CHAPTER 53
Hip Adductor Strain
Definition
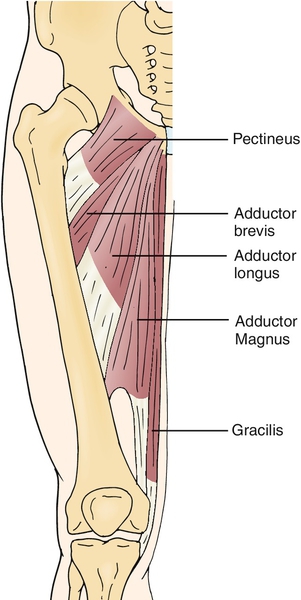
Hip adductor strain refers to an injury of the hip adductor muscles at the muscle belly, myotendinous junction, or tendon. It can be an acute or chronic injury. The hip adductor muscles include the adductor magnus, adductor brevis, adductor longus, pectineus, and gracilis muscles (Fig. 53.1). All of these muscles are innervated by the obturator nerve with the exception of the pectineus muscle, which is innervated by the femoral nerve. Their functions include hip adduction and hip flexion. Adductor strain is the most common cause of acute groin pain in athletes [1]. The adductor longus myotendinous junction is the most commonly injured site [2].
A prospective cohort study of the incidence of groin injuries during a 1-year period among Swedish male club soccer players reported that 8% of all injuries were in the groin area, and 52% of these were attributed to adductor muscle or tendon injuries [3]. A similar incidence was reported in a study of Norwegian female elite soccer players, in which 9% of all injuries were hip or groin strains; 83% of these were acute injuries and 17% were secondary to overuse [4]. For male ice hockey players of a single National Hockey League team, Tyler and colleagues [5] reported 3.2 strains per 1000 player-game exposures. Orchard and Seward [6] monitored all the injuries that occurred in the Australian Football League during 4 consecutive years. In total, more than 660 elite male athletes played 22 matches per season among 16 teams. There was an incidence of 3.3 groin strains per team per season, the second most common musculoskeletal injury after hamstring strain, and a recurrence rate of 21%. In addition, it was the third most prevalent injury after hamstring strain and anterior cruciate ligament tear, with 11.9 matches missed per team per season. A retrospective cohort study of 500 Australian Football League players indicated that 17% sustained a hip or groin injury during their junior years. Of these, 31% were secondary to a hip adductor strain or tear, and 17% were recurrent injuries [7]. Recurrence of hip adductor strains has been reported to be as high as 32% to 44% in ice hockey and Australian football athletes [5,8]. Adductor strains in elderly athletes older than 70 years occur at a slightly decreased incidence of 5% [9]. The incidence and prevalence of hip adductor strains in sedentary patients are unknown.
Athletes who participate in sports that require cutting and sudden change of direction (e.g., soccer, ice hockey, Australian-rules football) are at increased risk for this injury [10]. Adductor strains may also occur from an eccentric contraction of the adductor muscles opposing the abductor muscles, as may be seen with an explosive lateral propulsion in ice hockey [11]. Hip adductor strains have been attributed to low strength or flexibility of this muscle group [12]. There is usually poor conditioning of the trunk and lower extremities characterized by muscle imbalance among the pelvic stabilizing muscles, including the hip abductor and adductor muscles, as well as the core muscles and hip flexors [10]. In addition, poor technique and overuse are risk factors for adductor strains. In rare instances, sacroiliac dysfunction may be associated with adductor injuries [13].
Adductor strains may be classified according to functional limitation on physical examination or pathologic injury on radiographic imaging (Table 53.1). The functional classification may or may not directly correlate with the pathologic change of the tissue seen on radiographic imaging. If the injury is localized at the tendon or myotendinous junction, it may also be described as an adductor tendinitis, referring to an acute injury with active inflammatory process, or as an adductor tendinosis, referring to a chronic injury that is causing functional limitations and does not have an ongoing inflammatory reaction. Because it may be difficult to classify the presence of an inflammatory process, tendinopathy is used frequently to refer to an adductor tendon or myotendinous injury with partial or complete loss of function that may be acute or chronic.
