CASE 58 Iliac Artery Disease
Case presentation
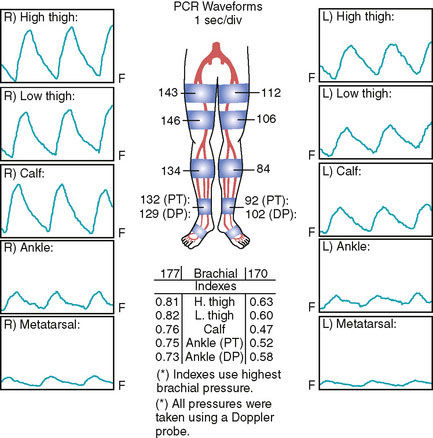
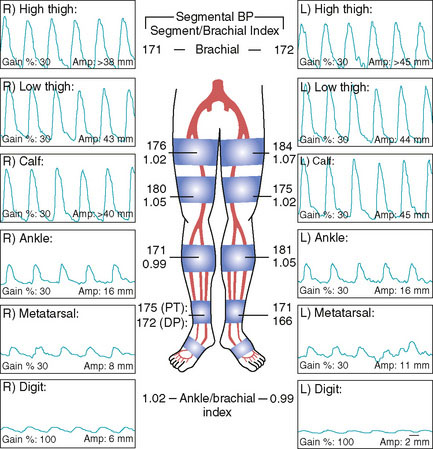
A 64-year-old woman with a history of hypertension, hyperlipidemia, and tobacco use noted progressive bilateral calf discomfort during activity. These symptoms slowly progressed, and ultimately they became so severe that she stopped participating in tennis, her favorite activity. She discussed these symptoms with her primary care physician. Her physician interpreted these symptoms as claudication and ordered noninvasive vascular testing. Her resting ankle brachial index (ABI) was 0.75 on the right and 0.58 on the left (Figure 58-1). After exercise, her right ABI dropped to 0.60 and her left ABI dropped to 0.21. In addition, exercise caused significant bilateral calf pain, with the left side hurting more than the right. She was subsequently referred for angiography.
Angiography
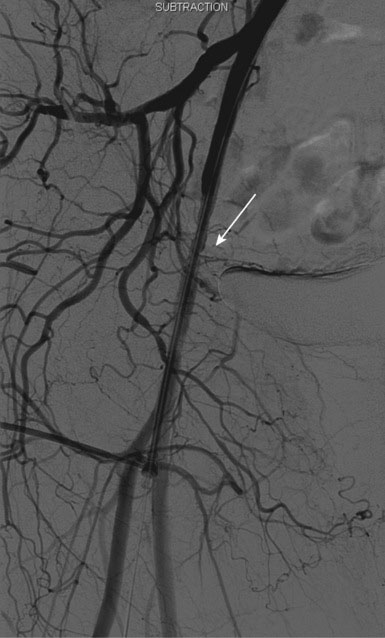
Abdominal angiography found normal renal arteries and distal aorta. Angiography of the pelvic vessels demonstrated a severe stenosis of the left external iliac artery (Figures 58-2, 58-3). Initially, there did not appear to be appreciable disease in the right iliac system to account for the findings on the noninvasive study; however, there was significant vessel overlap. The femoral and runoff vessels appeared normal bilaterally.
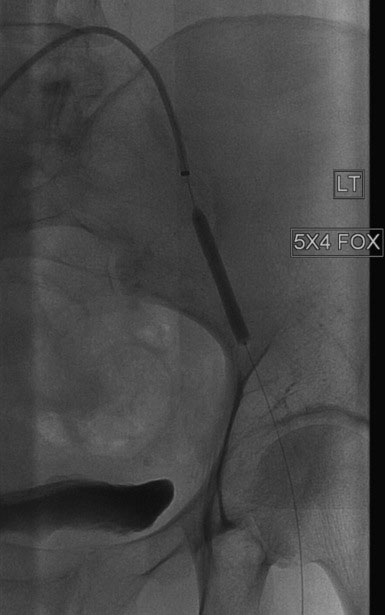
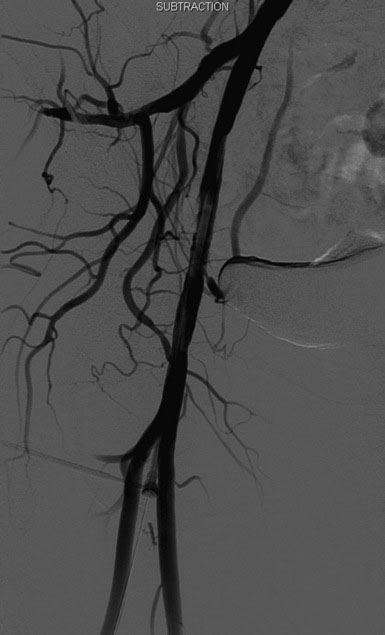
The left external iliac lesion was felt to be consistent with her noninvasive studies and likely accounted for her symptoms. The etiology of her right leg findings was not apparent on the initial angiograms. The operator decided to proceed with intervention of the left external iliac. Arterial access had initially been obtained in the right common femoral artery for the diagnostic angiograms. A long, 6 French Ansel 2 sheath was taken up and over the aortoiliac bifurcation and positioned proximal to the left external iliac lesion. A bolus of unfractionated heparin was administered intravenously to achieve a therapeutic activated clotting time of greater than 250 seconds. The operator positioned an 0.018 inch guidewire distally (Figure 58-4) and dilated the stenosis with a 5 mm diameter by 40 mm long balloon (Figure 58-5). Following balloon angioplasty, substantial residual narrowing remained due to elastic recoil. The operator then deployed a 7 mm diameter by 40 mm long self-expanding nitinol stent and postdilated the stent with the 5 mm diameter by 40 mm long balloon. The post-stent angiogram revealed an excellent result (Figure 58-6) and angiography of the distal runoff showed no distal emboli.

