CHAPTER 55
Hip Osteoarthritis
Patrick M. Foye, MD; Todd P. Stitik, MD
Definition
Hip osteoarthritis (OA, also called degenerative joint disease) is the most prevalent pathologic condition at the hip joint. The hip joint (femoroacetabular joint) is a ball-and-socket joint, with the femoral head situated within the concavity formed by the acetabulum and labrum. This anatomic arrangement allows movements in multiple planes, including flexion, extension, adduction, abduction, internal rotation, and external rotation. Significant mechanical forces (three to eight times body weight) [1,2] are exerted on the hip joint during weight-bearing activities such as walking, running, jumping, and lifting. Additional stresses are created by recreational activities (e.g., impacts and falls during sports) and severe trauma (e.g., motor vehicle collisions). Hip trauma is significantly associated with unilateral but not bilateral hip OA, whereas obesity is associated with bilateral but not unilateral hip OA [3]. Occupational heavy lifting and frequent stair climbing seem to increase the risk of hip OA [4].
In a study of 2490 subjects aged 55 to 74 years, the prevalence of hip OA was 3.1%; 58% of hip OA cases were unilateral and 42% were bilateral [3]. The prevalence of hip OA is about 3% to 6% in the white population, but by contrast, it is far lower in Asian, black, and East Indian populations [5]. Total hip replacement in patients with hip OA is twice as common in women [6].
A central feature of hip OA is cartilage breakdown, thus compromising the femoroacetabular articulation. In addition to cartilage, other tissues affected by the disease process include subchondral bone, synovial fluid, ligaments, synovial membrane, joint capsule, and adjacent muscles. Eventually, the joint develops osteophytes (exostosis), joint space narrowing, bone sclerosis adjacent to the joint, and potentially even joint fusion (arthrosis). OA can be classified as either primary (idiopathic) or secondary [7]. The most common form of hip OA is primary [8], which represents the “wear and tear” degenerative changes that occur over time. Hip OA is considered secondary if a specific underlying cause can be identified, such as significant prior hip trauma, joint infection, or preexisting congenital or other deformities [7]. Among patients undergoing total hip replacement, the likelihood that the hip OA was primary (rather than secondary) is highest among white individuals (66%), followed by black subjects (54%), Hispanics (53%), and Asians (28%) [9]. Unlike rheumatoid arthritis, OA is relatively noninflammatory during most stages of the disease process. Symptomatic acetabular structural abnormalities can occur in patients with hip instability from classic developmental dysplasia or post-traumatic acetabular dysplasia as well as with retroversion of the acetabulum [10].
Symptoms
Groin pain is the classic manifesting symptom for hip OA. Other presenting symptoms of hip OA include hip pain, stiffness, and associated functional limitations. Many patients report “hip” pain when really they are referring to the superior lateral thigh region (e.g., greater trochanteric bursitis rather than hip joint disease). Hip joint pain typically presents as groin pain, perhaps with some referred pain down toward (and even beyond) the medial knee. Questioning the patient about lumbosacral, sacroiliac, or coccyx pain may reveal that the “hip” symptoms are actually referred from the spine. Hip OA pain usually has an insidious onset, is worse with activity (particularly weight bearing and rotational loading of the joint), and is somewhat relieved with rest [7]. Advanced OA may be painful even at rest [7]. The physician should specifically ask about any constitutional symptoms that might suggest infection or malignant disease and also about any history of hip trauma [11] (recent or remote).
Physical Examination
Antalgic gait is characterized by a limp with decreased single-limb stance time on the painful limb, a shortened stride length for the contralateral limb, and an increased double support time.
