Procedure 5 Surgical Treatment of Trigger Digits
![]() See Video 2: Surgical Treatment of Trigger Digits
See Video 2: Surgical Treatment of Trigger Digits
Indications
 Failure of tendon sheath steroid injections
Failure of tendon sheath steroid injections
 A fixed flexion contracture of the proximal interphalangeal (PIP) joint owing to the triggering
A fixed flexion contracture of the proximal interphalangeal (PIP) joint owing to the triggering
Examination/Imaging
Clinical Examination
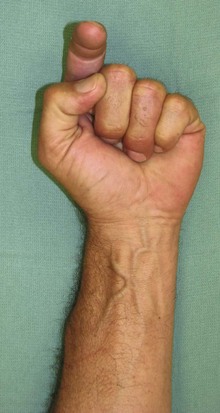
 The patient is examined for a palpable nodule at the level of A1 pulley. The patient may be unable to flex the finger or experience a catching when the finger flexes as the enlarged tendon passes through the A1 pulley (Fig. 5-1).
The patient is examined for a palpable nodule at the level of A1 pulley. The patient may be unable to flex the finger or experience a catching when the finger flexes as the enlarged tendon passes through the A1 pulley (Fig. 5-1).
 The grade of triggering should be recorded for follow-up purposes (Table 5-1). One should look for tenderness over the A1 pulley and a palpable nodule. In long-standing triggering, a flexion contracture of the PIP joint may be present, and the degree of contracture should be noted.
The grade of triggering should be recorded for follow-up purposes (Table 5-1). One should look for tenderness over the A1 pulley and a palpable nodule. In long-standing triggering, a flexion contracture of the PIP joint may be present, and the degree of contracture should be noted.
 The most frequently involved digit is the ring finger, followed by the thumb and the long, small, and index fingers. Patients who present with primary index finger trigger must be evaluated for associated conditions like diabetes and rheumatoid arthritis.
The most frequently involved digit is the ring finger, followed by the thumb and the long, small, and index fingers. Patients who present with primary index finger trigger must be evaluated for associated conditions like diabetes and rheumatoid arthritis.
 In patients with rheumatoid arthritis, one must carefully differentiate between the snapping observed in fingers with early swan-neck deformity and the catching seen in trigger finger. The snapping finger is due to the sudden return of the lateral bands from a dorsal to a palmar location over the condyle of the proximal phalanx as the patient actively corrects the hyperextension deformity. Occasionally triggering may be due to flexor tendon nodules getting caught under the carpal tunnel.
In patients with rheumatoid arthritis, one must carefully differentiate between the snapping observed in fingers with early swan-neck deformity and the catching seen in trigger finger. The snapping finger is due to the sudden return of the lateral bands from a dorsal to a palmar location over the condyle of the proximal phalanx as the patient actively corrects the hyperextension deformity. Occasionally triggering may be due to flexor tendon nodules getting caught under the carpal tunnel.
 Rarely, a locked metacarpophalangeal (MCP) joint can be confused with a trigger finger. A trigger finger primarily affects the interphalangeal joints and is usually gradual in onset, in contrast to the sudden onset of MCP joint locking. MCP joint locking usually results from collateral ligament injury, sesamoid, or osteophyte entrapment.
Rarely, a locked metacarpophalangeal (MCP) joint can be confused with a trigger finger. A trigger finger primarily affects the interphalangeal joints and is usually gradual in onset, in contrast to the sudden onset of MCP joint locking. MCP joint locking usually results from collateral ligament injury, sesamoid, or osteophyte entrapment.
 Congenital trigger thumb most commonly presents with a fixed flexion deformity, and less commonly with triggering. A characteristic nodule (Notta node) can be palpated on the flexor pollicis longus (FPL) tendon at the region of the A1 pulley. This can help differentiate congenital trigger thumb from other clasped thumb deformities.
Congenital trigger thumb most commonly presents with a fixed flexion deformity, and less commonly with triggering. A characteristic nodule (Notta node) can be palpated on the flexor pollicis longus (FPL) tendon at the region of the A1 pulley. This can help differentiate congenital trigger thumb from other clasped thumb deformities.
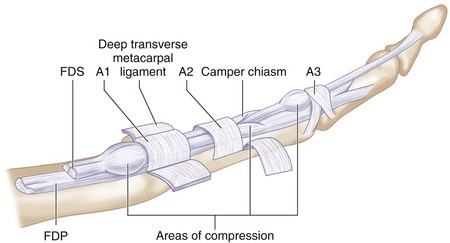
 Congenital trigger finger is a distinct entity related to abnormal thickening of the flexor digitorum superficialis (FDS) and flexor digitorum profundus (FDP), calcifications or granulations within the tendons, or abnormal relationship of the tendons at the FDS decussation. The common sites for triggering in a congenital trigger finger are the A1 pulley, the FDS chiasm, and the A3 pulley (Fig. 5-2).