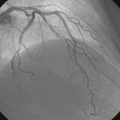
FIGURE 58-6 Angiographic appearance of the left external iliac artery following angioplasty and stenting.
Following the procedure on the left external iliac artery, the operator withdrew the long sheath over a 0.035 inch wire. Pressure monitoring during the pullback uncovered a 60 mmHg pressure gradient between the distal aorta and the distal right external iliac. Another angiogram was performed, which found a stenosis just proximal to the inguinal ligament (Figure 58-7). The lesion did not resolve with intraarterial nitroglycerin. Although it did not appear severe angiographically, this stenosis was associated with a significant pressure gradient and likely accounted for the patient’s right leg symptoms and the findings on the noninvasive studies. The distal right external iliac stenosis was then treated with a 5 mm diameter by 40 mm long balloon for a prolonged inflation (Figures 58-8, 58-9). The operator was not entirely satisfied with the angiographic result and placed a 7 mm diameter by 40 mm long self-expanding nitinol stent, post dilated with the 5 mm diameter by 40 mm long balloon. The final angiograms demonstrated an excellent result with no evidence of distal embolization (Figure 58-10).
Postprocedural course
The arterial sheath was removed by manual pressure when the activated clotting time fell below 180 seconds and the patient was prescribed bed rest for 4 hours. She was discharged later that same day. At follow-up 1 month later, noninvasive testing was repeated and found a right ABI of 1.02 and a left ABI of 0.99 at rest (Figure 58-11). With exercise, the right ABI was 1.00 and the left ABI was 1.01. Her symptoms had completely resolved and she was able to return to her tennis game.
Discussion
Over 8 million individuals in the United States have peripheral arterial disease. Many are asymptomatic; however, at least a third experience claudication, and up to 5% develop limb-threatening ischemia.1 Noninvasive physiologic testing helps determine the degree of arterial insufficiency and provides information regarding the location of the stenoses. Conventional angiography remains the gold standard to define the arterial anatomy and diagnose luminal obstruction. Adjunctive techniques performed during angiography are also helpful to assess the disease severity and include measurement of translesional pressure gradients and intravascular ultrasound. In fact, in this case, based solely on the angiogram, the disease in the right external iliac artery might have been disregarded; the measurement of a translesional pressure gradient determined that this disease was, in fact, significant.
The management of inflow disease is outlined in the TransAtlantic Inter-Society Consensus Document on Management of Peripheral Arterial Disease (TASC), which was last revised in 2007.2 In this document, a classification system has been devised to help guide in the management of inflow disease (Table 58-1). Based on the excellent long-term patency rates with endovascular therapy, aortoiliac disease classified as TASC A or B is considered best treated initially by endovascular techniques. Lesions classified as TASC D are managed surgically. Lesions characterized as TASC C have a lower likelihood of long-term success with an endovascular approach. In this category, patient variables such as comorbidities and overall functional status become extremely important in the decision process. Surgical management is usually recommended in patients with TASC C lesions and low surgical risk due to better long-term outcomes with regards to patency. However, in these categories, it may be reasonable to proceed with an initial endovascular approach as long as surgical targets are not compromised. As the field of endovascular therapy evolves, new devices and novel techniques may improve the long-term patency and new data originating from larger series and randomized controlled trials may change these recommendations to a primary endovascular strategy.
| Classification | Characteristics |
|---|---|
| Type A |
1 Creager M.A., Loscalzo J. Vascular Diseases of the Extremities. In: Fauci A.S., Braunwald E., Kasper D.L., Hauser S.L., Longo D.L., Jameson J.L., Loscalzo J., editors. Harrison’s Principles of Internal Medicine. ed 17. New York, NY: McGraw-Hill; 2008:1568-1570.
2 on behalf of theNorgren L., Hiatt W.R., Dormandy J.A., Nehler M.R., Harris K.A., Fowkes F.G.R., TASC II Working Group. Inter-society consensus for the management of peripheral arterial disease (TASC II). Eur J Vasc Endovasc Surg. 2007;33:S1-S70.