instances when the clinical examination is equivocal, magnetic resonance imaging or ultrasound can be used to assess the extent of a UCL tear.
Surgical Anatomy
 The MCP joint has characteristics of both a condyloid and a ginglymus joint, which allow a relatively large range of motion. Consequently, there is little inherent stability in the bony architecture.
The MCP joint has characteristics of both a condyloid and a ginglymus joint, which allow a relatively large range of motion. Consequently, there is little inherent stability in the bony architecture.
 Stability of the joint depends largely on a complex arrangement of ligamentous and musculotendinous structures.
Stability of the joint depends largely on a complex arrangement of ligamentous and musculotendinous structures.
 The ulnar collateral ligament is composed of two units. The proper UCL originates on the ulnar lateral condyle of the metacarpal and traverses obliquely to insert on the volar third of the ulnar proximal phalanx. It is tight in flexion and loose in extension. The accessory UCL originates volar to the proper collateral ligament and inserts on the ulnar sesamoid and volar plate. It is tight in extension and loose in flexion.
The ulnar collateral ligament is composed of two units. The proper UCL originates on the ulnar lateral condyle of the metacarpal and traverses obliquely to insert on the volar third of the ulnar proximal phalanx. It is tight in flexion and loose in extension. The accessory UCL originates volar to the proper collateral ligament and inserts on the ulnar sesamoid and volar plate. It is tight in extension and loose in flexion.
 The adductor pollicis inserts on the ulnar sesamoid embedded in the volar plate. It has an aponeurosis that extends obliquely across the MCP joint, inserting into the extensor mechanism distal to the sagittal bands.
The adductor pollicis inserts on the ulnar sesamoid embedded in the volar plate. It has an aponeurosis that extends obliquely across the MCP joint, inserting into the extensor mechanism distal to the sagittal bands.
 A Stener lesion results from a forceful radial deviation of the proximal phalanx, resulting in a distal avulsion of the UCL from its insertion on the proximal phalanx. Because of the extensive radial deviation of the proximal phalanx, the UCL becomes displaced from its insertion point deep to the adductor aponeurosis and comes to lie superficial and proximal to the adductor aponeurosis, which prevents the ligament from anatomic alignment. The lesion is created with forced radial deviation of the proximal phalanx with displacement of the UCL superficial to the adductor aponeurosis to prevent its anatomic alignment (Fig. 58-2).
A Stener lesion results from a forceful radial deviation of the proximal phalanx, resulting in a distal avulsion of the UCL from its insertion on the proximal phalanx. Because of the extensive radial deviation of the proximal phalanx, the UCL becomes displaced from its insertion point deep to the adductor aponeurosis and comes to lie superficial and proximal to the adductor aponeurosis, which prevents the ligament from anatomic alignment. The lesion is created with forced radial deviation of the proximal phalanx with displacement of the UCL superficial to the adductor aponeurosis to prevent its anatomic alignment (Fig. 58-2).
 Branches of the superficial radial nerve often cross the operative field and need to be identified and protected.
Branches of the superficial radial nerve often cross the operative field and need to be identified and protected.
Exposures
 The lazy S-shaped skin incision is centered over the ulnar side of the MCP joint. It should start distally on the ulnar volar aspect of the proximal phalanx, curve over the joint, and continue proximally just ulnar to the extensor pollicis longus (EPL) tendon (Fig. 58-3).
The lazy S-shaped skin incision is centered over the ulnar side of the MCP joint. It should start distally on the ulnar volar aspect of the proximal phalanx, curve over the joint, and continue proximally just ulnar to the extensor pollicis longus (EPL) tendon (Fig. 58-3).
 The dissection is carried down through the subcutaneous tissue bluntly to protect branches of the superficial radial nerve, with elevation of full-thickness skin flaps dorsally and volarly. This should expose the EPL tendon, extensor hood, and adductor aponeurosis. Branches of the superficial radial nerve are often found in the operative field and need to be protected (Fig. 58-4).
The dissection is carried down through the subcutaneous tissue bluntly to protect branches of the superficial radial nerve, with elevation of full-thickness skin flaps dorsally and volarly. This should expose the EPL tendon, extensor hood, and adductor aponeurosis. Branches of the superficial radial nerve are often found in the operative field and need to be protected (Fig. 58-4).
 At this point, a mass of tissue may be seen at the proximal edge of the adductor aponeurosis. This represents a Stener lesion and consists of the retracted UCL.
At this point, a mass of tissue may be seen at the proximal edge of the adductor aponeurosis. This represents a Stener lesion and consists of the retracted UCL.
 The extensor hood is then incised just ulnar to the EPL tendon, leaving a cuff of tissue on the tendon for later repair. Although there is often scarring that can obliterate the tissue planes, the EPL can then be retracted radially, and the adductor aponeurosis is elevated from the underlying MCP joint capsule and reflected volarly. If a Stener lesion is not present, the torn end of the UCL should be found underneath the adductor aponeurosis.