Range of motion should be evaluated not only at both hip joints (in multiple planes) but also at the lumbosacral spine, knees, and ankles to more thoroughly evaluate the kinetic chain. The earliest sign of hip OA is loss of hip internal rotation [12,13]. Limping, groin pain, or limited hip internal rotation supports a diagnosis of a hip (rather than spine) disorder [14], but it still remains prudent also to perform a lumbosacral physical examination when lumbosacral pain generators are being considered. Whereas no one physical examination maneuver is diagnostic of hip OA or other form of intra-articular hip disease, assessment for painful range of motion about the hip, palpation, manual muscle testing, screening for radiculopathy and neuropathy, observation for systemic signs of OA, and performance of a provocative maneuver known as the Patrick test represent a reasonable evaluation. The Patrick test is performed by having the patient supine with the ipsilateral heel on the contralateral knee, thus forming the figure four position, also referred to by the acronym FABER (hip flexed, abducted, and externally rotated) maneuver (Fig. 55.1). The physician pushes the raised leg toward the table, producing groin pain that suggests intra-articular hip disease or back or buttock pain that suggests sacroiliac joint disease.

Palpation of the tissues about the greater trochanteric region, proximal iliotibial bands, sacroiliac joints, gluteal muscles, underlying piriformis and obturator internus muscles, and ischial bursae may reveal pain generators other than the hip joint itself.
Weak hip girdle muscles may be due to pain or disuse, but radiculopathy and neuropathy can also be considered. Hip abductor weakness may be manifested with a Trendelenburg gait [13]. With hip OA, the remainder of the neurologic examination in the lower limbs is normal (e.g., muscle stretch reflexes and sensory testing).
On inspection of the fingers, hypertrophic degenerative changes (exostoses), such as Heberden nodes at the distal interphalangeal joints [12], are independent risk factors for hip OA [11]. Their presence thus increases the likelihood of similar findings at the hip joint.
Functional Limitations
Patients with hip OA often report functional limitations in weight-bearing activities such as walking, running, and climbing stairs. The hip range of motion restrictions may cause difficulties with activities such as donning or doffing socks and shoes, picking up clothing from the floor [15], and getting in and out of cars. Hip pain and weakness may necessitate use of the upper limbs to arise from a chair [15]. A careful history can elicit details of occupational, recreational, and other functional activities that the patient has decreased or ceased because of the hip OA.
Diagnostic Studies
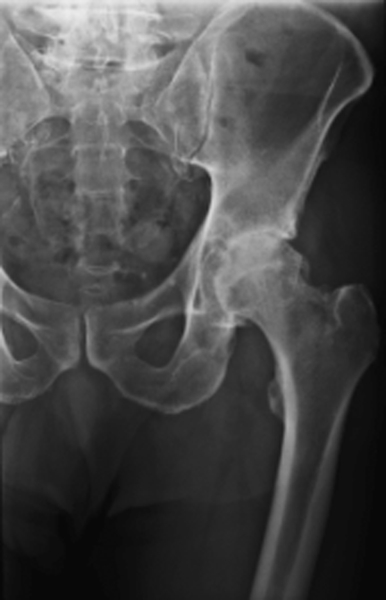
Plain radiography is the primary diagnostic study for hip OA [16] (Fig. 55.2). The severity of radiographic hip OA findings can be categorized on the basis of the minimal joint space (MJS), defined as the shortest distance on the radiograph between the femoral head margin and the acetabular edge [15]. MJS is determined by four joint space measurements (medial, lateral, superior, and axial). Croft’s MJS grades are 0 (MJS > 2.5 mm), 1 (MJS > 1.5 mm and ≤ 2.5 mm), and 2 (MJS ≤ 1.5 mm) [15]. MJS is predictive of hip pain, is strongly associated with other radiographic features of hip OA, and has a high inter-rater reliability [17]. Alternatively, the Kellgren-Lawrence grading system of hip OA is a scale of 0 to 5 that considers not only joint space narrowing but also three additional factors: presence of osteophytes, subchondral sclerosis, and subchondral cysts [15]. Both MJS and Kellgren-Lawrence grade are associated with clinical symptoms of hip OA [15].
