Procedure 53 Metacarpophalangeal and Proximal Interphalangeal Joint Collateral Ligament Avulsion Fractures
![]() See Video 39: Metacarpal Shaft Fractures
See Video 39: Metacarpal Shaft Fractures
Indications
 Displaced collateral ligament with or without associated joint subluxation or dislocation
Displaced collateral ligament with or without associated joint subluxation or dislocation
 Large avulsion fragment with articular incongruity
Large avulsion fragment with articular incongruity
 Displaced and interposed fracture fragment within joint
Displaced and interposed fracture fragment within joint
 Border digit injury such as radial border of index finger or ulnar collateral ligament of thumb metaphalangeal (MP) joint
Border digit injury such as radial border of index finger or ulnar collateral ligament of thumb metaphalangeal (MP) joint
Examination/Imaging
Clinical Examination
 Unilateral swelling and bruising of the injured joint
Unilateral swelling and bruising of the injured joint
 Lateral deviation deformity of digit due to loss of collateral ligament integrity (Fig. 53-1)
Lateral deviation deformity of digit due to loss of collateral ligament integrity (Fig. 53-1)
 Pain with restricted range of motion
Pain with restricted range of motion
 Gentle testing of collateral ligaments to ensure integrity, which may require local anesthetic block. Avoid excessive force to prevent displacement of fragment (Fig. 53-2)
Gentle testing of collateral ligaments to ensure integrity, which may require local anesthetic block. Avoid excessive force to prevent displacement of fragment (Fig. 53-2)
 Patient asked to flex and extend the uninjured joints distal to the injury to evaluate the continuity of the flexor and extensor tendons
Patient asked to flex and extend the uninjured joints distal to the injury to evaluate the continuity of the flexor and extensor tendons
Imaging
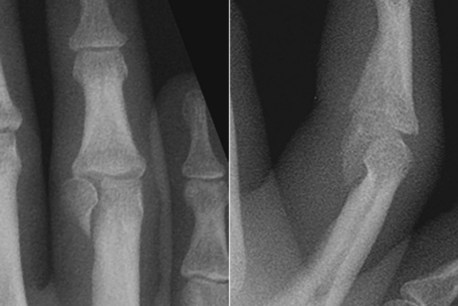
 Posteroanterior, oblique, and true lateral films of the digit for proximal interphalangeal (PIP) joint injuries. At the PIP joint, the most common avulsion fracture is a unicondylar fracture (Fig. 53-3).
Posteroanterior, oblique, and true lateral films of the digit for proximal interphalangeal (PIP) joint injuries. At the PIP joint, the most common avulsion fracture is a unicondylar fracture (Fig. 53-3).
 Posteroanterior, oblique, and true lateral films of the hand for metacarpophalangeal (MCP) joint injuries (Fig. 53-4).
Posteroanterior, oblique, and true lateral films of the hand for metacarpophalangeal (MCP) joint injuries (Fig. 53-4).
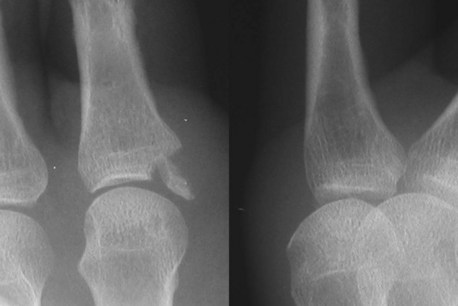
 In the immature skeleton, ligament avulsion injuries occur at the growth plate with a fragment of the epiphysis (Fig. 53-5).
In the immature skeleton, ligament avulsion injuries occur at the growth plate with a fragment of the epiphysis (Fig. 53-5).
 Brewerton view provides a tangential view of the metacarpal head, demonstrating the area of origin of the collateral ligament, which will help to reveal small avulsion fragments from the metacarpal head.
Brewerton view provides a tangential view of the metacarpal head, demonstrating the area of origin of the collateral ligament, which will help to reveal small avulsion fragments from the metacarpal head.
 Computed tomography scanning is useful in cases of suspected involvement of the articular surface for evaluation of joint congruity.
Computed tomography scanning is useful in cases of suspected involvement of the articular surface for evaluation of joint congruity.
Surgical Anatomy
 MCP joint collateral ligaments are more commonly avulsed at their distal insertion. An avulsed fragment from the base of the proximal phalanx is lateral and volar to the midaxis.
MCP joint collateral ligaments are more commonly avulsed at their distal insertion. An avulsed fragment from the base of the proximal phalanx is lateral and volar to the midaxis.
 Rarely, in more severe injuries, with pure ligamentous avulsions or smaller fragment avulsions, the avulsed ligament lies superficial to the extensor apparatus.
