Procedure 56 Percutaneous Pinning of Bennett Fracture and Open Reduction and Internal Fixation of Rolando Fracture
Indications
Figures 56-9 through 56-11 provided courtesy of Kevin C. Chung, MD; Figures 56-14 through 56-17 provided courtesy of Sandeep J. Sebastin, MD.
 If the fracture is nondisplaced at initial presentation (uncommon), it can be treated with splint or cast immobilization for 6 weeks, followed by protected motion.
If the fracture is nondisplaced at initial presentation (uncommon), it can be treated with splint or cast immobilization for 6 weeks, followed by protected motion.
 Surgery is indicated for failure to maintain acceptable reduction with splint or cast (articular step-off of <1 mm).
Surgery is indicated for failure to maintain acceptable reduction with splint or cast (articular step-off of <1 mm).
 Most Bennett and Rolando fractures are unstable and require surgical intervention.
Most Bennett and Rolando fractures are unstable and require surgical intervention.
 In most cases, closed reduction and percutaneous pinning is indicated for Bennett fractures.
In most cases, closed reduction and percutaneous pinning is indicated for Bennett fractures.
 Open reduction is indicated when reduction cannot be achieved by closed means (more common with Rolando fracture).
Open reduction is indicated when reduction cannot be achieved by closed means (more common with Rolando fracture).
 If open reduction is required, large fragments can be fixated by a variety of methods (plate, lag screw, percutaneous K-wires), whereas small fragments are best treated with K-wire fixation.
If open reduction is required, large fragments can be fixated by a variety of methods (plate, lag screw, percutaneous K-wires), whereas small fragments are best treated with K-wire fixation.
Surgical Anatomy
 A Bennett fracture is a two-fragment intra-articular thumb metacarpal base fracture.
A Bennett fracture is a two-fragment intra-articular thumb metacarpal base fracture.
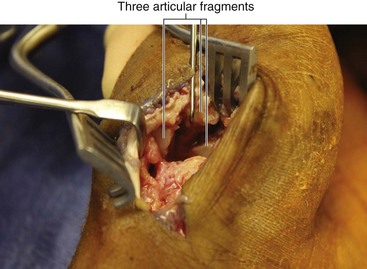
 A Rolando fracture is a three-fragment intra-articular thumb metacarpal base fracture.
A Rolando fracture is a three-fragment intra-articular thumb metacarpal base fracture.
 The thumb carpometacarpal (CMC) joint geometry is similar to two interlocking saddles, with their surfaces at 90 degrees to each other.
The thumb carpometacarpal (CMC) joint geometry is similar to two interlocking saddles, with their surfaces at 90 degrees to each other.
 The volar beak ligament is deep to the superficial anterior oblique ligament (SAOL) and is an important stabilizer of the thumb CMC joint.
The volar beak ligament is deep to the superficial anterior oblique ligament (SAOL) and is an important stabilizer of the thumb CMC joint.
 In a Bennett fracture, the volar beak ligament stabilizes the Bennett fragment, which is located volarly and ulnarly.
In a Bennett fracture, the volar beak ligament stabilizes the Bennett fragment, which is located volarly and ulnarly.
 The larger fragment, consisting of the remainder of the metacarpal, must be reduced to the Bennett fragment.
The larger fragment, consisting of the remainder of the metacarpal, must be reduced to the Bennett fragment.
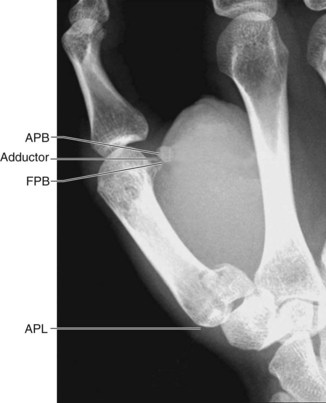
 The abductor pollicis longus (APL) tendon inserts on the dorsal base of the thumb metacarpal and causes dorsal subluxation and proximal displacement of the metacarpal (Fig. 56-1).
