Procedure 52 Hemi-Hamate Arthroplasty
Figures 52-1, 52-5, 52-7, and 52-8 through 52-11 borrowed with permission from Williams RMM, Kiefhaber TR, Sommerkamp TG, et al. Proximal interphalangeal fracture/dislocations using a hemi-hamate autograft. J Hand Surg [Am]. 2003;28:856-865.
Indications
 Unstable PIP joint fracture dislocations in which more than 50% of the palmar base of the middle phalanx is fractured. There must be dorsal cortical continuity.
Unstable PIP joint fracture dislocations in which more than 50% of the palmar base of the middle phalanx is fractured. There must be dorsal cortical continuity.
 Comminuted lateral plateau fractures of the base of the middle phalanx.
Comminuted lateral plateau fractures of the base of the middle phalanx.
 Joint salvage after failed treatment of complex fracture-dislocations of the PIP joint.
Joint salvage after failed treatment of complex fracture-dislocations of the PIP joint.
Examination/Imaging
Clinical Examination
 Record active range of motion of the affected finger as tolerated.
Record active range of motion of the affected finger as tolerated.
 Evaluate coronal plane alignment, assessing for lateral deviation that suggests asymmetrical compression of the articular surface.
Evaluate coronal plane alignment, assessing for lateral deviation that suggests asymmetrical compression of the articular surface.
 Examine the sagittal alignment with the finger extended, looking for colinearity of the proximal phalanx and middle phalanx.
Examine the sagittal alignment with the finger extended, looking for colinearity of the proximal phalanx and middle phalanx.
Imaging
 Standard anteroposterior, oblique, and lateral views of the involved digit to assess the amount of articular involvement of the base of the middle phalanx, the integrity of the middle phalangeal dorsal cortex, and other fractures (Fig. 52-1).
Standard anteroposterior, oblique, and lateral views of the involved digit to assess the amount of articular involvement of the base of the middle phalanx, the integrity of the middle phalangeal dorsal cortex, and other fractures (Fig. 52-1).
 Computed tomography can better delineate the extent of articular cartilage involvement and comminution, but it is rarely necessary.
Computed tomography can better delineate the extent of articular cartilage involvement and comminution, but it is rarely necessary.
Surgical Anatomy
 The PIP joint is a complex hinge joint formed by the head of the proximal phalanx and the base of the middle phalanx that moves through a 110-degree arc of motion.
The PIP joint is a complex hinge joint formed by the head of the proximal phalanx and the base of the middle phalanx that moves through a 110-degree arc of motion.
 The volar plate originates from the proximal phalanx periosteum and inserts onto the volar lip of the middle phalanx.
The volar plate originates from the proximal phalanx periosteum and inserts onto the volar lip of the middle phalanx.
 Lateral joint stability is afforded by the thick collateral ligaments. The proper collateral ligament inserts onto the volar-lateral third of the middle phalanx, and the accessory collateral ligament inserts onto the volar plate.
Lateral joint stability is afforded by the thick collateral ligaments. The proper collateral ligament inserts onto the volar-lateral third of the middle phalanx, and the accessory collateral ligament inserts onto the volar plate.
 Dorsal translation of the middle phalanx is prevented by the volar plate and the cup-shaped articular surface of the middle phalanx, which congruously articulates with the proximal phalanx head.
Dorsal translation of the middle phalanx is prevented by the volar plate and the cup-shaped articular surface of the middle phalanx, which congruously articulates with the proximal phalanx head.
 Dorsal fracture-dislocations disrupt both of these restraints and result in dorsal subluxation of the middle phalanx.
Dorsal fracture-dislocations disrupt both of these restraints and result in dorsal subluxation of the middle phalanx.
 The stability of the PIP joint is directly related to the amount of middle phalangeal volar articular surface disrupted. Fractures with as little as 30% of the articular surface involved may be unstable.
The stability of the PIP joint is directly related to the amount of middle phalangeal volar articular surface disrupted. Fractures with as little as 30% of the articular surface involved may be unstable.
Exposures
 Exposure of the PIP joint is gained through a palmar V-shaped incision centered over the PIP joint (Fig. 52-2).
