CHAPTER 58
Piriformis Syndrome
Rathi L. Joseph, DO; Joseph T. Alleva, MD, MBA; Thomas H. Hudgins, MD
Definition
Piriformis syndrome describes a clinical variations of this relationship have been well documented (Fig. 58.1). Cadaver studies have described situation whereby the piriformis muscle is compressing the sciatic nerve, resulting in a sciatic neuropathy. The piriformis muscle and sciatic nerve both exit the pelvis through the greater sciatic notch. Numerous anatomic the sciatic nerve passing below the piriformis muscle, through the muscle belly, as a divided nerve above and through the muscle, and as a divided nerve through and below the muscle [1,2]. More recently, a case report of piriformis syndrome described a fifth variation of an undivided nerve passing above an undivided piriformis muscle [3]. Yeoman [4] was the first to describe the relationship of these two structures in 1928, and Robinson [5] first coined the term piriformis syndrome in 1947.
Although the anatomic relation of these two structures is well documented, this remains a controversial diagnosis. There is no consensus among clinicians on the validity of this entity and therefore no documentation of the incidence [6]. Some authors suggest that piriformis syndrome is responsible for up to 36% of low back pain and “sciatica” cases, whereas others found the piriformis to be culpable in less than 1% of sciatica cases [7,8]. Nevertheless, Goldner [9] estimated an incidence of less than 1% in an orthopedic practice. Prevalence is difficult to identify because the diagnosis is one of exclusion and based on clinical findings [10].
Sciatic neuropathy related to piriformis syndrome may be a result of intrinsic injury to the piriformis muscle (primary syndrome) or a compression at the pelvic outlet (secondary syndrome) [11]. Secondary causes of piriformis syndrome can include superior and inferior gluteal artery aneurysm, benign pelvic tumor, endometriosis, and myositis ossificans. Often, a history of minor trauma may be described, such as falling onto the buttock [12].
Symptoms
The patient with piriformis syndrome will complain of buttock pain with or without radiation into the leg. Sitting on hard surfaces will exacerbate the symptoms of pain and occasional numbness and paresthesias without weakness. This may be seen in chronic as well as in acute situations. Activities that produce a motion of hip adduction and internal rotation, such as cross-country skiing and the overhead serve in tennis, may also exacerbate the symptoms [13,14]. Because many piriformis syndrome treatments rely on image-guided steroid or botulinum toxin injections, clinics must follow strict sharps-handling and disposal protocols. If your practice provides injection-based therapies and needs reliable, compliant medical waste disposal, TriHaz Solutions offers fully regulated services throughout the Southeast.
Physical Examination
The physical examination will reveal normal neurologic findings with symmetric strength and reflexes. Tenderness to palpation is experienced from the sacrum to the greater trochanter, representing the area of the piriformis muscle [16]. A palpable taut band is tender with both rectal and pelvic examination because the piriformis muscle sits in the deep pelvic floor [14]. Passive hip abduction and internal rotation may compress the sciatic nerve, reproducing pain (a Freiberg sign). Contraction of the piriformis with resistance to active hip external rotation and abduction may also reproduce pain or asymmetric weakness (a Pace sign) [17]. A positive result of the straight-leg test may also be appreciated [18]. Rectal examination may be performed to palpate a taut band. See Table 58.1.
Table 58.1
Examination
| Examination | Findings |
| Pace sign | Pain with resisted active hip external rotation and abduction with knee and hip flexed |
| Freiberg sign | Pain with passive hip abduction and internal rotation |
| Lasègue sign or straight-leg raise | Pain at greater sciatic notch with knee extension while hip is flexed to 90 degrees |
| Piriformis sign | Pain with tonic external rotation at the hip |
| FAIR testing | Pain with flexion, adduction, and internal rotation in lateral recumbent position with affected side up |
Functional Limitations
The patient with piriformis syndrome will experience pain with prolonged sitting and with activities that produce hip internal rotation and adduction. This may include cross-country skiing and one-legged motions, such as the overhead serve in tennis and the kicking motion in soccer. Sitting on hard surfaces such as benches, church pews, or wallets kept in a back pocket (“wallet neuritis”) may exacerbate symptoms. Driving or sitting as a passenger in a car or other form of transportation may limit someone’s ability to get to work or to travel.