The extensor hood is then incised just ulnar to the EPL tendon, leaving a cuff of tissue on the tendon for later repair. Although there is often scarring that can obliterate the tissue planes, the EPL can then be retracted radially, and the adductor aponeurosis is elevated from the underlying MCP joint capsule and reflected volarly. If a Stener lesion is not present, the torn end of the UCL should be found underneath the adductor aponeurosis.
 If the capsule is not already torn from the injury, an incision should be made in the capsule at the dorsoulnar aspect at the approximate junction of the dorsal capsule and the proper collateral ligament. The MCP joint is then examined for chondral injuries.
If the capsule is not already torn from the injury, an incision should be made in the capsule at the dorsoulnar aspect at the approximate junction of the dorsal capsule and the proper collateral ligament. The MCP joint is then examined for chondral injuries.
Pearls
Care must be taken during exposure to identify and protect branches of the superficial radial nerve that can often be found in this area (see Fig. 58-4).
It is often helpful to use retraction sutures to hold back the skin flaps during the procedure.
If a Stener lesion is not present, an incision in the dorsal MCP capsule is made at the dorsal margin of the UCL. Passing a blunt instrument such as a Freer elevator along the ulnar aspect of the proximal phalangeal base and the metacarpal head will confirm whether the lesion represents a distal avulsion (most commonly), a midsubstance tear, or a proximal avulsion from the metacarpal origin.
Procedure
Step 1: Preparation of the UCL and Insertion Site
 The reconstruction technique depends on the pathologic changes observed. Rarely, there is a midsubstance tear of the UCL. If this is found, it can be repaired primarily using a nonabsorbable braided 4-0 suture with interrupted figure-of-eight sutures.
The reconstruction technique depends on the pathologic changes observed. Rarely, there is a midsubstance tear of the UCL. If this is found, it can be repaired primarily using a nonabsorbable braided 4-0 suture with interrupted figure-of-eight sutures.
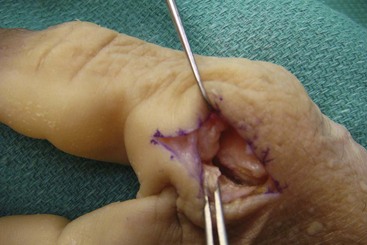
 More commonly, the ligament is avulsed from its distal insertion on the proximal phalanx and requires reattachment using either a pull-out suture (traditional) or bone anchors (the authors’ preferred method). In preparation for this, the torn end of the UCL must be mobilized by dissecting it free from adjacent soft tissue, scar, and hematoma (Fig. 58-5).
More commonly, the ligament is avulsed from its distal insertion on the proximal phalanx and requires reattachment using either a pull-out suture (traditional) or bone anchors (the authors’ preferred method). In preparation for this, the torn end of the UCL must be mobilized by dissecting it free from adjacent soft tissue, scar, and hematoma (Fig. 58-5).
 The insertion point of the UCL on the volar ulnar aspect of the proximal phalanx is prepared by clearing it of soft tissue with a curette. (In Fig. 58-6, the bone has been cleared of soft tissue and prepared for suture anchor placement. Forceps are holding the mobilized UCL.)
The insertion point of the UCL on the volar ulnar aspect of the proximal phalanx is prepared by clearing it of soft tissue with a curette. (In Fig. 58-6, the bone has been cleared of soft tissue and prepared for suture anchor placement. Forceps are holding the mobilized UCL.)
 Microsuture anchors preloaded with a 3-0/4-0 braided permanent suture are used. There are various anchors (both permanent and absorbable) that can be used; each contains a drill to create an appropriate pilot hole for the anchor.
Microsuture anchors preloaded with a 3-0/4-0 braided permanent suture are used. There are various anchors (both permanent and absorbable) that can be used; each contains a drill to create an appropriate pilot hole for the anchor.
 The pilot hole for the anchor is drilled at the prepared site just distal to the subchondral bone at the articular surface. The authors place two anchors. The first anchor targets the volar one third of the phalangeal base. Anchor placement, which is suitably volar to restore the insertion position of the UCL, is confirmed fluoroscopically. By doing this, if the initial anchor is found not to be sufficiently volar, additional dissection can be performed to place the second anchor appropriately. If the first anchor placement is acceptable, a second anchor is placed more dorsal to the first anchor.
The pilot hole for the anchor is drilled at the prepared site just distal to the subchondral bone at the articular surface. The authors place two anchors. The first anchor targets the volar one third of the phalangeal base. Anchor placement, which is suitably volar to restore the insertion position of the UCL, is confirmed fluoroscopically. By doing this, if the initial anchor is found not to be sufficiently volar, additional dissection can be performed to place the second anchor appropriately. If the first anchor placement is acceptable, a second anchor is placed more dorsal to the first anchor.