Exposure of the PIP joint is gained through a palmar V-shaped incision centered over the PIP joint (Fig. 52-2).
 The skin and subcutaneous tissue are sharply elevated, and both neurovascular bundles are visualized deep to the lateral digital sheet and protected.
The skin and subcutaneous tissue are sharply elevated, and both neurovascular bundles are visualized deep to the lateral digital sheet and protected.
 A rectangular flap of the fibro-osseous sheath that includes the entire A3 pulley is developed between the A2 and A4 pulleys.
A rectangular flap of the fibro-osseous sheath that includes the entire A3 pulley is developed between the A2 and A4 pulleys.
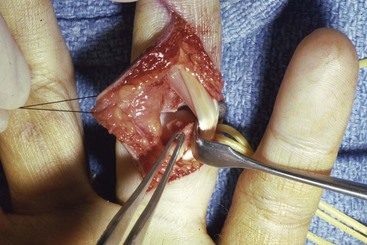
 The flexor tendons are retracted to expose the volar plate, which is released from the accessory collateral ligaments at its lateral margins (Fig. 52-3).
The flexor tendons are retracted to expose the volar plate, which is released from the accessory collateral ligaments at its lateral margins (Fig. 52-3).
 The volar plate is incised transversely from the base of the middle phalanx and reflected proximally (Fig. 52-4).
The volar plate is incised transversely from the base of the middle phalanx and reflected proximally (Fig. 52-4).
 Release the collateral ligaments from the head of the proximal phalanx, leaving a small stump attached to the middle phalanx to facilitate volar plate reattachment at the end of the procedure.
Release the collateral ligaments from the head of the proximal phalanx, leaving a small stump attached to the middle phalanx to facilitate volar plate reattachment at the end of the procedure.
Pearls
The V-shaped incision extends from the palmodigital crease to the DIP joint flexion crease, with the apex based either radially or ulnarly centered at the PIP joint.
The neurovascular bundles must be visualized, but it is not necessary to mobilize them; they remain protected deep to the lateral digital sheet.
Procedure
Step 1: Preparing the Articular Surface of the Middle Phalanx
 By means of a Penrose drain or moist umbilical tape, the flexor tendons are retracted radially or ulnarly. The PIP joint is hyperextended (“shotgunning”) to expose the fracture site. Loose fragments are débrided (Fig. 52-5).
By means of a Penrose drain or moist umbilical tape, the flexor tendons are retracted radially or ulnarly. The PIP joint is hyperextended (“shotgunning”) to expose the fracture site. Loose fragments are débrided (Fig. 52-5).
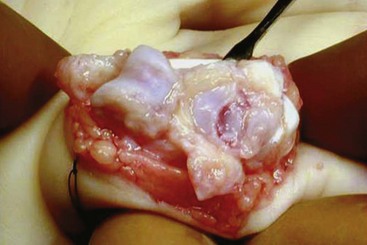
 After the fracture fragments from the articular surface of the middle phalanx are débrided, a 4-mm oscillating saw is used to create a boxlike recipient defect.
After the fracture fragments from the articular surface of the middle phalanx are débrided, a 4-mm oscillating saw is used to create a boxlike recipient defect.
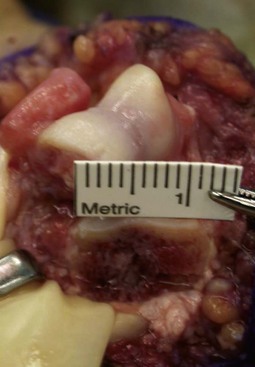
 Measure the bony defect, including the width of the articular surface, the dorsal-palmar height, and the proximal-distal length (Fig. 52-6).
Measure the bony defect, including the width of the articular surface, the dorsal-palmar height, and the proximal-distal length (Fig. 52-6).
Step 2: Harvesting the Hamate Osteochondral Graft
 Use fluoroscopy to locate the carpometacarpal (CMC) joint at the base of the ring and small finger. Then make a transverse 3-cm incision just proximal to the joint.