Rarely, in more severe injuries, with pure ligamentous avulsions or smaller fragment avulsions, the avulsed ligament lies superficial to the extensor apparatus.
 If avulsed without bone or with a small fragment, the ulnar collateral ligament of the thumb MP joint can come to lie superficial to the adductor aponeurosis (Stener lesion).
If avulsed without bone or with a small fragment, the ulnar collateral ligament of the thumb MP joint can come to lie superficial to the adductor aponeurosis (Stener lesion).
Positioning
Exposures
Metacarpophalangeal Joint
 The MCP joint of the thumb and borders of the hand (ulnar side of small and radial side of index finger) can be easily accessed through a lateral approach.
The MCP joint of the thumb and borders of the hand (ulnar side of small and radial side of index finger) can be easily accessed through a lateral approach.
 Cutaneous nerves are located in the subcutaneous plane and must be identified and preserved.
Cutaneous nerves are located in the subcutaneous plane and must be identified and preserved.
 The oblique fibers of the extensor hood cover the MCP joint and will need to be incised longitudinally for access to the joint; they require meticulous repair on completion.
The oblique fibers of the extensor hood cover the MCP joint and will need to be incised longitudinally for access to the joint; they require meticulous repair on completion.
 Access to the MP collateral avulsion fracture for nonborder digits is achieved by a volar approach that allows reduction and fixation with compression.
Access to the MP collateral avulsion fracture for nonborder digits is achieved by a volar approach that allows reduction and fixation with compression.
 With a volar approach, the digital neurovascular bundle is at risk for injury and must be identified and carefully retracted away from the flexor tendon sheath.
With a volar approach, the digital neurovascular bundle is at risk for injury and must be identified and carefully retracted away from the flexor tendon sheath.
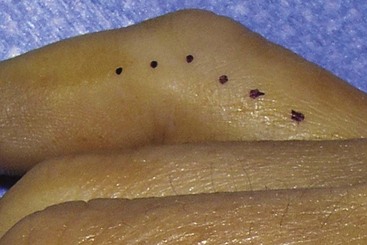
 A Bruner zigzag skin incision is made centered over the proximal digital crease (Fig. 53-6).
A Bruner zigzag skin incision is made centered over the proximal digital crease (Fig. 53-6).
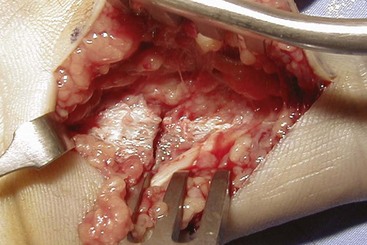
 The flexor sheath is kept intact (Fig. 53-7) and retracted subperiosteally off the base of the proximal phalanx and retracted (Fig. 53-8). After fracture fixation, the sheath is allowed to return to its normal position, and no repair is necessary.
The flexor sheath is kept intact (Fig. 53-7) and retracted subperiosteally off the base of the proximal phalanx and retracted (Fig. 53-8). After fracture fixation, the sheath is allowed to return to its normal position, and no repair is necessary.
Proximal Interphalangeal Joint
 At the PIP level, the fracture is approached using a midaxial incision.
At the PIP level, the fracture is approached using a midaxial incision.
 A digital midaxial incision is marked by joining the most dorsal points of the digital creases with the digit in full flexion (Fig. 53-9).
A digital midaxial incision is marked by joining the most dorsal points of the digital creases with the digit in full flexion (Fig. 53-9).
 The transverse fibers of the extensor apparatus at the level of the PIP are released to elevate the lateral band of the extensor mechanism dorsally.
The transverse fibers of the extensor apparatus at the level of the PIP are released to elevate the lateral band of the extensor mechanism dorsally.
Pearls
The midaxial skin incision is dorsal to the midlateral line and avoids dissection of the digital neurovascular bundle.
Careful spreading dissection is necessary after skin incision to preserve the subcutaneous nerves.
When exposing the fragments, care must be taken to avoid stripping excessive soft tissue and devascularizing the fragment.
Procedure
Step 1: Principles and Methods of Fixation
 Type of fixation depends on size of fragment and comminution.
Type of fixation depends on size of fragment and comminution.
 A single large fragment can be treated with lag screws. If possible, two screws should be employed for rotational stability.
A single large fragment can be treated with lag screws. If possible, two screws should be employed for rotational stability.