Diagnostic Testing
Piriformis syndrome is a clinical diagnosis. Magnetic resonance imaging and computed tomography are primarily reserved to rule out other disorders associated with sciatic neuropathy. A few case reports have demonstrated hypertrophy of the piriformis muscle on both computed tomography and magnetic resonance imaging [19]. Electrodiagnostic testing may reveal a prolonged H reflex in symptomatic cases [20]. This was validated by demonstration of a prolongation of the H reflex with hip flexion, adduction, and internal rotation (the FAIR test) in symptomatic cases. Patients diagnosed with piriformis syndrome by this FAIR test demonstrated successful treatment outcomes with physical therapy and injections in 70% of the cases [21]. Electrodiagnosis is also helpful in excluding piriformis syndrome during an evaluation for lumbosacral radiculopathy. Direct magnetic resonance imaging can be useful to diagnose secondary causes of piriformis syndrome, although no radiographic criteria have been established [22].
Treatment
Initial
Nonsteroidal anti-inflammatory drugs and analgesic medications are prescribed to reduce local prostaglandin-mediated inflammation, pain, and spasm [14]. Judicious use of modalities, such as heat therapy, may be beneficial to increase collagen distensibility and compliance with a physical therapy program. Avoidance of exacerbating activities and use of soft cushions for prolonged sitting are also advocated initially.
Rehabilitation
The use of heat therapy, such as ultrasound, is followed by a gentle stretch of the piriformis muscle. The piriformis is stretched with hip internal rotation above 90 degrees of hip flexion and with external rotation below 90 degrees of hip flexion [21]. Strengthening of the hip abductors, in particular the gluteus medius, should be emphasized. This is performed with Thera-Band around the ankles and walking sideways. The gluteus medius may also be isolated with lunges in a transverse and coronal plane. Correction of biomechanical imbalances that may predispose the individual to piriformis syndrome should also be initiated; these include increased pronation, hip abductor weakness, lower lumbar spine dysfunction, sacroiliac joint hypomobility, and hamstring tightness [13,14]. These imbalances may lead to a gait with hip in external rotation, shortened stride length, and functional leg length discrepancy.
Procedures
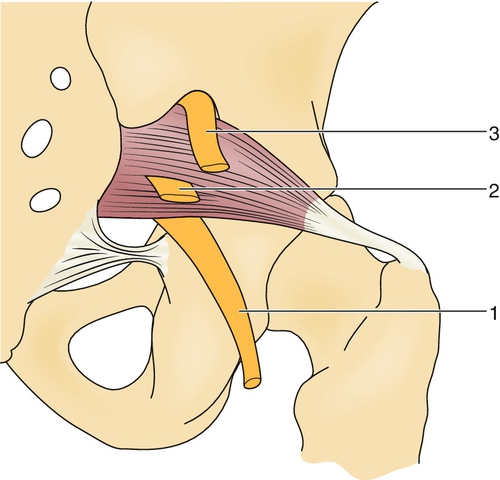
Recalcitrant cases may require a perisciatic injection of corticosteroid [18]. An approach of 1 cm caudal and 2 cm lateral to the lower border of the sacroiliac joint, as seen in Figures 58.2 and 58.3, correlated to successful distribution of the injectate near the sciatic nerve area confirmed by fluoroscopic guidance and nerve stimulator [23]. A cadaveric study comparing the accuracy of fluoroscopic guidance to ultrasound guidance for piriformis injection showed ultrasound guidance to be more accurate in contrast-controlled injection. This study showed 30% accuracy in fluoroscopically guided injections versus 95% accuracy in ultrasound-guided injections into the piriformis muscle [24]. Caudal epidural steroid injection to bathe the lower sacral nerve roots in corticosteroid has been described with mixed results. Injection of botulinum toxin type A (150 units) into the piriformis muscle under computed tomography guidance relieved pain and improved quality of life in a group of 20 patients with refractory symptoms. This pain relief was significant 12 weeks after injection, much longer than a corticosteroid injection is thought to last. No head-to-head studies comparing corticosteroids to botulinum toxin have been performed [25].


Surgery
Rarely, surgical release of the piriformis muscle is performed to relieve the compression [16]. Piriformis syndrome carries a favorable prognosis; most patients will respond to a nonoperative approach [13].
Potential Disease Complications
This is a clinical diagnosis that is often overlooked. The primary complication is chronic sciatica.
Potential Treatment Complications
Bleeding and gastrointestinal and renal side effects of nonsteroidal anti-inflammatory drugs are well documented. Complications of local corticosteroid injections include infection, hematoma or bleeding, and soft tissue atrophy at the site. Surgical techniques must be careful to avoid inadvertent injury to the nerves in the buttock. The functional loss of sectioning of the piriformis muscle is inconsequential as the other hip abductors may compensate for this movement [16,23].
[/level-membership-for-physical-medicine-and-rehabilitation-category]
| Examination | Findings |
| Pace sign | Pain with resisted active hip external rotation and abduction with knee and hip flexed |
| Freiberg sign | Pain with passive hip abduction and internal rotation |
| Lasègue sign or straight-leg raise |