Use fluoroscopy to locate the carpometacarpal (CMC) joint at the base of the ring and small finger. Then make a transverse 3-cm incision just proximal to the joint.
 Bluntly mobilize the subcutaneous veins and nerves and retract the extensor tendons.
Bluntly mobilize the subcutaneous veins and nerves and retract the extensor tendons.
 Make a longitudinal capsulotomy to expose the ring and small CMC joint (Fig. 52-7).
Make a longitudinal capsulotomy to expose the ring and small CMC joint (Fig. 52-7).
 Use a fine-tipped marker to outline the donor graft dimension, using the distal articular surface as a reference point.
Use a fine-tipped marker to outline the donor graft dimension, using the distal articular surface as a reference point.
 Make the axial osteotomy (line A) and the sagittal osteotomies (lines B and C), using an osteotome or an oscillating saw just outside the marked line to ensure that the graft is large enough (Fig. 52-8).
Make the axial osteotomy (line A) and the sagittal osteotomies (lines B and C), using an osteotome or an oscillating saw just outside the marked line to ensure that the graft is large enough (Fig. 52-8).
 Make the coronal osteotomy using a curved osteotome, taking care to avoid damage to the articular surface of the ring and small fingers.
Make the coronal osteotomy using a curved osteotome, taking care to avoid damage to the articular surface of the ring and small fingers.
Step 2 Pearls
Protect the articular surface of the fourth and fifth metacarpals with a Freer elevator when making the osteotomy.
Err on the side of taking an osteochondral graft 1 to 2 mm larger than measured.
The coronal plane osteotomy using the curved osteotome can be facilitated by making an osseous trough in the hamate just proximal to the osteotomy site.
Step 2 Pitfalls
Failure to leave at least 2 mm of the radial edge of the fourth metacarpal—hamate articulation and 2 mm of the ulnar edge of the fifth metacarpal—hamate joint may lead to CMC joint instability.
Avoid making the coronal osteotomy too obliquely because this might prevent adequate restoration of joint geometry and potentially lead to instability.
The coronal plane osteotomy must be done carefully to avoid fracture of the osteochondral autograft.
Step 3: Graft Fixation
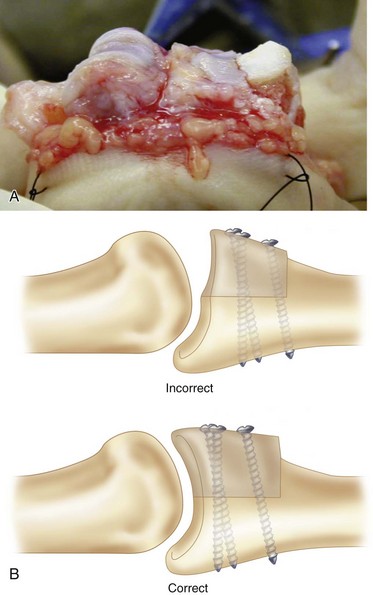
 Contour the graft as needed to fill the defect, giving special attention to reconstructing the concave articular surface. Additional bone graft may be used distally if the hamate graft is too vertical (Fig. 52-9).
Contour the graft as needed to fill the defect, giving special attention to reconstructing the concave articular surface. Additional bone graft may be used distally if the hamate graft is too vertical (Fig. 52-9).
 Provisionally secure the autograft with a 0.028-inch K-wire.
Provisionally secure the autograft with a 0.028-inch K-wire.
 Secure the graft with two 1.1- or 1.3-mm screws on either side of the provisional K-wire. A third screw placed into the hole is left once the K-wire is removed if the graft is large enough (Fig. 52-10).
Secure the graft with two 1.1- or 1.3-mm screws on either side of the provisional K-wire. A third screw placed into the hole is left once the K-wire is removed if the graft is large enough (Fig. 52-10).
 Reduce the PIP joint and assess rotational alignment and joint stability throughout an arc of motion.
Reduce the PIP joint and assess rotational alignment and joint stability throughout an arc of motion.
 Assess the screw length under fluoroscopy.
Assess the screw length under fluoroscopy.
 Trim the distal volar surface of the graft so that there is a smooth transition between the graft and the volar cortex of the middle phalanx.