The abductor pollicis longus (APL) tendon inserts on the dorsal base of the thumb metacarpal and causes dorsal subluxation and proximal displacement of the metacarpal (Fig. 56-1).
 The adductor pollicis inserts on the metacarpal shaft and causes CMC flexion and adduction (see Fig. 56-1).
The adductor pollicis inserts on the metacarpal shaft and causes CMC flexion and adduction (see Fig. 56-1).
 In a Bennett fracture, the metacarpal is supinated, adducted, and flexed, with proximal displacement and dorsal subluxation of the base.
In a Bennett fracture, the metacarpal is supinated, adducted, and flexed, with proximal displacement and dorsal subluxation of the base.
Positioning
 A pneumatic tourniquet is placed on the arm in case closed reduction is not possible and open reduction is required.
A pneumatic tourniquet is placed on the arm in case closed reduction is not possible and open reduction is required.
 The extremity is placed on a hand table, with the thumb pointing upward.
The extremity is placed on a hand table, with the thumb pointing upward.
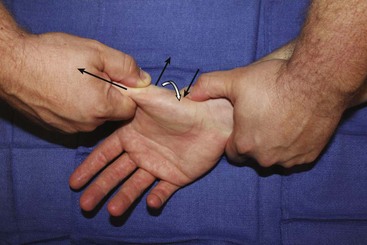
 The surgeon or assistant placing the K-wires sits at the patient’s axilla, facing the palm.
The surgeon or assistant placing the K-wires sits at the patient’s axilla, facing the palm.
 The surgeon or assistant performing the reduction sits at the patient’s shoulder, facing the dorsum of the hand.
The surgeon or assistant performing the reduction sits at the patient’s shoulder, facing the dorsum of the hand.
Exposures
 If open reduction is required, the exposure is through a modified Wagner incision (Fig. 56-2).
If open reduction is required, the exposure is through a modified Wagner incision (Fig. 56-2).
 The longitudinal limb of the incision is along the glabrous/nonglabrous skin border.
The longitudinal limb of the incision is along the glabrous/nonglabrous skin border.
 At the thumb base, the incision turns ulnarly and extends to the flexor carpi radialis (FCR) tendon.
At the thumb base, the incision turns ulnarly and extends to the flexor carpi radialis (FCR) tendon.
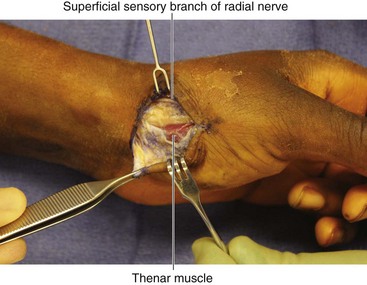
 Dissection is carried down to the border of the thenar musculature, protecting sensory nerve branches in the subcutaneous tissue (Fig. 56-3).
Dissection is carried down to the border of the thenar musculature, protecting sensory nerve branches in the subcutaneous tissue (Fig. 56-3).
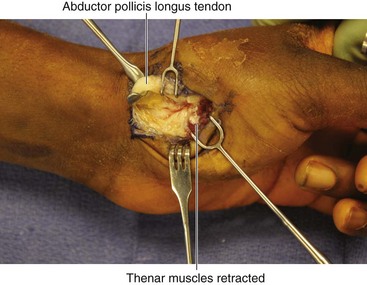
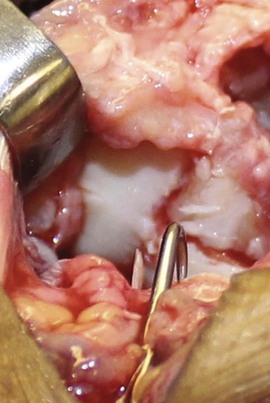
 A no. 15 blade is used to elevate the thenar muscles off of the metacarpal base and trapezium (Fig. 56-4).
