CASE 54 Left Subclavian Stenosis
Cardiac catheterization
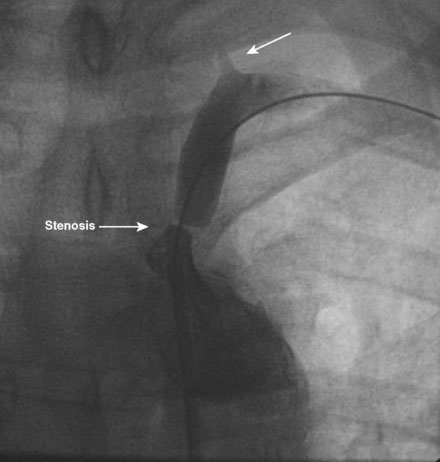
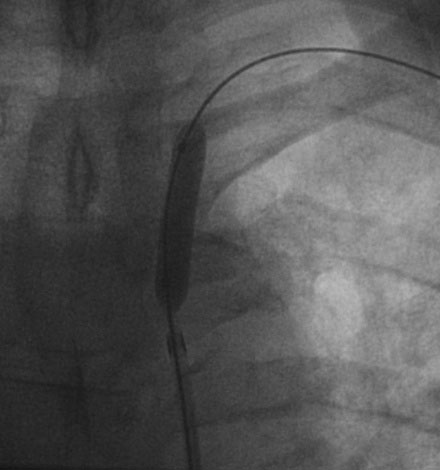
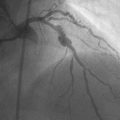
Angiography of the left subclavian artery revealed a severe stenosis of the subclavian artery proximal to any branches and with clear evidence of left vertebral steal evidenced by absence of anterograde flow in the left vertebral artery (Figure 54-1 and Video 54-1). The operator planned to stent this lesion and positioned a 7 French, 90 cm long sheath in the proximal subclavian artery. Procedural anticoagulation was accomplished with a bolus and infusion of bivalirudin. The lesion was first crossed with a 0.035 inch angled glide wire and a 4 French catheter was placed across the lesion; simultaneous pressure measurements proximal and distal to the stenosis recorded a 30 mmHg systolic pressure gradient across the lesion. The glide wire was exchanged for a 0.035 inch, 300 cm long angled Storq wire and a 7 mm diameter by 3 cm long, 0.035 inch, compatible, over-the-wire balloon was advanced to the stenosis and inflated (Figure 54-2). Balloon dilatation restored anterograde flow to the left vertebral artery, but a significant residual stenosis remained (Video 54-2). The operator exchanged the balloon catheter for a 8 mm diameter by 24 mm long balloon-expandable biliary stent and achieved an excellent angiographic result with no residual pressure gradient noted (Figure 54-3 and Video 54-3). There was prompt restoration of the radial pulse noted, with no evidence of distal embolization.
Postprocedural course
After an overnight period of observation, he was discharged the next morning. While still in the hospital, he noted immediate improvement in arm strength and no longer noted arm claudication. At 3 month and 1 year follow-up, he remained completely asymptomatic with equal blood pressures in both arms. Eighteen months after the subclavian stent was placed, he developed atypical chest pain and underwent cardiac catheterization. This showed no significant coronary lesions, and arch aortography confirmed wide patency of the subclavian stent (Figure 54-4).
Discussion
Subclavian stenosis is an uncommon manifestation of peripheral vascular disease. Left subclavian disease is more common than disease in the innominate artery or right subclavian artery. Although the overall prevalence of this condition is not entirely clear, significant left subclavian stenosis is present in 2% of the general population, in about 7% of patients referred to a noninvasive vascular laboratory, and in about 5% of patients with coronary disease requiring coronary bypass surgery.1,2 A blood pressure differential of greater than 15 mmHg is a strong predictor for the presence of significant subclavian stenosis.2,3
Treatment options for symptomatic patients include endovascular therapy with balloon-expandable stents or surgical treatment.1,4 Endovascular therapy is the preferred method for patients with patent but stenotic subclavian arteries; the procedural success rate approaches 100%, and the long-term patency rate is greater than 90%.4 Balloon-expandable stents are most commonly used. Technically, these are often approached from femoral access but brachial approaches may also be employed, particularly if there is significant tortuosity of the proximal subclavian or aorta. Complications include stroke (1%), distal embolization, and access site hematoma. It is important to delineate the origin and status of the left vertebral artery when considering endovascular therapy. Stenting of lesions adjacent to the left vertebral artery may result in closure or compromise of this important vessel and may result in devastating consequences if the right vertebral is diminutive or closed. Chronically occluded vessels have a much lower procedural success rate (approximately 50%), a higher acute complication rate and, if successful, a higher restenosis rate than for nonoccluded arteries. A variety of surgical methods may be employed including carotid-subclavian bypass using a synthetic graft or transposition of the sublavian to the common carotid.1,4 These techniques are also highly effective and are usually performed for symptomatic, chronically occluded subclavian arteries and for lesions at high risk for endovascular repair.
1 Mahmud E., Cavendish J.J., Salami A. Current treatment of peripheral arterial disease. Role of percutaneous interventional therapies. J Am Coll Cardiol. 2007;50:473-490.
2 Shadman R., Criqui M.H., Bundens W.P., Fronek A., Denenberg J.O., Gamst A.C., McDermott M.M. Subclavian artery stenosis: prevalence, risk factors, and association with cardiovascular disease. J Am Coll Cardiol. 2004;44:618-623.
3 Osborn L.A., Vernon S.M., Reynolds B., Timm T.C., Allen K. Screening for subclavian artery stenosis in patients who are candidates for coronary bypass surgery. Catheter Cardiovasc Interv. 2002;56:162-165.
4 Brountzos E.N., Malagari K., Kelekis D.A. Endovascular treatment of occlusive lesions of the subclavian and innominate arteries. Cardiovasc Interv Radiol. 2006;29:503-510.