Procedure 54 Metacarpal Neck Fractures
Examination/Imaging
Clinical Examination
 Note swelling and bruising over the dorsum of the hand.
Note swelling and bruising over the dorsum of the hand.
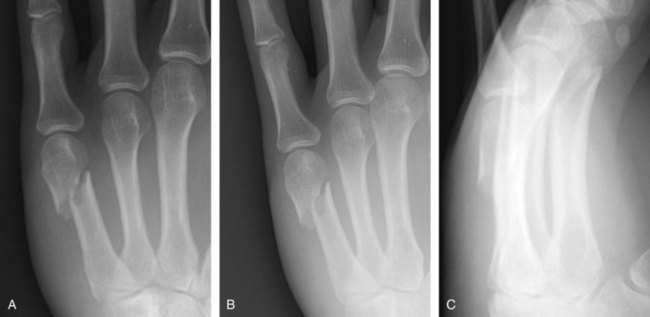
 Look carefully for any wounds—may indicate an open fracture (Fig. 54-1).
Look carefully for any wounds—may indicate an open fracture (Fig. 54-1).
 Look carefully for rotational deformity with fingers flexed and compared with opposite hand (Fig. 54-2).
Look carefully for rotational deformity with fingers flexed and compared with opposite hand (Fig. 54-2).
 Ensure circulation is adequate by checking capillary refill.
Ensure circulation is adequate by checking capillary refill.
 Test and document digital sensation.
Test and document digital sensation.
 Ask patient to flex and extend interphalangeal joints within limits of pain to confirm continuity of flexor and extensor tendons.
Ask patient to flex and extend interphalangeal joints within limits of pain to confirm continuity of flexor and extensor tendons.
Surgical Anatomy
 Metacarpals can be easily accessed through the dorsal approach.
Metacarpals can be easily accessed through the dorsal approach.
 Dorsal cutaneous nerves are located in the subcutaneous plane. The dorsal cutaneous branch of the ulnar nerve winds around the ulnar border of the hand 1 cm distal to the ulnar head and then divides into its branches at the level of the small finger carpometacarpal joint.
Dorsal cutaneous nerves are located in the subcutaneous plane. The dorsal cutaneous branch of the ulnar nerve winds around the ulnar border of the hand 1 cm distal to the ulnar head and then divides into its branches at the level of the small finger carpometacarpal joint.
 The extensor tendons are surrounded by paratenon and can be easily separated by dividing the juncturae tendinum that interconnect them at the level of the metacarpal necks.
The extensor tendons are surrounded by paratenon and can be easily separated by dividing the juncturae tendinum that interconnect them at the level of the metacarpal necks.
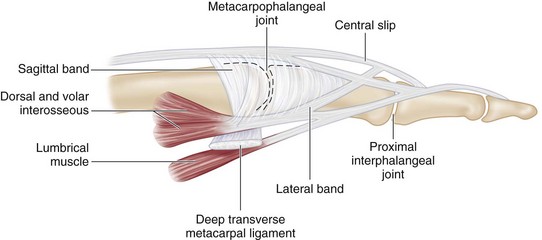
 The extensor hood envelops the distal part of the metacarpal. Plate placement at this level can interfere with gliding of the hood (Fig. 54-5).
The extensor hood envelops the distal part of the metacarpal. Plate placement at this level can interfere with gliding of the hood (Fig. 54-5).
Positioning
Exposures
 For open plating, a longitudinal incision is centered over the metacarpal neck. The incision is on the dorsum for the long and ring fingers. For the border digits—index and small fingers—the incision is on the midlateral line and then curves dorsally at the metacarpophalangeal joint (Fig. 54-6).
For open plating, a longitudinal incision is centered over the metacarpal neck. The incision is on the dorsum for the long and ring fingers. For the border digits—index and small fingers—the incision is on the midlateral line and then curves dorsally at the metacarpophalangeal joint (Fig. 54-6).
 For intramedullary pinning, the incision is placed at the metacarpal base (Fig. 54-7).
For intramedullary pinning, the incision is placed at the metacarpal base (Fig. 54-7).
 The periosteum at the fracture site is elevated circumferentially to allow accurate reduction without soft tissue interposition.
The periosteum at the fracture site is elevated circumferentially to allow accurate reduction without soft tissue interposition.