Congenital trigger finger is a distinct entity related to abnormal thickening of the flexor digitorum superficialis (FDS) and flexor digitorum profundus (FDP), calcifications or granulations within the tendons, or abnormal relationship of the tendons at the FDS decussation. The common sites for triggering in a congenital trigger finger are the A1 pulley, the FDS chiasm, and the A3 pulley (Fig. 5-2).
| Grade I | Before triggering | History of triggering, but not demonstrable on examination |
| Grade II | Active | Demonstrable triggering, but patient can actively overcome the trigger |
| Grade III | Passive | Demonstrable triggering, but patient cannot actively overcome trigger |
| • IIIA | • Extension | • Locked in flexion and needs passive extension to overcome trigger |
| • IIIB | • Flexion | • Locked in extension and needs passive flexion to overcome trigger |
| Grade IV | Contracture | Demonstrable trigger with flexion contracture of posterior interphalangeal joint |
Surgical Anatomy
 Triggering occurs at the proximal edge of the A1 pulley for the fingers and the thumb.
Triggering occurs at the proximal edge of the A1 pulley for the fingers and the thumb.
 The proximal edge of the A1 pulley for the small and ring fingers is in line with the distal palmar crease; for the long finger, it is midway between the distal and proximal palmar creases; and for the index finger, it is in line with the proximal palmar crease. The proximal edge of the A1 pulley of the thumb is at the level of the MCP joint crease.
The proximal edge of the A1 pulley for the small and ring fingers is in line with the distal palmar crease; for the long finger, it is midway between the distal and proximal palmar creases; and for the index finger, it is in line with the proximal palmar crease. The proximal edge of the A1 pulley of the thumb is at the level of the MCP joint crease.
 Biomechanical studies have shown that the integrity of the A2 and A4 annular pulleys is most important to prevent bowstringing in the fingers. Therefore, it is important to prevent injury to the A2 pulley during division of the A1 pulley. Similarly, the oblique pulley in the thumb prevents bowstringing and should be preserved.
Biomechanical studies have shown that the integrity of the A2 and A4 annular pulleys is most important to prevent bowstringing in the fingers. Therefore, it is important to prevent injury to the A2 pulley during division of the A1 pulley. Similarly, the oblique pulley in the thumb prevents bowstringing and should be preserved.
Exposures
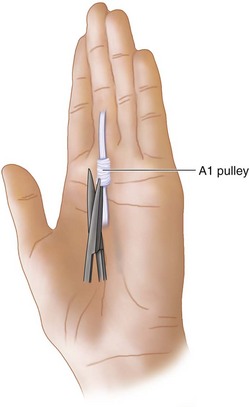
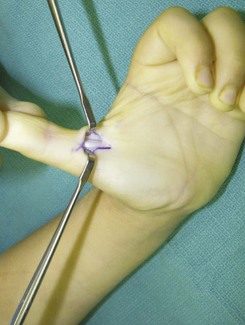
 A 1-cm transverse incision is made in line with the distal palmar crease for the long, ring, and small fingers and at the proximal palmar crease for the index finger (Fig. 5-3).
A 1-cm transverse incision is made in line with the distal palmar crease for the long, ring, and small fingers and at the proximal palmar crease for the index finger (Fig. 5-3).
 A 2-cm chevron-shaped apex radial incision is made over the MCP joint crease (a more extensile incision to visualize the digital nerves) for release of thumb trigger.
A 2-cm chevron-shaped apex radial incision is made over the MCP joint crease (a more extensile incision to visualize the digital nerves) for release of thumb trigger.
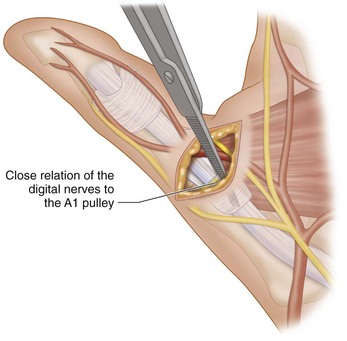
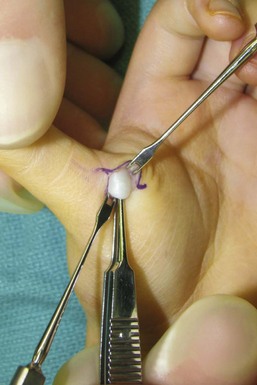
 The subcutaneous fat is gently spread with scissors to expose the tendon sheath and the A1 pulley. Two Ragnell retractors are held by the assistant to maintain visualization (Fig. 5-4).
The subcutaneous fat is gently spread with scissors to expose the tendon sheath and the A1 pulley. Two Ragnell retractors are held by the assistant to maintain visualization (Fig. 5-4).
Pitfalls
Procedure
Primary Trigger Finger Release
Step 1
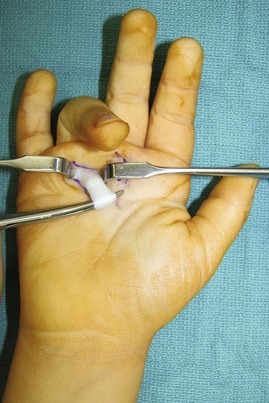
 The A1 pulley is exposed with gentle traction of the soft tissues and incised with a no. 15 blade (Fig. 5-6).