A no. 15 blade is used to elevate the thenar muscles off of the metacarpal base and trapezium (Fig. 56-4).
 The APL tendon is reflected ulnarly.
The APL tendon is reflected ulnarly.
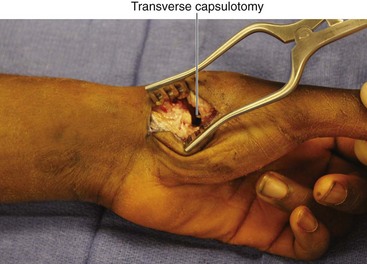
 The joint is then exposed with a transverse capsulotomy, in the interval between the APL and the reflected thenar musculature (Fig. 56-5).
The joint is then exposed with a transverse capsulotomy, in the interval between the APL and the reflected thenar musculature (Fig. 56-5).
Pearls
It is important not to extend the Wagner incision ulnar to the FCR tendon, to avoid injury to the palmar cutaneous branch of the median nerve.
It is important to protect sensory nerves, such as the superficial sensory branches of the radial nerve, and smaller branches of the lateral antebrachial cutaneous nerve (LABC).
Fluoroscopy can be used to confirm joint location before capsulotomy.
Pitfalls
Injury to the palmar cutaneous branch of the median nerve by extending the incision ulnar to the FCR.
Injury to the LABC or superficial sensory branch of the radial nerve.
Excessive soft tissue elevation at the metacarpal base resulting in disinsertion of the APL—care should be taken to preserve the APL insertion.
Procedures
Closed Reduction Percutaneous Pinning of Bennett Fracture
Step 1
Step 2
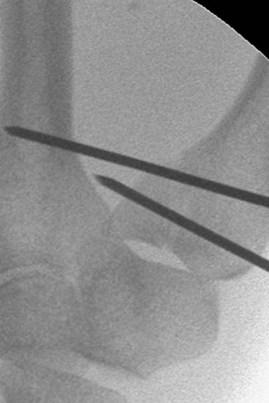
 While reduction is maintained, K-wires are placed.
While reduction is maintained, K-wires are placed.
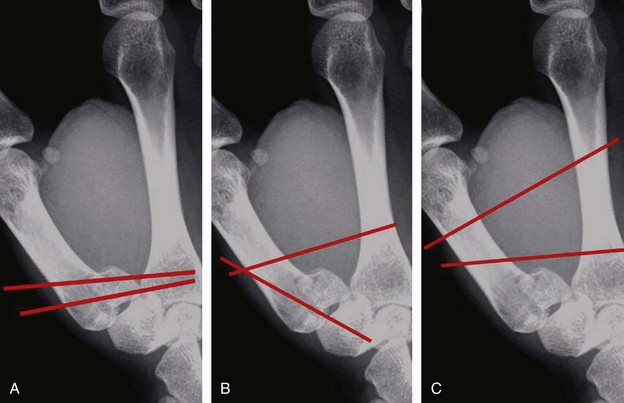
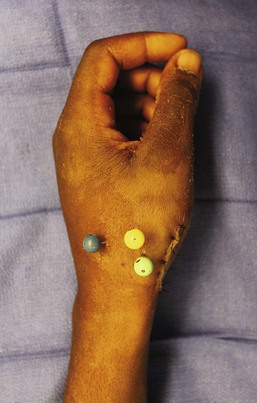
 Multiple patterns of K-wire fixation are acceptable (Fig. 56-7); the author’s preference follows.
Multiple patterns of K-wire fixation are acceptable (Fig. 56-7); the author’s preference follows.
Step 2 Pearls
• If placing the initial K-wire while maintaining fracture reduction proves difficult, the K-wire can be placed into the metacarpal base, but not across the fracture, with the fracture unreduced.
• Once the K-wire is in position, the fracture is reduced, and the K-wire is advanced across the fracture and into the Bennett fragment.
• K-wires should be advanced using oscillating mode on the K-wire driver, to avoid injury to sensory nerve branches.
