CASE 53

History: A 39-year-old man presents with 2-year history of intermittent bloody diarrhea.
1. Which of the following should be included in the differential diagnosis of the imaging findings shown in the figures? (Choose all that apply.)
A. Familial adenomatous polyposis
2. Noting the general appearance of the colon in figure A, what disease has this patient suffered from previously?
3. What is the most common acute complication of severe acute ulcerative colitis?
4. Patients with chronic ulcerative colitis undergo imaging or colonoscopic surveillance. What complication of chronic disease is being screened for?
ANSWERS
CASE 53
Chronic Ulcerative Colitis
1. A, C, D, and E
2. D
3. C
4. B
References
Roggeveen MJ, Tismenetsky M, Shapiro R. Ulcerative colitis. Radiographics. 2006;26:947–951.
Zegal HG, Laufer I. Filiform polyposis. Radiology. 1978;127:615–619.
Cross-Reference
Gastrointestinal Imaging: THE REQUISITES, 3rd ed, p 287.
Comment
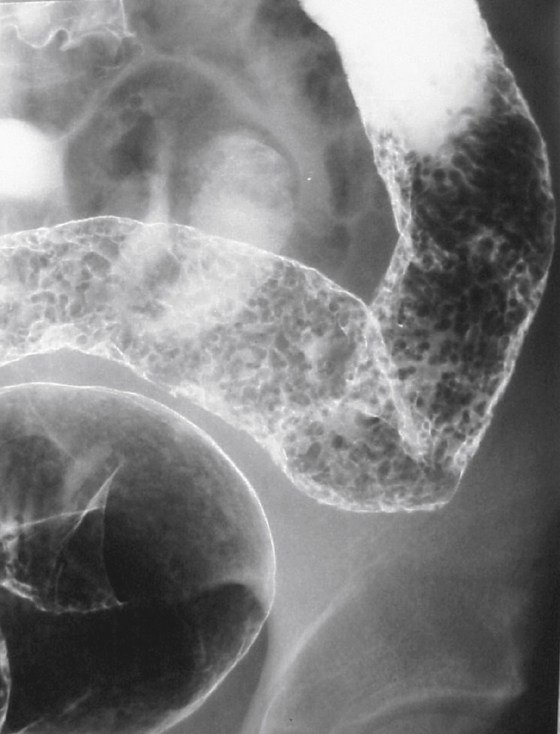
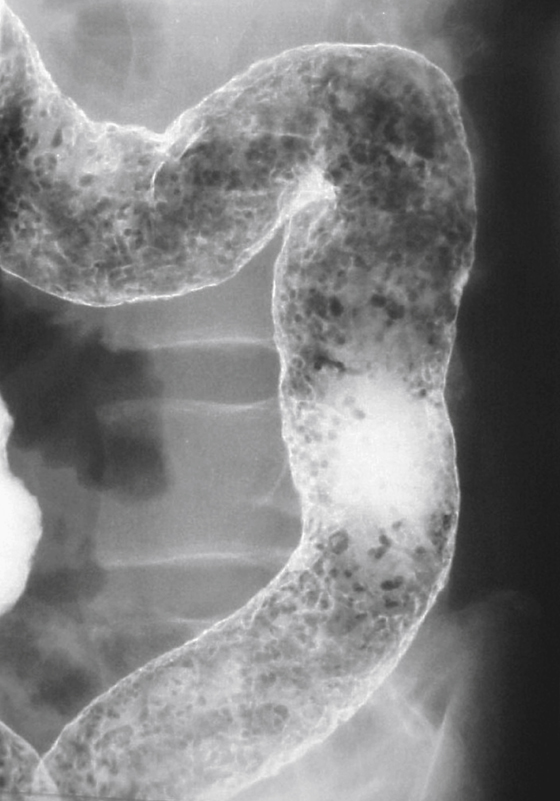
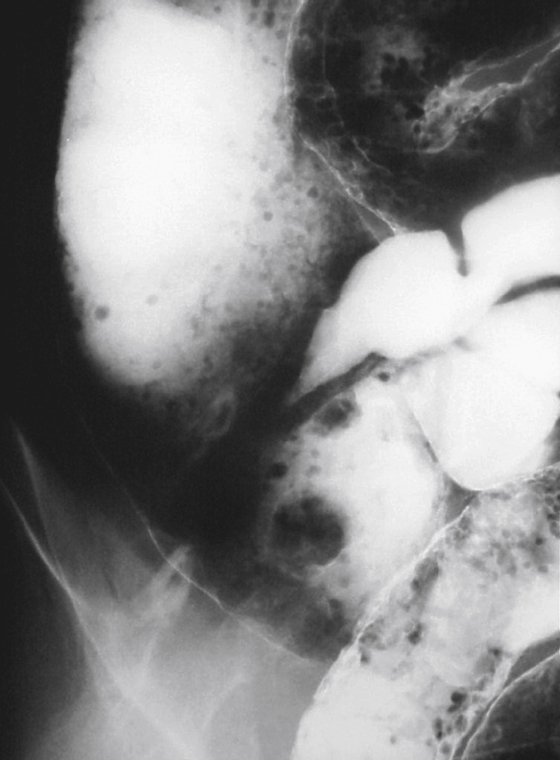
Chronic or “burned out” ulcerative colitis can leave behind sequelae, such as the postinflammatory polyposis seen in this case (see figures). These defects are also known as filiform polyposis of the colon. In reality, they are not true polyps or even hyperplastic polyps (although a tiny number may be hyperplastic). They are, instead, mucosal tags, which have been left behind following the healing process. In the acute phase of severe ulcerative colitis there is marked ulcerative denouement of the colonic mucosal surface by the widespread ulcerative process. Not all the mucosa is ulcerated, and small islands of residual edematous mucosa remain (pseudopolyps). In the healing process, the colonic surface re-epithelializes. The small islands of residual mucosa that have survived the inflammatory process are re-epithelialized up to the base of the residual mucosal tags and in some cases beneath the tags, leaving them dangling in the bowel lumen and giving us the picture of filiform or postinflammatory polyposis. Although patients with ulcerative colitis who have suffered pancolitis continuously over 10 years have a 10% chance of malignancy, patients who have had limited involvement and healing will have a much lesser, but still increased risk. The patient shown has had pancolitis. Note the normal appearance of the terminal ileum (see figures).