The A1 pulley is exposed with gentle traction of the soft tissues and incised with a no. 15 blade (Fig. 5-6).
 Once identified and partially divided, the scissors is used to complete the sheath division (Fig. 5-7).
Once identified and partially divided, the scissors is used to complete the sheath division (Fig. 5-7).
 Any excessive synovial tissue should also be excised, if encountered.
Any excessive synovial tissue should also be excised, if encountered.
 A tendon hook is used to provide traction on the FDS, and then the FDP, ensuring that it results in smooth flexion of the PIP joint and distal interphalangeal (DIP) joint, respectively. It is advisable to ask the patient to move the fingers actively to determine whether there is any limitation of tendon excursion.
A tendon hook is used to provide traction on the FDS, and then the FDP, ensuring that it results in smooth flexion of the PIP joint and distal interphalangeal (DIP) joint, respectively. It is advisable to ask the patient to move the fingers actively to determine whether there is any limitation of tendon excursion.
Step 1 Pearls
The scissor tips should be placed parallel to the course of the tendon sheath during soft tissue dissection to avoid injury to the neurovascular bundles.
Patients with rheumatoid arthritis and trigger fingers need flexor tenosynovectomy. A1 pulley release may be done only after tenosynovectomy has failed to relieve the trigger. The release of the A1 pulley may contribute to the MCP joint ulnar drift deformity, especially for the index and long fingers, because of the oblique line of pull of the long flexors for these digits. Because of this tendency, some surgeons recommend resection of one slip of the FDS to provide more space for passage of the FDP, as opposed to an A1 pulley release.
Procedure
Congenital Trigger Thumb
Step 1
 A longitudinal chevron incision is designed over the metacarpophalangeal joint crease, corresponding to the A1 pulley (Fig. 5-8).
A longitudinal chevron incision is designed over the metacarpophalangeal joint crease, corresponding to the A1 pulley (Fig. 5-8).
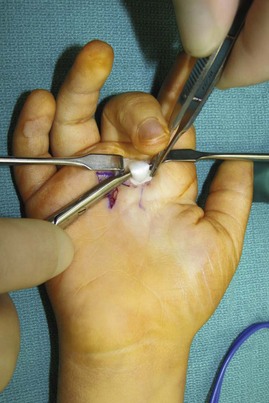
 The A1 pulley and FPL tendon, often with a focal enlargement called the Notta node, are identified using blunt dissection, with care taken to identify and protect the radial digital nerve (Fig. 5-9).
The A1 pulley and FPL tendon, often with a focal enlargement called the Notta node, are identified using blunt dissection, with care taken to identify and protect the radial digital nerve (Fig. 5-9).
 The A1 pulley is incised with a no. 15 blade, and the remainder of the division is completed with a tenotomy scissors under direct visualization (Fig. 5-10).
The A1 pulley is incised with a no. 15 blade, and the remainder of the division is completed with a tenotomy scissors under direct visualization (Fig. 5-10).
Procedure
Congenital Trigger Finger
 Congenital trigger finger is rare. It is usually due to an enlarged tendon or abnormal anatomic relationship of the FDS and FDP at the FDS decussation. Treatment is directed at specific intraoperative findings but may include not only A1 pulley release but also partial resection of the FDP or FDS tendon.
Congenital trigger finger is rare. It is usually due to an enlarged tendon or abnormal anatomic relationship of the FDS and FDP at the FDS decussation. Treatment is directed at specific intraoperative findings but may include not only A1 pulley release but also partial resection of the FDP or FDS tendon.
Step 1
Step 2
 Intraoperative traction is applied to the flexor tendons, and they are observed for triggering—most commonly at the FDS decussation or under A2 (Fig. 5-14).
Intraoperative traction is applied to the flexor tendons, and they are observed for triggering—most commonly at the FDS decussation or under A2 (Fig. 5-14).
 If triggering is observed, the focally thickened tendon is partially shaved to decrease the bulk, and the FDS decussation is opened partially to permit easier movement to the FDP through the decussation.
If triggering is observed, the focally thickened tendon is partially shaved to decrease the bulk, and the FDS decussation is opened partially to permit easier movement to the FDP through the decussation.
 If triggering is not yet completely resolved, partial division of A2 may be required (Fig. 5-15).
If triggering is not yet completely resolved, partial division of A2 may be required (Fig. 5-15).
Bae DS, Sodha S, Waters PM. Surgical treatment of the pediatric trigger finger. J Hand Surg [Am]. 2007;32:1043-1047.
Marks MR, Gunther SF. Efficacy of cortisone injection in treatment of trigger fingers and thumbs. J Hand Surg [Am]. 1989;14:722-727.
Wilhelmi BJ, Snyder N, Verbesey JE, et al. Trigger finger release with hand surface landmark ratios: an anatomic and clinical study. Plast Reconstr Surg. 2001;108:908-915.