Pearls
For plating of adjacent metacarpals, a single skin incision between the metacarpals will allow access to both fractures.
Careful spreading dissection is necessary after skin incision to preserve subcutaneous nerves and veins.
Paratenon around extensor tendons must be preserved to minimize postoperative tendon adhesions.
With exposure for intramedullary pinning of the small finger, particular care must be taken to identify and preserve the dorsal branch of the ulnar nerve.
In case of excessive comminution, the periosteum around the fracture is left intact, and the implant is secured distally and proximally (bridge plating).
Procedure
Step 1: Preparation of Plate and Insertion of Blade
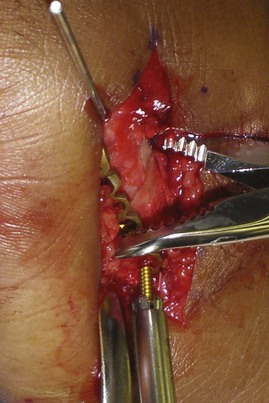
 Achieve provisional reduction and stabilize with a K-wire (Fig. 54-8).
Achieve provisional reduction and stabilize with a K-wire (Fig. 54-8).
 Select the appropriate-sized condylar plate.
Select the appropriate-sized condylar plate.
 The plate is held against the fracture, and the required length of plate is determined. The plate is cut to appropriate length (Fig. 54-9).
The plate is held against the fracture, and the required length of plate is determined. The plate is cut to appropriate length (Fig. 54-9).
 The blade hole is drilled first in the metacarpal head. The plate is rotated such that the blade is pointing away from the bone, and the plate hole adjacent to the blade is drilled with the drill directed parallel to the blade (Fig. 54-10).
The blade hole is drilled first in the metacarpal head. The plate is rotated such that the blade is pointing away from the bone, and the plate hole adjacent to the blade is drilled with the drill directed parallel to the blade (Fig. 54-10).
 The hole is measured, and the blade is cut to the appropriate length.
The hole is measured, and the blade is cut to the appropriate length.
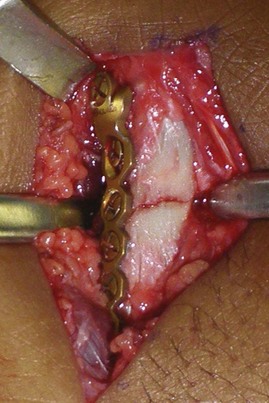
 The blade is inserted into the hole, and the plate is approximated with the shaft using a bone clamp (Fig. 54-11).
The blade is inserted into the hole, and the plate is approximated with the shaft using a bone clamp (Fig. 54-11).
Step 2: Alignment of Plate with Shaft
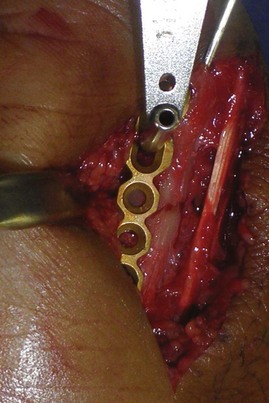
 The plate is aligned with the shaft, and fracture reduction is confirmed (Fig. 54-12).
The plate is aligned with the shaft, and fracture reduction is confirmed (Fig. 54-12).
 The plate must be contoured well along the shaft.
The plate must be contoured well along the shaft.
 The most proximal screw in the shaft is inserted first to secure the plate to the shaft (Fig. 54-13).
The most proximal screw in the shaft is inserted first to secure the plate to the shaft (Fig. 54-13).
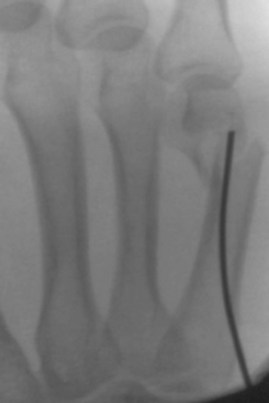
 Rotational alignment of the finger is checked clinically, and reduction and plate position are checked radiographically (Figs. 54-14 and 54-15).
Rotational alignment of the finger is checked clinically, and reduction and plate position are checked radiographically (Figs. 54-14 and 54-15).
 The screw adjacent to the blade is then inserted after drilling.