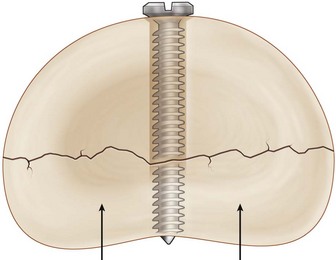
 Lag or compression screw implies a screw that does not have any purchase on the near fragment. This is achieved by drilling a glide hole that exceeds the screw thread diameter in the near cortex. The far cortex is then drilled with the thread hole that matches the screw shaft diameter. As the screw is inserted, it slides through the near cortex and gains purchase in the far cortex. With further tightening, compression between the fragments is generated (Fig. 53-10).
Lag or compression screw implies a screw that does not have any purchase on the near fragment. This is achieved by drilling a glide hole that exceeds the screw thread diameter in the near cortex. The far cortex is then drilled with the thread hole that matches the screw shaft diameter. As the screw is inserted, it slides through the near cortex and gains purchase in the far cortex. With further tightening, compression between the fragments is generated (Fig. 53-10).
 If screws are not available or lag screw fixation is not possible, tension band fixation of the fragment can be performed. Malleable wire is passed through the collateral ligament close to its bony insertion and passed through a drill hole in the metaphysis in a figure-of-eight loop. The fragment is then reduced, a K-wire is passed through the fragment for longitudinal stability, and the wire loop is tightened to compress the fracture.
If screws are not available or lag screw fixation is not possible, tension band fixation of the fragment can be performed. Malleable wire is passed through the collateral ligament close to its bony insertion and passed through a drill hole in the metaphysis in a figure-of-eight loop. The fragment is then reduced, a K-wire is passed through the fragment for longitudinal stability, and the wire loop is tightened to compress the fracture.
 If the fracture fragments are too small for fixation, they may be excised, and direct repair of the ligament to bone is performed using an anchor or pull-through sutures.
If the fracture fragments are too small for fixation, they may be excised, and direct repair of the ligament to bone is performed using an anchor or pull-through sutures.
Step 1 Pearls
Step 2
 The avulsed fragment is carefully handled to maintain the attached collateral ligament.
The avulsed fragment is carefully handled to maintain the attached collateral ligament.
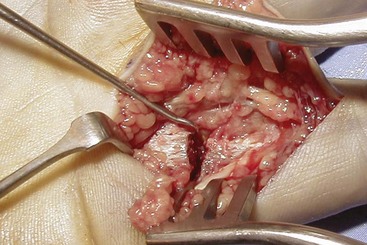
 The fragment must be carefully retracted with a hook, and the joint is subluxated to look for any loose cartilaginous fragments or impaction of the joint surface (Fig. 53-12).
The fragment must be carefully retracted with a hook, and the joint is subluxated to look for any loose cartilaginous fragments or impaction of the joint surface (Fig. 53-12).
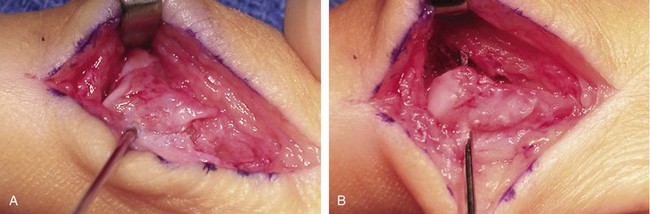
 A 0.035-inch K-wire inserted into the fragment may be used as a joystick to gently manipulate the piece as needed (Fig. 53-13A).
A 0.035-inch K-wire inserted into the fragment may be used as a joystick to gently manipulate the piece as needed (Fig. 53-13A).
 After reduction, the same wire is advanced distally for temporary fixation (Fig. 53-13B).
After reduction, the same wire is advanced distally for temporary fixation (Fig. 53-13B).
 The reduction is then checked by imaging.
The reduction is then checked by imaging.
 Definitive fixation is then performed. If screw fixation is planned, the appropriate-sized glide hole is drilled through the fragment. The thread hole is then drilled through the far cortex. The screw length is determined, and an appropriate screw is inserted.
Definitive fixation is then performed. If screw fixation is planned, the appropriate-sized glide hole is drilled through the fragment. The thread hole is then drilled through the far cortex. The screw length is determined, and an appropriate screw is inserted.
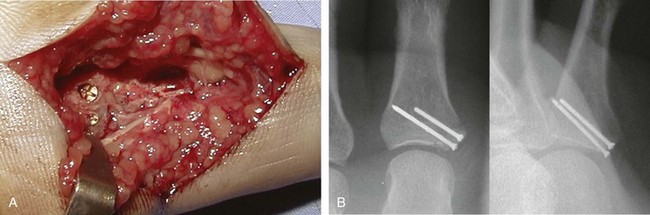
 The K-wire is then removed, and the second screw is inserted through the K-wire hole, after overdrilling the near cortex (Fig. 53-14).
