Procedure 55 Metacarpal Shaft Fractures
![]() See Video 39: Metacarpal Shaft Fractures
See Video 39: Metacarpal Shaft Fractures
Examination/Imaging
Clinical Examination
 Note swelling and bruising over the dorsum of the hand.
Note swelling and bruising over the dorsum of the hand.
 Multiple metacarpal fractures predispose to compartment syndrome of the hand.
Multiple metacarpal fractures predispose to compartment syndrome of the hand.
 Look carefully for any wounds—may indicate an open fracture.
Look carefully for any wounds—may indicate an open fracture.
 Look carefully for rotational deformity with fingers flexed as much as possible and compare with opposite hand.
Look carefully for rotational deformity with fingers flexed as much as possible and compare with opposite hand.
 Ensure circulation is adequate by checking capillary refill.
Ensure circulation is adequate by checking capillary refill.
 Test and document digital sensation.
Test and document digital sensation.
 Ask patient to flex and extend the interphalangeal joints within limits of pain to confirm continuity of flexor and extensor tendons.
Ask patient to flex and extend the interphalangeal joints within limits of pain to confirm continuity of flexor and extensor tendons.
Surgical Anatomy
 Metacarpals can be easily accessed through the dorsal approach (Fig. 55-1).
Metacarpals can be easily accessed through the dorsal approach (Fig. 55-1).
 Dorsal cutaneous nerves and veins are located in the subcutaneous plane and must be identified and preserved.
Dorsal cutaneous nerves and veins are located in the subcutaneous plane and must be identified and preserved.
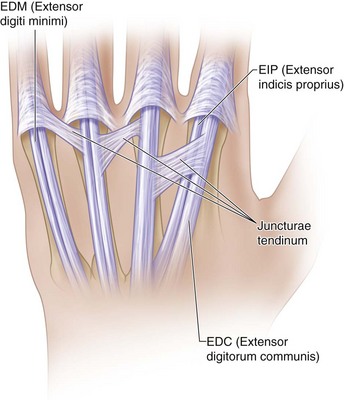
 The extensor tendons are surrounded by paratenon and can be easily separated by dividing the juncturae tendinum that interconnect them at the level of the metacarpal necks (Fig. 55-2).
The extensor tendons are surrounded by paratenon and can be easily separated by dividing the juncturae tendinum that interconnect them at the level of the metacarpal necks (Fig. 55-2).
Positioning
Exposures
 A longitudinal incision is marked along the dorsum of the metacarpal. The incision is centered over the fracture and equals the length of the plate.
A longitudinal incision is marked along the dorsum of the metacarpal. The incision is centered over the fracture and equals the length of the plate.
 In open injuries, the open wound is incorporated in the incision and excised as needed.
In open injuries, the open wound is incorporated in the incision and excised as needed.
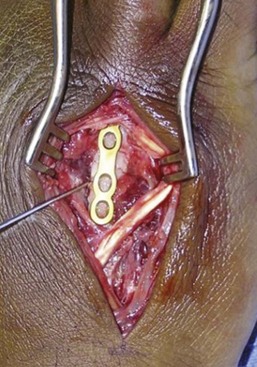
 For fixation of multiple fractures, two incisions on the dorsum in the second and fourth web space will provide access to adjacent metacarpals and allow decompression of the interosseous compartments if needed. Alternatively, a transverse incision across the back of the hand may be used as an extension of a preexisting traumatic wound (Fig. 55-3).
For fixation of multiple fractures, two incisions on the dorsum in the second and fourth web space will provide access to adjacent metacarpals and allow decompression of the interosseous compartments if needed. Alternatively, a transverse incision across the back of the hand may be used as an extension of a preexisting traumatic wound (Fig. 55-3).
 After spreading dissection, the extensors are exposed and retracted (Fig. 55-4).
After spreading dissection, the extensors are exposed and retracted (Fig. 55-4).
 The periosteum at the fracture site is elevated circumferentially to allow accurate reduction and remove any interposed soft tissue.
The periosteum at the fracture site is elevated circumferentially to allow accurate reduction and remove any interposed soft tissue.
Pearls
For plating of adjacent metacarpals, a single skin incision between the metacarpals will allow access to both fractures (Fig. 55-5).
Careful spreading dissection is necessary after skin incision to preserve subcutaneous nerves and veins.
Paratenon around the extensor tendons must be preserved to minimize postoperative tendon adhesions.
Juncturae tendinum between tendons may need to be divided to facilitate retraction of the extensor tendons.
In case of excessive comminution, periosteum around the fracture is left intact, and the implant is secured distally and proximally. Figure 55-6 shows the bridge plating technique used in a comminuted metacarpal fracture due to a gunshot wound.
