CASE 55

History: A patient presents with chest pain.
1. What are the causes of acute aortic syndrome? (Choose all that apply.)
A. Aneurysm
B. Dissection
2. What is the most likely diagnosis?
A. Aneurysm
B. Dissection
3. What is the most likely cause of this finding?
A. Rupture of the vasa vasorum
B. Communication with the aortic lumen
C. Trauma
4. Which of the following is not an appropriate management of this patient?
A. No treatment
B. Antihypertensive medication
D. Surgery
ANSWERS
References
Chin AS, Fleischmann D. State-of-the-art computed tomography angiography of acute aortic syndrome. Semin Ultrasound CT MR. 2012;33(3):222–234.
Reddy GP, Gunn M, Mitsumori LM, et al. Multislice CT and MRI of the thoracic aorta. In: Webb WR, Higgins CB, eds. Thoracic imaging: pulmonary and cardiovascular radiology. ed 2 Philadelphia: Lippincott Williams & Wilkins; 2010.
Cross-Reference
Cardiac Imaging: The REQUISITES, ed 3, p 411.
Comment
Acute Aortic Syndrome
Acute aortic syndrome is suspected in the setting of hypertension and chest pain radiating to the back. Acute aortic syndrome can be caused by aortic dissection, intramural hematoma, and penetrating aortic ulcer.
Etiology and Management
An intramural hematoma is most commonly caused by rupture of the vasa vasorum, the arteries that supply the aortic wall. The ruptured vessels bleed into the aortic wall, which can result in an intimal tear and separation of the wall—a classic dissection. If the intima does not separate, an intramural hematoma remains. The intramural hematoma may remain localized, or it can extend along the wall in an antegrade or a retrograde direction or rarely rupture through the adventitia. Intramural hematoma can be considered to be a type of dissection, and treatment is similar to treatment of a frank dissection. Stanford type B intramural hematoma (not involving the ascending aorta) is usually managed medically. Traditionally, type A intramural hematoma (not involving the ascending aorta) is treated with surgery. In recent years, some surgeons have begun to manage type A hematoma conservatively with antihypertensive medication and close observation. Patients who develop pericardial hemorrhage, aortic valve regurgitation, or extension of hematoma into the coronary or arch vessels need surgery.
Imaging
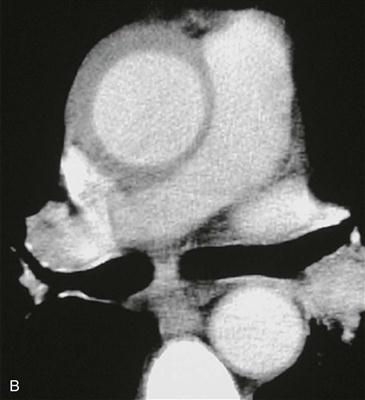
Non–contrast-enhanced CT scan shows characteristic high-density thickening of the aortic wall, indicating intramural hematoma (Fig. A). Contrast-enhanced CT scan shows the thickening of the wall, but the high density may be difficult to appreciate (Fig. B). On MRI, the signal intensity is intermediate to high on black blood sequences. Relying solely on gadolinium-enhanced magnetic resonance angiography (MRA) can be risky in the setting of dissection because an intramural hematoma can be overlooked on this sequence.