CHAPTER 54 Trauma
3 What is the significance of Glasgow Coma Scale (GCS) score of 8?
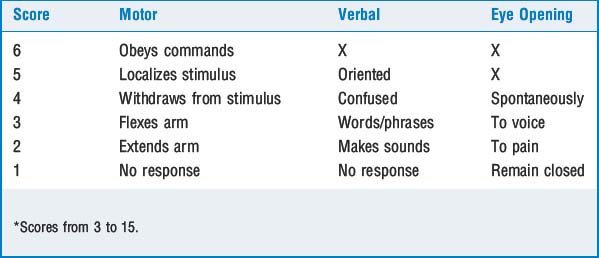
The GCS is an assessment for patients with head injury. The final score is the sum of scores for best eye opening, best motor and best verbal responses; scores range from 3 to 15. Generally, the GCS for severe head injury is 9 or less; for moderate injury, 9–12; and for minor injury, 12 and higher. A patient with a GCS of 8 is sufficiently depressed that endotracheal intubation is indicated (see Table 54-1).
13 How does cardiac tamponade present? What is Beck’s triad? How should anesthesia be managed in a patient with tamponade?
18 Describe the presentation of a myocardial contusion
KEY POINTS: Trauma 
21 How might a bronchial or tracheal tear present? What are alternatives for managing ventilation during operative repair?
1. Bonatti H., Calland J.F. Trauma. Emerg Med Clin North Am. 2008;26:625-648.
2. Cereda M., Weiss Y.G., Deutschman C.S. The critically ill injured patient. Anesthesiol Clin. 2007;25:13-21.
3. Holcomb J.B., Jenkins D., Rhee P., et al. Damage control resuscitation: directly addressing the early coagulopathy of trauma. J Trauma. 2007;62:307-310.