Procedure
Step 1: Principles and Methods of Fixation
 In oblique and spiral fractures, achieve provisional reduction and stabilize with a K-wire (Fig. 55-7).
In oblique and spiral fractures, achieve provisional reduction and stabilize with a K-wire (Fig. 55-7).
 Temporary fixation of transverse fractures is not usually possible. After a trial reduction is performed, proceed with fixation of the plate to one fragment.
Temporary fixation of transverse fractures is not usually possible. After a trial reduction is performed, proceed with fixation of the plate to one fragment.
 Type of fixation depends on the fracture geometry.
Type of fixation depends on the fracture geometry.
 Transverse fractures are treated with compression plating (Fig. 55-8).
Transverse fractures are treated with compression plating (Fig. 55-8).
 Short oblique fractures are held with reduction forceps and stabilized with a lag screw. The fixation is then reinforced with a contoured plate without additional compression through the plate (neutralization plate). If the plane of the fracture allows insertion of the lag screw through the plate, this is preferred.
Short oblique fractures are held with reduction forceps and stabilized with a lag screw. The fixation is then reinforced with a contoured plate without additional compression through the plate (neutralization plate). If the plane of the fracture allows insertion of the lag screw through the plate, this is preferred.
 For insertion of a lag screw, first drill the thread hole through both cortices. Then drill near the cortex with a lag hole and countersink near the cortex. Countersinking minimizes the risk for fracture of the near cortex when the screw is tightened by distributing force more evenly the around screw hole. Screw length is measured and the appropriate screw inserted.
For insertion of a lag screw, first drill the thread hole through both cortices. Then drill near the cortex with a lag hole and countersink near the cortex. Countersinking minimizes the risk for fracture of the near cortex when the screw is tightened by distributing force more evenly the around screw hole. Screw length is measured and the appropriate screw inserted.
 Long oblique and spiral fractures that are longer than two times the diameter of the bone are stabilized with a series of lag screws. Plating is not necessary (Fig. 55-9).
Long oblique and spiral fractures that are longer than two times the diameter of the bone are stabilized with a series of lag screws. Plating is not necessary (Fig. 55-9).
 When multiple lag screws are to be placed, generally the smaller fragment is lagged to the larger piece.
When multiple lag screws are to be placed, generally the smaller fragment is lagged to the larger piece.
Step 1 Pitfalls
In a short oblique fracture, the lag screw placement interferes with plate placement. If the fracture is in the coronal plane, the plate is fixed to bone first, and then the lag screw is passed through the plate.
Avoid aggressive countersinking of the near cortex using powered instruments to prevent weakening the cortex.
Placing a screw too close to the fracture line may result in additional comminution. Stay at least two screw head diameters away from the fracture line.
Step 2: Dynamic Compression Plate
 A transverse diaphyseal fracture without comminution is best treated with compression plating.
A transverse diaphyseal fracture without comminution is best treated with compression plating.
 A dynamic compression plate of adequate length is selected to ensure a minimum fixation of four cortices (two screws) on either side of the fracture.
A dynamic compression plate of adequate length is selected to ensure a minimum fixation of four cortices (two screws) on either side of the fracture.
 The plate is prebent slightly so that it stands off the fracture by 2 mm to ensure that the far cortex does not gap when compression is applied.
The plate is prebent slightly so that it stands off the fracture by 2 mm to ensure that the far cortex does not gap when compression is applied.
 The oval holes in the plate enable application of compression as the screws are tightened.
The oval holes in the plate enable application of compression as the screws are tightened.
 A trial reduction is first performed, and then the plate is fixed to one fragment with a single screw close to the fracture site. The screw is drilled and inserted in the center of the drill hole.
A trial reduction is first performed, and then the plate is fixed to one fragment with a single screw close to the fracture site. The screw is drilled and inserted in the center of the drill hole.
 The plate is then aligned with the long axis of the bone, and the opposite fragment is fixed. Using an eccentric drill guide, the drill hole for the screw is made at the edge of the oval hole away from the fracture.
The plate is then aligned with the long axis of the bone, and the opposite fragment is fixed. Using an eccentric drill guide, the drill hole for the screw is made at the edge of the oval hole away from the fracture.
 As the screw is inserted and centers within the plate hole, it moves the fragment closer to the fracture, thereby compressing the fracture by about 1 mm.
As the screw is inserted and centers within the plate hole, it moves the fragment closer to the fracture, thereby compressing the fracture by about 1 mm.
 The remaining screws are then drilled in the center of each hole (neutral position).