Magnetic resonance imaging is generally not needed to diagnose hip OA, but it is superior to radiography or bone scan when the differential diagnosis includes avascular necrosis or hip labral tear [18]. Hip joint arthrography is also generally unnecessary for the diagnosis of hip OA but may help define labral tears. Diagnostic musculoskeletal ultrasound can assist in early detection of hip OA, can sometimes demonstrate gross evidence of bone and cartilage damage, can detect associated synovitis [19], and can detect concomitant iliopsoas bursitis [20]. Hip pain that is relieved through intra-articular diagnostic injection of local anesthetic (e.g., with ultrasound [21] or fluoroscopic guidance) can help confirm that the patient’s symptoms are arising from the hip joint and predicts a good surgical outcome with joint replacement [21]. Patients who fail to obtain adequate relief with image-guided anesthetic injection tend to have alternative pathologic processes at the spine (61%) or knee (16%) [21].
Electrodiagnostic studies should be considered when the differential diagnosis includes lumbosacral radiculopathy or peripheral nerve disease.
Treatment
Initial
Patients with OA should be educated about their diagnosis, prognosis, and available treatments. Patients are encouraged to take an active role in managing their OA and maximizing their outcomes [22].
Weight loss is important because body weight is an independent risk factor for the development and progression of hip OA [23,24], although this relationship is less clearly established at the hip than at the knee [12]. Forces on the hip joint are roughly three to five times the patient’s body weight during ambulation [2] and up to eight times body weight during jogging [1]. Loss of even modest amounts of excess body weight can significantly decrease lower extremity joint forces, OA progression, and related symptoms [23,24].
The initial medication of choice for OA is acetaminophen [25,26], at a maximum dose of 1000 mg three times a day, depending on the presence or absence of hepatic dysfunction. Although OA is primarily considered a noninflammatory arthritis (at least in early stages), prescription of nonsteroidal anti-inflammatory drugs in addition to the acetaminophen can provide further analgesic benefit [12]. Diagnostic musculoskeletal ultrasound offers the clinician a practical way of quickly assessing for evidence of inflammation and thus potentially influencing medication selection. In appropriately selected patients, tramadol or more traditional opioid analgesics may also be used for pain relief and associated functional benefits [12].
Rehabilitation
The American College of Rheumatology guidelines for the medical management of hip and knee OA recommend exercise as an important component of treatment [24,25]. These guidelines recommend an exercise program consisting of range of motion, muscle strengthening, and aerobic conditioning by walking or aquatic therapy [24,25]. Water-based exercise for lower limb OA decreases pain and increases function in the short term and also at 1 year [27].
Stretching programs can address the range of motion restrictions in patients with hip OA, which are, in order of severity, extension, internal rotation, abduction, external rotation, adduction, and flexion [22]. Flexibility programs often begin with patients gently moving their joints through the available range of motion (to maintain range of motion) and then progress to regaining of lost range of motion. [12] Proper stretching should be sustained for at least 30 seconds while avoiding the sudden, jerky, or ballistic stretching that would be likely to exacerbate OA [12].
Muscle strengthening programs should address all planes of hip movement [22]. OA patients may begin with static strengthening exercises [12] to minimize joint movements that could exacerbate the OA symptoms [12]. Eventually, incorporation of dynamic exercises can maximize strength and function [12]. Patients with hip OA are often deconditioned, thus suggesting a role for aerobic exercises [22]. Because OA particularly affects the elderly, it is especially important to screen for cardiovascular or other precautions before an exercise program is begun. Many patients with hip OA may have difficulty tolerating high-impact aerobics, such as jogging and stair climbing [22], so activities such as cycling (perhaps using a high-seat bike or recumbent bike, depending on the patient’s symptoms) and aquatic exercises may be substituted. It is important to encourage ongoing exercise compliance [8,12].
There is little clinical scientific evidence supporting passive modalities (e.g., cryotherapy, thermotherapy, transcutaneous electrical nerve stimulation) for hip OA [22], although theoretically they may facilitate better tolerance of the active therapy program [12]. A recent literature review by a European multispecialty panel of experts concluded that massage, therapeutic ultrasound, electrotherapy, electromagnetic field, and low-level laser therapy cannot be recommended in hip OA [28].