Table 53.1
Functional and Radiographic Classifications
| Grade | Functional Classification | Radiographic Classification |
| 1 | No loss or minimal loss of function or mobility | Inflammation at the injured site with no tear |
| 2 | Partial loss of strength and mobility | Partial tear of the adductor muscle or tendon |
| 3 | Complete loss of function | Full tear of the adductor muscle or tendon |
Symptoms
Patients with hip adductor strains complain of sharp, stinging, or aching pain in the groin area that may radiate down to the anteromedial thigh. Symptoms are worse when they adduct and flex the leg at the hip, such as when they move the outside leg into a car. They usually report tightness in the groin or anteromedial pelvic girdle region. In injuries involving a partial or complete tear of the muscle or tendon, they complain of soft tissue swelling and bruising in the medial thigh. Chronic injuries may hurt only during physical activity or sports participation.
Physical Examination
The patient presents with tenderness to palpation in the groin region, most commonly over the adductor longus tendon or myotendinous junction distal to the origin of the muscle at the anterior surface of the pubis between the crest and the symphysis. In severe injuries, a defect may be palpated in the muscle representing a tear in the muscle or tendon. There can be associated ecchymosis, swelling, and tenderness of the surrounding soft tissue. Antalgic gait may be noted with ambulation secondary to pain or dysfunction. Single-leg standing and squatting may reveal Trendelenburg sign, excessive hip internal or external rotation, or genu valgus or varus.
Pain or weakness of the hip adductor muscle may be elicited with active resisted hip adduction, hip adduction and flexion, and hip flexion. Groin pain may also be reproduced with passive forced hip abduction as well as with passive flexion, abduction, and external rotation of the hip (FABER test). The cross-over sign may be used to determine if the adductor strain is moderate to severe and likely to cause functional impairment. This maneuver consists of reproducing the typical groin pain while performing any of the provocative maneuvers mentioned before on the contralateral side (i.e., FABER test, active resisted hip adduction, or passive hip abduction). The squeeze test and the static resisted hip adduction test are specific examinations for hip adductor muscles. During the squeeze test, the patient is in the supine position with feet on the table, hips flexed to 45 degrees, and knees flexed to 90 degrees. The examiner places the fist between the knees and asks the patient to squeeze the fist by adducting the hips bilaterally. The resisted hip adduction test consists of laying the patient supine with legs straight, positioning each leg at 15 degrees of abduction, and bilaterally resisting active hip adduction.
Functional Limitations
Patients usually have difficulty with walking, running, doing pivot turns, going up and down stairs, and standing up from a sitting position and vice versa. As mentioned before, getting in and out of a car is particularly painful. Sexual intimacy is frequently avoided because of the proximity of the injury to the sexual organs and groin pain experienced as the adductor muscles contract to stabilize the pelvis.
Hip adductor strains present with significant functional limitations during sports participation and interfere with athletes’ optimal performance. They may report difficulty with propulsion in the lateral direction due to the eccentric contraction of the hip adductor muscles attempting to decelerate the leg stride, tightness in the groin region despite stretching, and loss of maximal sprinting speed, among other complaints [10,14]. The biomechanics of movements involving the hip joint are consequently altered as the athlete tries to avoid experiencing pain. If it is left uncorrected, this adaptation eventually leads to other injuries, such as contralateral hip adductor strain, osteitis pubis, and sports hernia.
Diagnostic Studies
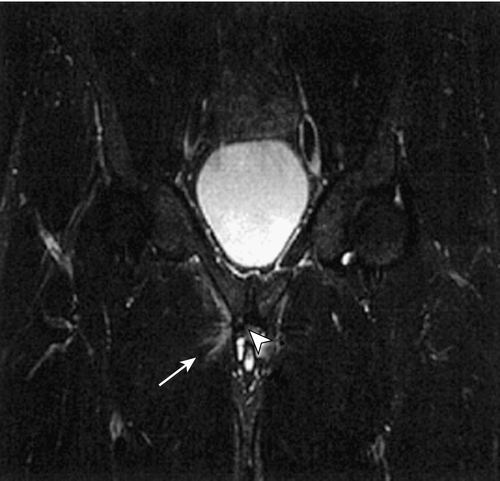
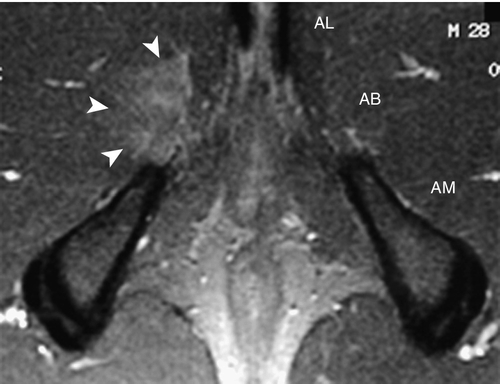
Initial evaluation of groin pain should include plain films to rule out bone disease, such as hip osteoarthritis and neoplasm. Avulsion injuries of the symphysis pubis and inferior pubic ramus may also occur from chronic overuse and be manifested with adductor enthesopathy and osteitis pubis [15]. Magnetic resonance imaging is the optimal imaging tool to evaluate for groin and hip disease because it provides visualization of a large field and gives a three-dimensional view of the region with excellent soft tissue contrast resolution [16]. It is particularly effective for diagnosis of adductor muscle and tendon disease. Fat-saturated, fluid-sensitive magnetic resonance sequences in the axial-oblique and coronal planes are best for evaluating hip adductor strains [17] (Figs. 53.2 and 53.3). Magnetic resonance imaging also helps differentiate hip adductor injuries from other pelvic disease, such as acetabular labrum tears and osteitis pubis.