The K-wire is then removed, and the second screw is inserted through the K-wire hole, after overdrilling the near cortex (Fig. 53-14).
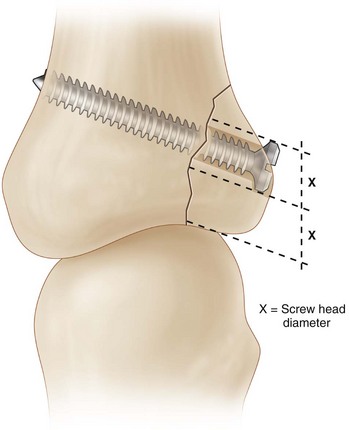
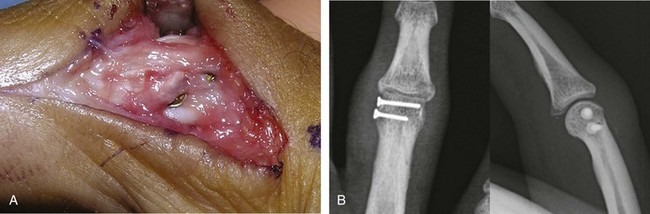
 At the PIP joint, the screw head may interfere with gliding of the near collateral ligament. This can be avoided by placing one screw at or just proximal to the ligament origin. The second screw is placed between the main and accessory parts of the ligament and tightened until it sinks beneath the ligament complex (Fig. 53-15).
At the PIP joint, the screw head may interfere with gliding of the near collateral ligament. This can be avoided by placing one screw at or just proximal to the ligament origin. The second screw is placed between the main and accessory parts of the ligament and tightened until it sinks beneath the ligament complex (Fig. 53-15).
Step 2 Pitfalls
The screw may accidentally penetrate the articular surface.
Placement of a long screw may cause irritation of the extensor mechanism at the base of the proximal phalanx.
A long screw at the head of the proximal phalanx may impinge on the collateral ligament at the far end of the joint and lead to joint stiffness.
Step 3
 Screw length and position are checked by intraoperative imaging.
Screw length and position are checked by intraoperative imaging.
 At the MCP joint, the flexor tendons with surrounding sheath are replaced, and no suture is necessary.
At the MCP joint, the flexor tendons with surrounding sheath are replaced, and no suture is necessary.
 At the PIP joint, the extensor mechanism is then repaired with a continuous nonabsorbable suture.
At the PIP joint, the extensor mechanism is then repaired with a continuous nonabsorbable suture.
Postoperative Care and Expected Outcomes
 The hand is rested in a plaster splint for the first 5 to 7 days after surgery.
The hand is rested in a plaster splint for the first 5 to 7 days after surgery.
 The hand is placed in a removable splint, and active motion is commenced by the end of the first week after surgery. The ligament repair is protected by buddy taping to the digit adjacent to the injured ligament.
The hand is placed in a removable splint, and active motion is commenced by the end of the first week after surgery. The ligament repair is protected by buddy taping to the digit adjacent to the injured ligament.
 Splinting is discontinued by 4 to 6 weeks when tenderness and swelling have subsided.
Splinting is discontinued by 4 to 6 weeks when tenderness and swelling have subsided.
 Strengthening is commenced after full range of motion has returned.
Strengthening is commenced after full range of motion has returned.
 Most patients with PIP joint injuries can expect residual swelling and flexion contracture that is usually mild.
Most patients with PIP joint injuries can expect residual swelling and flexion contracture that is usually mild.
 MCP joint injuries have a better prognosis, and patients usually can regain full motion. Swelling around the joint is less noticeable than in the finger.
MCP joint injuries have a better prognosis, and patients usually can regain full motion. Swelling around the joint is less noticeable than in the finger.
Bischoff R, Buechler U, De Roche R, Jupiter J. Clinical results of tension band fixation of avulsion fractures in the hand. J Hand Surg [Am]. 1994;19:1019-1026.
Kozin SH, Bishop AT. Tension wire fixation of avulsion fractures at the thumb metacarpophalangeal joint. J Hand Surg [Am]. 1994;19:1027-1031.
Schubiner JM, Mass DP. Operation for collateral ligament ruptures of the metacarpophalangeal joints of the fingers. J Bone Joint Surg [Br]. 1989;71:388-389.
Shewring DJ, Thomas RH. Avulsion fractures from the base of the proximal phalanges of the fingers. J Hand Surg [Br]. 2003;28:10-14.
Shewring DJ, Thomas RH. Collateral ligament avulsion fractures from the heads of the metacarpals of the fingers. J Hand Surg [Br]. 2006;31:537-541.