The screw adjacent to the blade is then inserted after drilling.
Step 3: Compression of the Fracture
 It is helpful to gain compression of a short oblique or transverse fracture to enhance stability.
It is helpful to gain compression of a short oblique or transverse fracture to enhance stability.
 Longitudinal compression is achieved by eccentric drilling in the oval hole of the plate. If the screw hole is drilled away from the fracture site, compression is achieved as the screw is inserted and tightened (Fig. 54-16).
Longitudinal compression is achieved by eccentric drilling in the oval hole of the plate. If the screw hole is drilled away from the fracture site, compression is achieved as the screw is inserted and tightened (Fig. 54-16).
 The screw adjacent to the blade is inserted after drilling (Fig. 54-17).
The screw adjacent to the blade is inserted after drilling (Fig. 54-17).
 In a short oblique fracture, additional compression can be achieved with a lag screw inserted through the plate. To insert a lag screw, the gliding hole is drilled in the near cortex (same diameter as the outer screw diameter—2.0 mm drill for a 2 mm screw). The thread hole (1.5 mm for a 2 mm screw) is drilled in the far cortex (Fig. 54-18).
In a short oblique fracture, additional compression can be achieved with a lag screw inserted through the plate. To insert a lag screw, the gliding hole is drilled in the near cortex (same diameter as the outer screw diameter—2.0 mm drill for a 2 mm screw). The thread hole (1.5 mm for a 2 mm screw) is drilled in the far cortex (Fig. 54-18).
Step 3 Pitfalls
When placing a screw across the fracture for compression, failure to drill near the cortex with a gliding hole may result in distraction rather than compression.
Axial compression with eccentric screw placement is not possible if done later in the fixation as the fragments are fixed rigidly to the plate.
Step 4: Completion of Fixation
 Remaining screws are inserted (Fig. 54-19).
Remaining screws are inserted (Fig. 54-19).
 Radiographs are obtained to confirm that the fracture is reduced and compressed and the screw lengths are correct (Fig. 54-20).
Radiographs are obtained to confirm that the fracture is reduced and compressed and the screw lengths are correct (Fig. 54-20).
 The fingers are moved passively to ensure that full range and rotational alignment is confirmed.
The fingers are moved passively to ensure that full range and rotational alignment is confirmed.
Step 5: Wound Closure
Additional Steps
 Intramedullary pinning of a metacarpal subcapital fracture provides an alternative to open plating with an advantage of percutaneous fixation.
Intramedullary pinning of a metacarpal subcapital fracture provides an alternative to open plating with an advantage of percutaneous fixation.
 A 2-cm incision is made just proximal to the base of the metacarpal.
A 2-cm incision is made just proximal to the base of the metacarpal.
 Cutaneous nerves are identified and protected.
Cutaneous nerves are identified and protected.
 Using a soft tissue protector, a 2-mm hole is drilled obliquely aiming distally and centrally toward the medullary cavity. A small awl can be used to enlarge the hole (Fig. 54-21).
Using a soft tissue protector, a 2-mm hole is drilled obliquely aiming distally and centrally toward the medullary cavity. A small awl can be used to enlarge the hole (Fig. 54-21).
 A 1.5-mm K-wire is selected and cut to 1 cm longer than the estimated length of the metacarpal. A gentle 30-degree curve is made over a distance of 1 cm at the blunt end of the wire. A 90-degree bend is made over a 1-cm segment in the opposite end of the wire. Both bends are in the same plane (Fig. 54-22).
A 1.5-mm K-wire is selected and cut to 1 cm longer than the estimated length of the metacarpal. A gentle 30-degree curve is made over a distance of 1 cm at the blunt end of the wire. A 90-degree bend is made over a 1-cm segment in the opposite end of the wire. Both bends are in the same plane (Fig. 54-22).
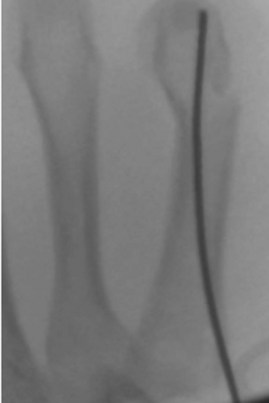
 The prebent wire is introduced manually into the medullary cavity and passed up to the fracture site under radiographic control (Fig. 54-23). The fracture angulation is then corrected by dorsally directed force on the maximally flexed metacarpophalangeal joint (Fig. 54-24).