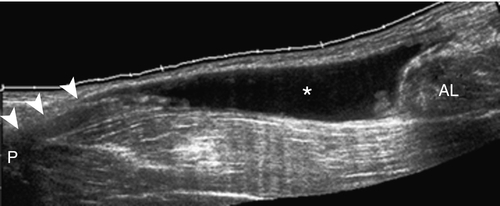
Ultrasound can be used to evaluate the adductor muscles under dynamic conditions, to compare the asymptomatic side, and specifically to image the area of maximal tenderness to detect tissue injury such as a partial or full tear [18] (Fig. 53.4). Ultrasound imaging can be as sensitive as magnetic resonance imaging in the acute setting; however, it has limited visualization in patients with large thighs and is less useful when prognostic indicators are required [19,20].
Treatment
Initial
Hip adductor strains are managed initially with rest, ice, compression, elevation, and nonsteroidal anti-inflammatory drugs (NSAIDs) to decrease swelling and inflammation. Athletes with acute hip adductor strains are requested to stop competitive participation and training to avoid further injury. The initial treatment (first phase of rehabilitation) should focus on tissue protection using an elastic wrap or compression shorts, reducing the local inflammation with cryotherapy and NSAIDs, and minimizing excessive motion of the injured site as well as weight bearing as tolerated with crutches. This is especially important in the presence of an apophyseal injury or tendon tear. Other causes of groin pain should be ruled out (see differential diagnosis) before a comprehensive rehabilitation program is implemented.
Rehabilitation
When the acute inflammatory phase subsides, usually within 48 hours, the second phase of rehabilitation is started to facilitate tissue healing and proper collagen deposition. Any increased muscle tone guarding the injured site should be addressed with various therapeutic modalities, including soft tissue massage and gentle passive range of motion. The appropriate time to commence stretching is debated. Some experts suggest that stretching should be done early to promote proper lengthening of the injured tissue as it remodels. Others suggest that early stretching may expose the athlete to development of chronic tendinopathy and should not start until at least 4 days after the injury [14].
A gradual muscle strengthening program is implemented, initially focusing on gentle active range of motion of the hip and strengthening of adjacent regions including core stabilization exercises. After full pain-free passive range of motion is achieved, exercises specifically focusing on hip adductor strengthening are initiated, starting with static exercises and progressing to concentric exercises. Neuromuscular electrical stimulation may be used to assist proper muscle activation. Once the patient is pain free with concentric exercises, on average 2 to 4 weeks after the initial injury, eccentric exercises are started for strengthening of the injured site. In an example of a hip adductor eccentric exercise, the patient lies supine, places the feet together against a wall with knees at full extension and hips at 60 degrees of flexion, and then slowly opens the legs symmetrically into hip abduction. If pain is experienced during any of the stages of the gradual strengthening program, the specific painful activity should be modified or stopped until the exercises can be completed pain free.
The third phase of the rehabilitation program involving functional training can be implemented once strength and flexibility are recovered. Proprioceptive training and plyometric exercises on unbalanced surfaces are done to continue strengthening of the hip adductor muscles and to reeducate proper neuromuscular activation of the various pelvic stabilizing agonist and antagonist muscles. In addition, dynamic strengthening exercises that incorporate the entire body are started (e.g., cable cross-over pull while standing on unstable surface).
At some point between the second and third phase of rehabilitation, the patient may start doing straight-line aerobic exercises, such as jogging or cycling, as long as muscle guarding is eliminated, there is no cross-over sign, and there is no pain experienced with the strengthening program. Distance, intensity, and time should be gradually increased as tolerated, ensuring that the athlete does not experience pain during or after the activity. Once the athlete tolerates straight-line running exercises at more than 75% of maximum performance, drills involving lateral movements and change of directions can be implemented. The last stage of functional training focuses on sports-specific exercises and drills that simulate actual playing.