 The bone anchors are placed into the hole with the appropriate introducers, and tension is placed on the sutures to ensure solid fixation in the bone.
The bone anchors are placed into the hole with the appropriate introducers, and tension is placed on the sutures to ensure solid fixation in the bone.
Step 2: Reattachment
 The ends of the suture attached to the anchor are then brought through the distal end of the UCL in horizontal mattress fashion. The MCP joint is held in a neutral or slight ulnarly deviated position in the radioulnar plane, and the sutures are tied.
The ends of the suture attached to the anchor are then brought through the distal end of the UCL in horizontal mattress fashion. The MCP joint is held in a neutral or slight ulnarly deviated position in the radioulnar plane, and the sutures are tied.
 This repair is supplemented by suturing the distal volar aspect of the UCL to the volar plate. Additionally, sutures may be placed through the distal UCL and local tissue or periosteum.
This repair is supplemented by suturing the distal volar aspect of the UCL to the volar plate. Additionally, sutures may be placed through the distal UCL and local tissue or periosteum.
 If the dorsal capsule has been torn, it is repaired with 3-0 or 4-0 braided suture to prevent volar subluxation of the joint.
If the dorsal capsule has been torn, it is repaired with 3-0 or 4-0 braided suture to prevent volar subluxation of the joint.
 The MCP joint can be transfixed with a Kirschner wire by correcting palmar subluxation and establishing a slightly overcorrected ulnar-deviated position to prevent tension on the repair. Ideally, the MCP joint is first stabilized and then the sutures placed.
The MCP joint can be transfixed with a Kirschner wire by correcting palmar subluxation and establishing a slightly overcorrected ulnar-deviated position to prevent tension on the repair. Ideally, the MCP joint is first stabilized and then the sutures placed.
Step 2 Pearls
Be sure to identify and attach the UCL to its anatomic insertion point. If the ligament is reattached more distally or dorsally than its normal insertion point, MCP joint range of motion can be decreased.
Be sure to identify and repair dorsal capsule tears to reduce and prevent recurrent volar subluxation of the joint.
Step 3: Closure
Postoperative Care and Expected Outcomes
 Seven to 10 days after surgery, the skin sutures are removed, and the patient is placed in a short-arm thumb spica cast.
Seven to 10 days after surgery, the skin sutures are removed, and the patient is placed in a short-arm thumb spica cast.
 Four weeks after surgery, the cast and K-wire (if used) are removed. After 6 weeks of immobilization, the patient is referred to occupational therapy for a thumb spica splint and initiation of range-of-motion exercises.
Four weeks after surgery, the cast and K-wire (if used) are removed. After 6 weeks of immobilization, the patient is referred to occupational therapy for a thumb spica splint and initiation of range-of-motion exercises.
 Patients are encouraged to remove the splint and do flexion and extension range-of-motion exercises six to eight times a day. Any radially directed force that would stress the repair is avoided at this time.
Patients are encouraged to remove the splint and do flexion and extension range-of-motion exercises six to eight times a day. Any radially directed force that would stress the repair is avoided at this time.
 The splint is discontinued except for strenuous activities 2 weeks after the cast is removed.
The splint is discontinued except for strenuous activities 2 weeks after the cast is removed.
 After 8 weeks, strengthening exercises focusing on pinch and grip strength in the plane of the flexor pollicis longus (FPL) are initiated.
After 8 weeks, strengthening exercises focusing on pinch and grip strength in the plane of the flexor pollicis longus (FPL) are initiated.
 Unrestricted activity, including lateral pinch, is allowed after 12 weeks.
Unrestricted activity, including lateral pinch, is allowed after 12 weeks.
Pitfalls
Many patients develop transient neurapraxia of the branches of the superficial radial nerve owing to traction on the nerve during the procedure. This can result in numbness or tingling on the dorsal ulnar aspect of the thumb distal to the incision. This is usually self limiting and resolves over the first several weeks with progressive desensitization exercises.
Patients (and some therapists) must be cautioned against being too aggressive in pinch and grip strengthening early in the postoperative period to prevent attenuation of the repair.
Downey DJ, Moneim MS, Omer GE. Acute gamekeeper’s thumb: quantitative outcome of surgical repair. Am J Sports Med. 1995;23:222-226.
Katolik LI, Friedrich J, Trumble TE. Repair of acute ulnar collateral ligament injuries of the thumb metacarpophalangeal joint: a retrospective comparison of pull-out sutures and bone anchor techniques. Plast Reconstr Surg. 2008;122:1451-1456.
Kozin SH. Treatment of thumb ulnar collateral ligament ruptures with the Mitek bone anchor. Ann Plast Surg. 1995;35:1-5.
Weiland AJ, Berner SH, Hotchkiss RN, et al. Repair of acute ulnar collateral ligament injuries of the thumb metacarpophalangeal joint with an intraosseous suture anchor. J Hand Surg [Am]. 1997;22:585-591.