Procedure 57 Open Reduction of Metacarpophalangeal Joint Dislocation
Examination/Imaging
Clinical Examination
 The MCP joint region will be swollen and tender.
The MCP joint region will be swollen and tender.
 A neurovascular examination of the finger should be performed to document perfusion and sensory changes.
A neurovascular examination of the finger should be performed to document perfusion and sensory changes.
 Simple subluxation should be distinguished from a complete dislocation.
Simple subluxation should be distinguished from a complete dislocation.
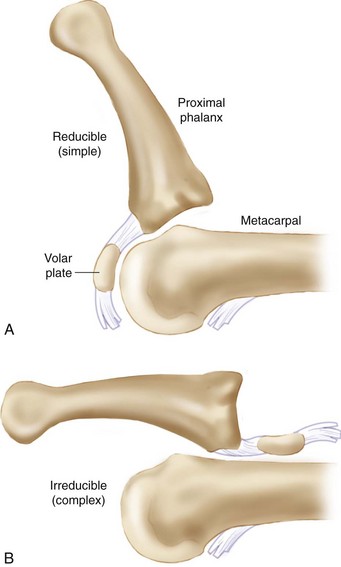
 In simple subluxation, the proximal phalanx is locked in a hyperextended position (Fig. 57-1).
In simple subluxation, the proximal phalanx is locked in a hyperextended position (Fig. 57-1).
 In a complete dislocation, the proximal phalanx may be less hyperextended and may even be in a bayoneted position (Fig. 57-2).
In a complete dislocation, the proximal phalanx may be less hyperextended and may even be in a bayoneted position (Fig. 57-2).
Surgical Anatomy
 The MCP volar plate has a weaker proximal insertion and tends to avulse from the metacarpal, remaining attached to the base of the proximal phalanx.
The MCP volar plate has a weaker proximal insertion and tends to avulse from the metacarpal, remaining attached to the base of the proximal phalanx.
 In a simple subluxation, the proximal phalanx is hyperextended. In this case, the volar plate remains draped over the articular surface of the metacarpal head and does not lie on the dorsal cortex of the metacarpal head (Fig. 57-4A).
In a simple subluxation, the proximal phalanx is hyperextended. In this case, the volar plate remains draped over the articular surface of the metacarpal head and does not lie on the dorsal cortex of the metacarpal head (Fig. 57-4A).
 In a complete or complex dislocation, the proximal phalanx is less hyperextended and may be in a bayonet position. In this case, the volar plate is no longer draped over the metacarpal articular surface but rather lies completely dorsal to the metacarpal head (Fig. 57-4B).
In a complete or complex dislocation, the proximal phalanx is less hyperextended and may be in a bayonet position. In this case, the volar plate is no longer draped over the metacarpal articular surface but rather lies completely dorsal to the metacarpal head (Fig. 57-4B).
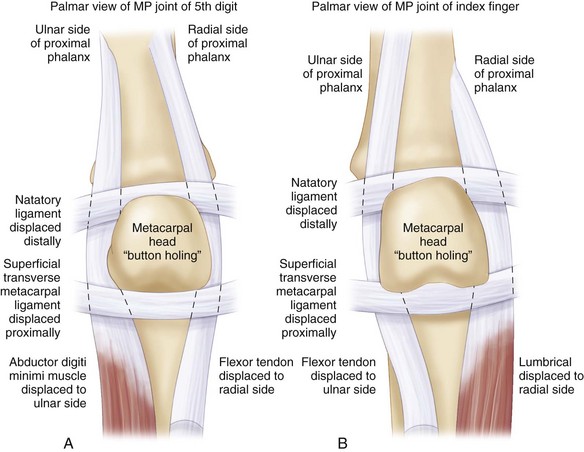
 The dislocation is made complex (irreducible) not only by the volar plate but also by the flexor tendons and lumbrical, which form a noose around the metacarpal neck (Fig. 57-5).
The dislocation is made complex (irreducible) not only by the volar plate but also by the flexor tendons and lumbrical, which form a noose around the metacarpal neck (Fig. 57-5).
Exposures
 A longitudinal incision is made dorsal to the MCP joint.
A longitudinal incision is made dorsal to the MCP joint.
 In the thumb, the interval between the extensor pollicis brevis (EPB) and extensor pollicis longus (EPL) is incised.
In the thumb, the interval between the extensor pollicis brevis (EPB) and extensor pollicis longus (EPL) is incised.
 In the index and small fingers, the interval between the extensor digitorum communis (EDC) and the more ulnar proprius or minimi tendon is incised.
In the index and small fingers, the interval between the extensor digitorum communis (EDC) and the more ulnar proprius or minimi tendon is incised.
 In the long and ring fingers, the extensor tendon is split longitudinally in its midline.
In the long and ring fingers, the extensor tendon is split longitudinally in its midline.
 The dorsal capsule is torn, but further capsulotomy and retraction or dorsal capsulectomy may be necessary to visualize the pathology.
The dorsal capsule is torn, but further capsulotomy and retraction or dorsal capsulectomy may be necessary to visualize the pathology.
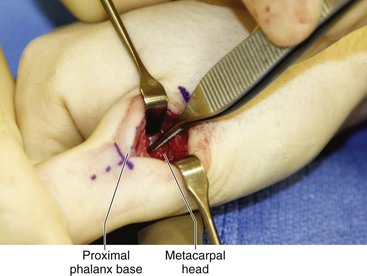
 The base of the proximal phalanx with attached volar plate is noted to lie on top of the metacarpal head (Fig. 57-6).