Alternative 1
 A 0.045-inch K-wire is inserted into the thumb metacarpal shaft, beginning at the middle or distal third.
A 0.045-inch K-wire is inserted into the thumb metacarpal shaft, beginning at the middle or distal third.
 It is advanced proximally down the medullary canal and across the CMC joint into the trapezium.
It is advanced proximally down the medullary canal and across the CMC joint into the trapezium.
 The leading tip of the K-wire should enter the subchondral bone of the proximal trapezium, without entering the scaphotrapezial joint (Fig. 56-9).
The leading tip of the K-wire should enter the subchondral bone of the proximal trapezium, without entering the scaphotrapezial joint (Fig. 56-9).
 The second K-wire is then advanced from the radial metacarpal base, across the fracture, and into the Bennett fragment (Fig. 56-10).
The second K-wire is then advanced from the radial metacarpal base, across the fracture, and into the Bennett fragment (Fig. 56-10).
 Alternatively, it can be placed from the thumb metacarpal into the index metacarpal (Fig. 56-11).
Alternatively, it can be placed from the thumb metacarpal into the index metacarpal (Fig. 56-11).
Postoperative Care and Expected Outcomes
 Pins are removed 6 weeks after surgery.
Pins are removed 6 weeks after surgery.
 Mobilization is begun 6 weeks after surgery under the guidance of a hand therapist.
Mobilization is begun 6 weeks after surgery under the guidance of a hand therapist.
 Posttraumatic arthritis may develop, particularly if articular reduction is not achieved. This may or may not be clinically significant.
Posttraumatic arthritis may develop, particularly if articular reduction is not achieved. This may or may not be clinically significant.
 Radiographic and clinical outcomes are likely superior in patients who heal with less than 1 mm of articular step-off.
Radiographic and clinical outcomes are likely superior in patients who heal with less than 1 mm of articular step-off.
Open Reduction and Percutaneous Pinning of Bennett Fracture
Step 2
Postoperative Care and Expected Outcomes
 Pins are removed 6 weeks after surgery.
Pins are removed 6 weeks after surgery.
 Mobilization is begun 6 weeks after surgery under the guidance of a hand therapist.
Mobilization is begun 6 weeks after surgery under the guidance of a hand therapist.
 Posttraumatic arthritis may develop, particularly if articular reduction is not achieved. This may or may not be clinically significant.
Posttraumatic arthritis may develop, particularly if articular reduction is not achieved. This may or may not be clinically significant.
 Radiographic and clinical outcomes are superior in patients who heal with less than a 1-mm step-off.
Radiographic and clinical outcomes are superior in patients who heal with less than a 1-mm step-off.
Open Reduction and Internal Fixation of Rolando Fracture
Step 2
Step 3
Postoperative Care and Expected Outcomes
 Sutures are removed in 10 to 14 days, and an Orthoplast splint is made.
Sutures are removed in 10 to 14 days, and an Orthoplast splint is made.
 Active range of motion begins at 10 to 14 days, and passive range of motion when tolerated.
Active range of motion begins at 10 to 14 days, and passive range of motion when tolerated.
 Strengthening begins at 6 weeks.
Strengthening begins at 6 weeks.
 Good outcomes are expected if the fracture heals with acceptable articular reduction (step-off of <1 mm).
Good outcomes are expected if the fracture heals with acceptable articular reduction (step-off of <1 mm).
Open Reduction and Percutaneous Pinning of Comminuted Thumb Metacarpal Base Fracture
Step 1
Step 3
Step 4
Step 5
Green DP, O’Brien ET. Fractures of the thumb metacarpal. South Med J. 1972;65:807-814.
Kjaer-Petersen K, Langhoff O, Andersen K. Bennett’s fracture. J Hand Surg [Br]. 1990;15:58-61.
Timmenga EF, Blokhuis TJ, Maas M, et al. Long-term evaluation of Bennett’s fracture: a comparison between open and closed reduction. J Hand Surg [Br]. 1994;19:373-377.