The remaining screws are then drilled in the center of each hole (neutral position).
Step 2 Pitfalls
Failure to prebend the plate will result in gapping at the fracture site at the opposite surface. If this situation occurs, it can be addressed with insertion of cancellous bone graft into the gap.
Inaccurate drilling of screw holes can result in distraction at the fracture when the screws are fully seated.
Axial compression with eccentric screw placement is not possible if done later in the fixation because the fragments already are fixed rigidly to the plate.
Step 3: Neutralization Plate
 A neutralization plate is applied after initial fracture compression with a lag screw.
A neutralization plate is applied after initial fracture compression with a lag screw.
 If the lag screw is to be applied through the dorsal surface of the metacarpal for a coronal fracture, the plate is applied first, and the lag screw is inserted through the plate hole.
If the lag screw is to be applied through the dorsal surface of the metacarpal for a coronal fracture, the plate is applied first, and the lag screw is inserted through the plate hole.
 The neutralization plate is contoured to adapt exactly to the dorsal surface of the bone. No prebending is necessary because the lag screw will prevent fracture distraction at the far cortex.
The neutralization plate is contoured to adapt exactly to the dorsal surface of the bone. No prebending is necessary because the lag screw will prevent fracture distraction at the far cortex.
 All screws must be inserted through the center of each hole to avoid inadvertent distraction at the fracture and stripping of the lag screw.
All screws must be inserted through the center of each hole to avoid inadvertent distraction at the fracture and stripping of the lag screw.
 The screws farthest from the fracture are inserted first to ensure alignment of the plate with the bone.
The screws farthest from the fracture are inserted first to ensure alignment of the plate with the bone.
 If a lag screw is to be inserted through the plate, it is done after initial stabilization of the plate and before completion of fixation.
If a lag screw is to be inserted through the plate, it is done after initial stabilization of the plate and before completion of fixation.
Step 4: Completion of Fixation
 Remaining screws are inserted.
Remaining screws are inserted.
 Radiographs are obtained to confirm that the fracture is reduced and compressed and the screw lengths are correct.
Radiographs are obtained to confirm that the fracture is reduced and compressed and the screw lengths are correct.
 The fingers are moved passively to ensure full range and to confirm rotational alignment.
The fingers are moved passively to ensure full range and to confirm rotational alignment.
Step 5: Wound Closure
Additional Steps
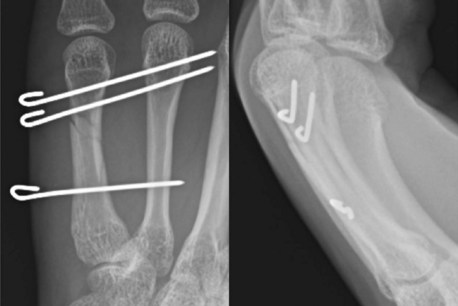
 Transverse pinning of a metacarpal shaft fracture is an alternative treatment for fractures that can be reduced by closed manipulation (Fig. 55-10).
Transverse pinning of a metacarpal shaft fracture is an alternative treatment for fractures that can be reduced by closed manipulation (Fig. 55-10).
 Fractures are usually angulated with the apex dorsal.
Fractures are usually angulated with the apex dorsal.
 Reduction is achieved by closing the fingers into a fist and stabilizing the hand with all digits in corrected rotation. A dorsally directed force is applied to the flexed proximal interphalangeal joint to push the distal metacarpal fragment dorsally.
Reduction is achieved by closing the fingers into a fist and stabilizing the hand with all digits in corrected rotation. A dorsally directed force is applied to the flexed proximal interphalangeal joint to push the distal metacarpal fragment dorsally.
 Reduction is achieved by resolution of the palpable bump and confirmed with an image intensifier.
Reduction is achieved by resolution of the palpable bump and confirmed with an image intensifier.
 With the surgeon holding the patient’s fingers in a closed fist with one hand, wires are introduced with the other.
With the surgeon holding the patient’s fingers in a closed fist with one hand, wires are introduced with the other.
 A stab incision for each K-wire is made over the subcutaneous border of the metacarpal shaft (ulnar for small finger and radial border of hand for index finger), followed by blunt dissection.
A stab incision for each K-wire is made over the subcutaneous border of the metacarpal shaft (ulnar for small finger and radial border of hand for index finger), followed by blunt dissection.
 Using a power driver, a K-wire is inserted transversely from the ulnar side of the small finger into the ring finger metacarpal close to the metaphalangeal joint. The wire is stopped at the ulnar cortex of the long finger metacarpal. Reduction and wire position are checked with imaging. Rotational alignment of the digit is checked again.