The ultimate objective of the rehabilitation protocol is to improve the pelvic stability by balancing the strength between the opposing pelvic stabilizing muscles and, in the case of athletes, gradually return them to peak performance. Specifically, hip adductor muscles should have at least 80% of the strength of the ipsilateral hip abductor muscles before return to play [21]. The length of the rehabilitation program varies according to the severity of the injury and the athlete’s demand on the pelvic stabilizing muscles for participation in his or her sport. Severe injuries may take up to 12 weeks for full recovery and return to play.
Procedures
Patients may have trigger points along the muscle belly of one or more of the adductor muscles. These may be managed by trigger point injections with a local anesthetic such as lidocaine. In chronic cases in which pain is severely interfering with the rehabilitation program, a corticosteroid injection under ultrasound guidance may be placed in the peritendinous area, avoiding direct injection into the adductor tendon. This will decrease any residual inflammatory reaction, reduce pain, and facilitate the athlete’s completion of the rehabilitation protocol. In cases that have been recalcitrant to conservative measures, the patient may benefit from needling the tendon under ultrasound guidance to reactivate the tissue healing cascade [22]. A regenerative injectate such as platelet-rich plasma may be used; nonetheless, there is limited evidence of the benefits with use of these injectates [23,24]. Extracorporeal shock wave therapy may also be considered for recalcitrant cases [25].
Surgery
Referral to a sports medicine orthopedic surgeon should be considered with a significant avulsion fracture, complete adductor tendon tear, or chronic recalcitrant cases that failed the rehabilitation program. Depending on the chronicity of the injury, the patient may benefit from a partial or complete adductor tendon release. Most athletes who undergo adductor longus tenotomy return to competitive sports within 3 months [26].
Potential Disease Complications
Early diagnosis and treatment usually lead to successful outcomes and complete recovery. Continued activity or sports participation without proper rehabilitation frequently causes worsening pain, weakness, and functional limitations. Signs of mild hip adductor strains include recurrent tightness during or after activity with no relief from stretching and a decrease in sports-specific performance. Mild injuries may become severe if they are not treated accordingly. In addition, the injured adductor muscle will cause pelvic instability and may lead to further injury of the suprapubic muscles or the contralateral hip adductor muscles.
Potential Treatment Complications
Early return to play may lead to recurrent hip adductor strains [27]. Management of a hip adductor strain with only rest or NSAIDs will provide symptom relief but will not address the original cause of the injury, which in most cases is attributed to poor conditioning and imbalance of the pelvic stabilizing muscles. Athletes who complete an active training program are more likely to have excellent outcomes and pain-free successful return to sports in the first 6 months as well as to maintain significant improvement in symptoms up to 12 years after the injury compared with athletes who undergo a physiotherapy program without an active strengthening program [28,29]. Inadequate rehabilitation may lead to chronic injury, especially if there is concomitant pelvic dysfunction that is left untreated.
One of the most frequently used treatments for the pain associated with tendinopathies is prescription-strength anti-inflammatory drugs such as NSAIDs, selective cyclooxygenase 2 inhibitors, and corticosteroid injections. However, these treatment options carry potential risks for complications. A study of the effect of ibuprofen over rat Achilles tendon cells showed increased activity of the collagen-degrading enzymes, suggesting a detrimental effect of ibuprofen on the mechanism for tendon healing [30]. In vitro and in vivo experiments showed that NS-398, a specific cyclooxygenase 2 inhibitor, inhibited the proliferation and maturation of differentiated myogenic precursor cells, suggesting a detrimental effect on skeletal muscle healing [31]. Studies of corticosteroid injections for lateral epicondylitis show positive short-term results but frequent relapses and no significant difference from placebo or physiotherapy in the long term [32,33]. In addition, corticosteroid injections have resulted in tendon rupture in several cases of Achilles tendinopathy [34]. Surgery also carries significant risks. In addition to the risk of infection or nerve injury seen with most surgeries, adductor longus tenotomy may leave patients with decreased hip adduction strength [26]. Patients should be educated on the corresponding risks versus benefits of the chosen treatment plan.
Acknowledgment
The author thanks Michael T. Ellerbusch, MD, for his contribution to this chapter.