Hip OA pain may be decreased by use of a cane in the contralateral hand [8,13], presumably by shifting the center of gravity medially, away from the involved hip. In cases of bilateral hip OA, the cane can be used contralateral to the more severely involved hip. A shoe lift can correct a leg length discrepancy [8] caused by hip joint space narrowing or superior migration of the femoral head within the acetabulum.
An occupational therapy evaluation of activities of daily living may identify difficulties with hand activities (e.g., due to hand OA) and difficulties with donning and doffing footwear (due to restricted hip range of motion). Adaptive equipment (e.g., reachers, sock donners, long-handled shoe horns, elastic shoelaces) may help maximize independence despite persistent physical impairments [12].
Procedures
Nonsurgical procedures for hip OA primarily include intra-articular injections with corticosteroids or viscosupplements.
Corticosteroid Injections
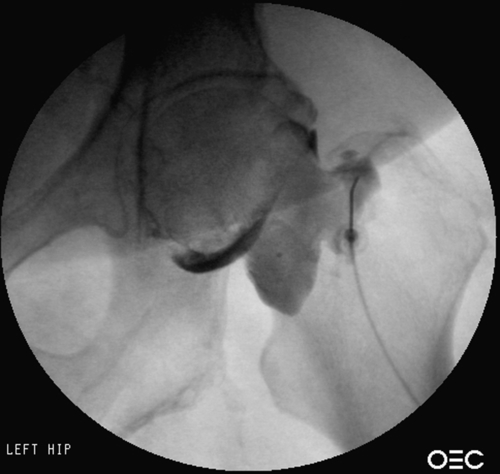
Although early OA is considered relatively noninflammatory, end-stage OA may have an inflammatory component [7], which may provide a basis for anti-inflammatory intra-articular injections with corticosteroids. It is difficult to obtain true intra-articular hip joint injection without fluoroscopy [8,12] or other image guidance such as ultrasound [21,29], particularly because the hip joint cannot be palpated and is adjacent to important neurovascular structures [29]. Also, OA can decrease the targeted joint space and osteophytes can obstruct needle entry [30]. A randomized controlled trial of fluoroscopically guided intra-articular hip joint injections has shown that compared with local anesthetic, corticosteroids decrease hip OA pain (at 3- and 12-week follow-up), improve hip range of motion in all directions, and significantly improve functional abilities [31]. Ultrasound-guided hip joint corticosteroid injection for hip OA has shown significant relief of pain during walking compared with saline injection [32]. Another prospective study of ultrasound-guided corticosteroid injection for hip OA showed that compared with baseline, there is significantly decreased walking pain at 1 and 3 months after injection [33] and 75% of the hips show decreased synovial hypertrophy at 1 and 3 months after injection [33]. Even in patients with advanced hip OA waiting for total hip replacement, image-guided intra-articular steroid injection can provide months of improved pain and function [34]. Despite the benefits shown in prospective, randomized controlled trials [31,32], it is notable that one retrospective study seems to show that combined injections of corticosteroid, contrast agent, and anesthetic before total hip arthroplasty may increase the risk of postoperative infection and surgical revision [35]. Despite the limitations of that study (inherent flaws of a retrospective review and data lacking statistical power to determine the role of the time interval between steroid injection and subsequent total hip arthroplasty) [35], the possibility of infection should be discussed with patients before corticosteroid injection. Hip joint injection under fluoroscopic guidance is shown in Figure 55.3.
Viscosupplementation Injections
True intra-articular placement is even more important with viscosupplementation than with corticosteroids because viscosupplements have high molecular weights and are unlikely to permeate to the joint capsule [30]. Thus, when it is available, image guidance with fluoroscopy [30] or ultrasonography seems prudent for viscosupplementation injections [35].
At the time of this writing, viscosupplements are approved by the Food and Drug Administration only for use at the knee. Some initial studies indicate that image-guided hip joint viscosupplementation injections are well tolerated, safe, and beneficial for hip OA [36]. Image-guided intra-articular hip viscosupplementation injections in symptomatic hip OA patients seems to effectively delay the need for total hip replacement surgery, thus decreasing OA-related financial costs and decreasing mortality related to total hip replacement [37]. A literature review concluded that viscosupplementation is as effective for hip OA as for knee OA, appears to be a reasonable and safe alternative to oral nonsteroidal anti-inflammatories, and appears to work best in patients with milder radiographic findings of OA [38].