The prebent wire is introduced manually into the medullary cavity and passed up to the fracture site under radiographic control (Fig. 54-23). The fracture angulation is then corrected by dorsally directed force on the maximally flexed metacarpophalangeal joint (Fig. 54-24).
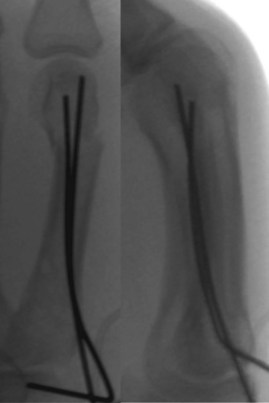
 The wire is then advanced across the fracture and right up to the subchondral bone of the metacarpal head while the corrective force is maintained (Fig. 54-25).
The wire is then advanced across the fracture and right up to the subchondral bone of the metacarpal head while the corrective force is maintained (Fig. 54-25).
 Rotational alignment is clinically examined, and reduction is confirmed radiographically.
Rotational alignment is clinically examined, and reduction is confirmed radiographically.
 A second wire is then passed in a similar fashion with the curve facing opposite the first wire (Fig. 54-26).
A second wire is then passed in a similar fashion with the curve facing opposite the first wire (Fig. 54-26).
 In a large or osteopenic bone with wide medullary cavity, insertion of three or four pins may be possible.
In a large or osteopenic bone with wide medullary cavity, insertion of three or four pins may be possible.
 The wires are cut close to the bone, and skin is closed with interrupted sutures.
The wires are cut close to the bone, and skin is closed with interrupted sutures.
Pearls
Initial drilling must be directed obliquely to engage the medullary cavity of the bone.
Attention to the bending of the wires is essential to allow easy passage.
Manual insertion ensures that the wires engage the medullary cavity.
When negotiating the fracture, the wire tends to exit the dorsal side of the fracture. This can be avoided by turning the pin so that the curve points in a palmar direction.
Postoperative Care and Expected Outcomes
 The hand is rested in a splint for the first 5 to 7 days after surgery (Fig. 54-27).
The hand is rested in a splint for the first 5 to 7 days after surgery (Fig. 54-27).
 Following open reduction and plate fixation, active motion is commenced by the end of the first week after surgery. Between exercises, the hand is rested in a thermoplastic splint in a functional intrinsic-plus position (Fig. 54-28).
Following open reduction and plate fixation, active motion is commenced by the end of the first week after surgery. Between exercises, the hand is rested in a thermoplastic splint in a functional intrinsic-plus position (Fig. 54-28).
 If the fracture is treated with closed reduction and percutaneous fixation, the hand is immobilized in a cast for 3 weeks. Motion is started as described previously with a protective splint thereafter.
If the fracture is treated with closed reduction and percutaneous fixation, the hand is immobilized in a cast for 3 weeks. Motion is started as described previously with a protective splint thereafter.
 Most patients can be expected to regain functional motion after about 6 weeks and nearly full range of motion by 3 months.
Most patients can be expected to regain functional motion after about 6 weeks and nearly full range of motion by 3 months.
 Strengthening exercises are commenced after about 2 to 3 months when the fracture is nontender and the patient has satisfactory motion.
Strengthening exercises are commenced after about 2 to 3 months when the fracture is nontender and the patient has satisfactory motion.
Foucher G. “Bouquet” osteosynthesis in metacarpal neck fractures: a series of 66 patients. J Hand Surg [Am]. 1995;20:S86-S90.
Ouellette EA, Freeland AE. Use of the minicondylar plate in metacarpal and phalangeal fractures. Clin Orthop Relat Res. 1996;327:38-46.
Schädel-Höpfner M, Wild M, Windolf J, Linhart W. Antegrade intramedullary splinting or percutaneous retrograde crossed pinning for displaced neck fractures of the fifth metacarpal? Arch Orthop Trauma Surg. 2007;127:435-440.
Wong TC, Ip FK, Yeung SH. Comparison between percutaneous transverse fixation and intramedullary K-wires in treating closed fractures of the metacarpal neck of the little finger. J Hand Surg [Br]. 2006;31:61-65.