Trim the distal volar surface of the graft so that there is a smooth transition between the graft and the volar cortex of the middle phalanx.
Step 3 Pearls
Make every effort to cant the graft into 10 to 15 degrees of extension so as to better restore the cup-shaped contour of the base of the middle phalanx.
The hamate articular cartilage is thicker than the middle phalanx cartilage, which creates an apparent radiographic stepoff (Fig. 52-11). Direct visualization of the joint will confirm the lack of an articular stepoff.
The joint should remain located throughout a full range of motion. Dorsal subluxation suggests that the graft has been set too “flat,” failing to restore a concave articular surface.
Step 4: Closure
 Reattach the volar plate to the middle phalanx with a 4-0 nonabsorbable suture. The suture can be secured through small drill holes if necessary.
Reattach the volar plate to the middle phalanx with a 4-0 nonabsorbable suture. The suture can be secured through small drill holes if necessary.
 Reattach the collateral ligaments to the stumps on the middle phalanx.
Reattach the collateral ligaments to the stumps on the middle phalanx.
 Reapproximate the flexor tendon sheath flap over the PIP joint with a 6-0 absorbable suture.
Reapproximate the flexor tendon sheath flap over the PIP joint with a 6-0 absorbable suture.
 Deflate the tourniquet and obtain hemostasis.
Deflate the tourniquet and obtain hemostasis.
 Close the skin and apply a bulky dressing and dorsal splint with the PIP joint in 20 degrees of flexion.
Close the skin and apply a bulky dressing and dorsal splint with the PIP joint in 20 degrees of flexion.
Postoperative Care and Expected Outcomes
 Remove the dressing on postoperative day 3 to 5. Apply an elastic sleeve for edema control and a figure-of-eight splint to prevent PIP joint hyperextension.
Remove the dressing on postoperative day 3 to 5. Apply an elastic sleeve for edema control and a figure-of-eight splint to prevent PIP joint hyperextension.
 Begin active PIP joint flexion with an extension block splint that prevents full PIP joint extension.
Begin active PIP joint flexion with an extension block splint that prevents full PIP joint extension.
 At the same time, begin active and passive motion of the metacarpophalangeal and distal interphalangeal joints.
At the same time, begin active and passive motion of the metacarpophalangeal and distal interphalangeal joints.
 If the radiographs at 3 weeks show concentric joint reduction and solid graft fixation, begin gentle active assisted flexion and extension of the PIP joint.
If the radiographs at 3 weeks show concentric joint reduction and solid graft fixation, begin gentle active assisted flexion and extension of the PIP joint.
 Obtain radiographs 6 weeks postoperatively to confirm solid graft fixation and concentric joint reduction (see Fig. 52-11). Begin passive range of motion into flexion and correction of an excessive (>20 degrees) PIP flexion contracture with dynamic extension splinting.
Obtain radiographs 6 weeks postoperatively to confirm solid graft fixation and concentric joint reduction (see Fig. 52-11). Begin passive range of motion into flexion and correction of an excessive (>20 degrees) PIP flexion contracture with dynamic extension splinting.
 The figure-of-eight splint can be discontinued at 8 weeks.
The figure-of-eight splint can be discontinued at 8 weeks.
 Allow full, unrestricted use at 12 weeks.
Allow full, unrestricted use at 12 weeks.
 The procedure can restore a stable, well-aligned PIP joint with a functional arc of motion of 90 degrees. A 15- to 20-degree extension contracture is not uncommon.
The procedure can restore a stable, well-aligned PIP joint with a functional arc of motion of 90 degrees. A 15- to 20-degree extension contracture is not uncommon.
Calfee RP, Kiefhaber TR, Sommerkamp TG, et al. Hemi-hamate arthroplasty provides functional reconstruction of acute and chronic proximal interphalangeal fracture-dislocations. J Hand Surg [Am]. 2009;34:1232-1241.
Williams RMM, Kiefhaber TR, Sommerkamp TG, et al. Proximal interphalangeal fracture/dislocations using a hemi-hamate autograft. J Hand Surg [Am]. 2003;28:856-865.