Surgery
Surgical treatment of hip OA (see Chapter 61) includes joint realignment (realignment osteotomy, such as for hip dysplasia [13]), joint fusion (arthrodesis), and, most commonly, joint replacement (arthroplasty) [26]. Hip joint arthroplasty can be categorized as either hemiarthroplasty (prosthetic replacement of the proximal femur while the acetabulum is left intact) or total hip arthroplasty (also called total hip replacement, with surgical replacement of both the acetabulum and the proximal femur) [26]. Hip hemiarthroplasty is often performed after proximal femur fractures, when the acetabulum is relatively intact. Conversely, in OA, there is usually degeneration of both the acetabulum and the femur; thus, the definitive surgery is to replace both of these through total hip arthroplasty. An arthroplasty can also be categorized on the basis of the specific prosthetic hardware used (e.g., unipolar or bipolar) and whether cement is used to hold the hardware in place [26]. Comparisons of the posterior and direct lateral surgical approaches for total hip arthroplasty show similar rates of postoperative dislocation (1% to 4%), postoperative Trendelenburg gait, and sciatic nerve injury [39].
Customized preoperative exercises are well tolerated even in patients with end-stage hip OA and improve early recovery of physical function after eventual total hip arthroplasty is performed [40]. Postoperative rehabilitation with physical therapy (and perhaps occupational therapy) generally includes therapeutic exercise, transfer training, gait training, and instruction in activities of daily living [41]. After total hip arthroplasty, early ambulation (even within the first 1 to 2 days postoperatively) [8] may maximize recovery and minimize complications such as deep venous thrombosis and symptomatic thromboembolism [41].
The patient is taught how to follow the weight-bearing status specified by the orthopedic surgeon [8], which depends on factors such as whether the prosthesis was cemented in place [41]. Many patients may safely bear weight as tolerated [41]. A cane or walker should be used until hip abductors are strong enough that the patient no longer limps during unassisted gait [8]. After a posterior approach total hip arthroplasty, prevention of hip dislocation often involves “hip precautions” (e.g., teaching the patient to carefully avoid positions of hip adduction, flexion, and internal rotation) [8]. Patients are taught to use elevated chair seats and elevated toilet seats and to avoid crossing the legs [8]. The recommended duration for hip precautions varies widely from 6 weeks to 6 months. Postoperative patients with a significant fall or sudden onset of pain should undergo radiography for evaluation of dislocation.
Prophylaxis against deep venous thrombosis and related venous thromboembolism may include early ambulation, intermittent pneumatic compression stockings, inferior vena cava filters, and pharmacologic methods (such as unfractionated heparin, low-molecular-weight heparin, warfarin, or synthetic pentasaccharides) [41]. The optimal duration of thromboprophylaxis is not known, but a 4- to 6-week course has been suggested after total hip arthroplasty [41].
After the acute care hospital, total hip arthroplasty patients are discharged to either inpatient rehabilitation (acute or subacute) or directly home, depending on postoperative pain, functional status, and home environment [8,41].
Potential Disease Complications
Hip OA is a degenerative process characterized by gradual progressive worsening of femoroacetabular joint destruction and resultant symptoms. Hip OA can produce severe pain, stiffness, functional limitations, and associated compromise of quality of life. The decrease in mobility can subsequently result in weakness, osteoporosis, obesity, and cardiovascular deconditioning.
Potential Treatment Complications
Acetaminophen can cause hepatic side effects; nonsteroidal anti-inflammatory drugs are associated with gastrointestinal, renal, and cardiovascular risks. Tramadol can cause sedation and dizziness. Hip injections carry risks of infection and postprocedure exacerbation of symptoms. Hip replacement surgeries can be complicated by infection, nerve injury, dislocation, hardware loosening, deep venous thrombosis, and anesthesia-related side effects [41].