Using a power driver, a K-wire is inserted transversely from the ulnar side of the small finger into the ring finger metacarpal close to the metaphalangeal joint. The wire is stopped at the ulnar cortex of the long finger metacarpal. Reduction and wire position are checked with imaging. Rotational alignment of the digit is checked again.
 Two pins are inserted distal to the fracture site, and a third is inserted proximal to the fracture (Fig. 55-11).
Two pins are inserted distal to the fracture site, and a third is inserted proximal to the fracture (Fig. 55-11).
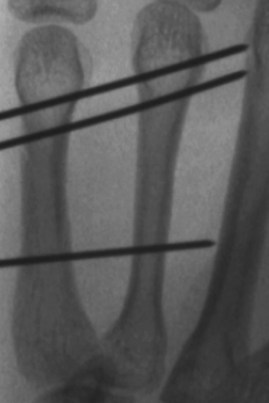
 Each K-wire should capture both cortices of the injured and neighboring uninjured metacarpal and abut against the next metacarpal shaft. The K-wire should go through four cortices and stop at the next intact one (Fig. 55-12). This will prevent late migration of the wire and ensure easy retrieval of the wires after 3 weeks.
Each K-wire should capture both cortices of the injured and neighboring uninjured metacarpal and abut against the next metacarpal shaft. The K-wire should go through four cortices and stop at the next intact one (Fig. 55-12). This will prevent late migration of the wire and ensure easy retrieval of the wires after 3 weeks.
 Maintenance of reduction and pin placement are confirmed fluoroscopically.
Maintenance of reduction and pin placement are confirmed fluoroscopically.
 K-wires are cut short and bent outside the skin for removal in the clinic.
K-wires are cut short and bent outside the skin for removal in the clinic.
Pearls
Attention to pain and edema control is essential in the early postoperative period.
Splinting with metacarpophalangeal joints in flexion is essential to prevent contracture.
When passing K-wire, it is important to count the number of cortices drilled to avoid incorrect trajectory of the K-wire. It should be confirmed that four cortices are passed and the K-wire stops at the outer cortex of the next intact metacarpal (fifth cortex).
Postoperative Care and Expected Outcomes
 The hand is rested in a plaster splint for the first 5 to 7 days after surgery.
The hand is rested in a plaster splint for the first 5 to 7 days after surgery.
 Following open reduction and plate fixation, active motion is commenced by the end of the first week after surgery. Between exercises, the injured digit and adjacent finger are immobilized in a thermoplastic splint in a functional intrinsic-plus position.
Following open reduction and plate fixation, active motion is commenced by the end of the first week after surgery. Between exercises, the injured digit and adjacent finger are immobilized in a thermoplastic splint in a functional intrinsic-plus position.
 If the fracture is treated with closed reduction and percutaneous fixation, the hand is immobilized in a cast for 3 weeks, with the concern that this mode of fixation is not rigid enough to initiate active motion within 1 week. Motion is started as described previously with a protective splint thereafter. The K-wires are removed in the clinic after 3 weeks.
If the fracture is treated with closed reduction and percutaneous fixation, the hand is immobilized in a cast for 3 weeks, with the concern that this mode of fixation is not rigid enough to initiate active motion within 1 week. Motion is started as described previously with a protective splint thereafter. The K-wires are removed in the clinic after 3 weeks.
 Most patients can be expected to regain functional motion after about 6 weeks and nearly full range of motion by 3 months.
Most patients can be expected to regain functional motion after about 6 weeks and nearly full range of motion by 3 months.
 Strengthening exercises are commenced after about 2 to 3 months when the fracture is nontender and the patient has satisfactory motion.
Strengthening exercises are commenced after about 2 to 3 months when the fracture is nontender and the patient has satisfactory motion.
Fusetti C, Meyer H, Borisch N, et al. Complications of plate fixation in metacarpal fractures. J Trauma. 2002;52:535-539.
Omokawa S, Fujitani R, Dohi Y, et al. Prospective outcomes of comminuted periarticular metacarpal and phalangeal fractures treated using a titanium plate system. J Hand Surg [Am]. 2008;33:857-863.
Ouellette EA, Freeland AE. Use of the minicondylar plate in metacarpal and phalangeal fractures. Clin Orthop Relat Res. 1996;327:38-46.
Page SM, Stern PJ. Complications and range of motion following plate fixation of metacarpal and phalangeal fractures. J Hand Surg [Am]. 1998;23:827-832.
Soeur JS, Mudgal CS. Plate fixation in closed ipsilateral multiple metacarpal fractures. J Hand Surg [Br]. 2008;33:740-744.