The base of the proximal phalanx with attached volar plate is noted to lie on top of the metacarpal head (Fig. 57-6).
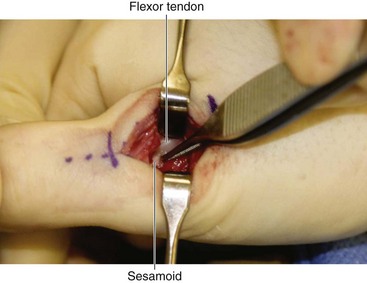
 The flexor tendon can be seen dorsal to the metacarpal head, resulting in a complex (irreducible) dislocation (Fig. 57-7).
The flexor tendon can be seen dorsal to the metacarpal head, resulting in a complex (irreducible) dislocation (Fig. 57-7).
 The sesamoids within the volar plate can be seen dorsal to the metacarpal head (see Fig. 57-7).
The sesamoids within the volar plate can be seen dorsal to the metacarpal head (see Fig. 57-7).
Procedure
Step 1
 Closed reduction should be attempted one more time after induction of anesthesia, before opening.
Closed reduction should be attempted one more time after induction of anesthesia, before opening.
 The wrist is flexed to take tension off the flexor tendons, which may be preventing reduction.
The wrist is flexed to take tension off the flexor tendons, which may be preventing reduction.
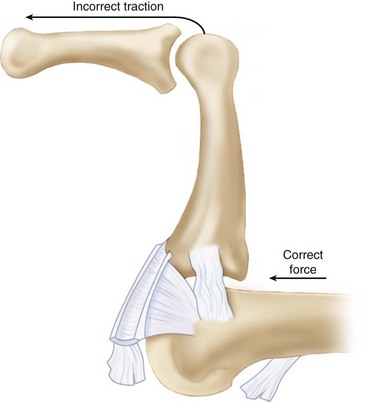
 Pressure is applied to the base of the proximal phalanx, pushing it distally and volarly, sliding it over the metacarpal head (Fig. 57-8).
Pressure is applied to the base of the proximal phalanx, pushing it distally and volarly, sliding it over the metacarpal head (Fig. 57-8).
 If this is unsuccessful, hyperextension may be required before applying pressure to the base of the proximal phalanx.
If this is unsuccessful, hyperextension may be required before applying pressure to the base of the proximal phalanx.
 If attempt at reduction under anesthesia is not successful, proceed with open reduction.
If attempt at reduction under anesthesia is not successful, proceed with open reduction.
Step 1 Pitfalls
Traction should be avoided during reduction maneuvers for both simple subluxation and complex dislocation (see Fig. 57-8).
Traction simply tightens the noose in a complex dislocation.
Traction can convert a simple subluxation to a complex dislocation.
Hyperextension should be avoided during reduction maneuvers for simple subluxation because it can convert this to a complex dislocation.
Step 3
 The wrist is flexed to relax the noose formed by the flexor tendons and lumbrical.
The wrist is flexed to relax the noose formed by the flexor tendons and lumbrical.
 A Freer elevator is used to push the volar plate distally and volarly, pushing it back into the joint space.
A Freer elevator is used to push the volar plate distally and volarly, pushing it back into the joint space.
 Simultaneously, the proximal phalanx is gently pushed distally and volarly, sliding it over the metacarpal head.
Simultaneously, the proximal phalanx is gently pushed distally and volarly, sliding it over the metacarpal head.
 If necessary, the flexor tendon is manipulated gently with a pick-up, pushing it back around the lateral aspect of the metacarpal head and into its normal volar position.
If necessary, the flexor tendon is manipulated gently with a pick-up, pushing it back around the lateral aspect of the metacarpal head and into its normal volar position.
Additional Steps
 Occasionally, reduction cannot be achieved by the previous technique.
Occasionally, reduction cannot be achieved by the previous technique.
 In this situation, the volar plate is divided longitudinally in its midline.
In this situation, the volar plate is divided longitudinally in its midline.
 The split volar plate then spreads out of the way of the metacarpal head as the joint is reduced.
The split volar plate then spreads out of the way of the metacarpal head as the joint is reduced.
 Alternatively, it can be tucked back into the joint, one side at a time, while radially and ulnarly deviating the proximal phalanx.
Alternatively, it can be tucked back into the joint, one side at a time, while radially and ulnarly deviating the proximal phalanx.
 If a dorsal metacarpal head shear fracture is present, it can be fixed with a K-wire or a small screw (Fig. 57-9).
If a dorsal metacarpal head shear fracture is present, it can be fixed with a K-wire or a small screw (Fig. 57-9).
 The MCP joint is usually stable after reduction, and K-wire fixation is not routinely necessary.
The MCP joint is usually stable after reduction, and K-wire fixation is not routinely necessary.
Postoperative Care and Expected Outcomes
 Within 3 to 5 days, the patient should begin range of motion.
Within 3 to 5 days, the patient should begin range of motion.
 An Orthoplast dorsal block splint is fabricated to prevent MCP hyperextension, and active flexion and extension within the splint are encouraged.
An Orthoplast dorsal block splint is fabricated to prevent MCP hyperextension, and active flexion and extension within the splint are encouraged.
 The interphalangeal joints can be left free.
The interphalangeal joints can be left free.
 The splint is weaned and light activity allowed at 4 to 6 weeks.
The splint is weaned and light activity allowed at 4 to 6 weeks.
 No sports or heavy use is allowed for 3 months.
No sports or heavy use is allowed for 3 months.
 Patients tend to have very good motion and hand function, although mild residual stiffness is not uncommon.
Patients tend to have very good motion and hand function, although mild residual stiffness is not uncommon.