CASE 5 Nondilatable Lesion
Cardiac catheterization
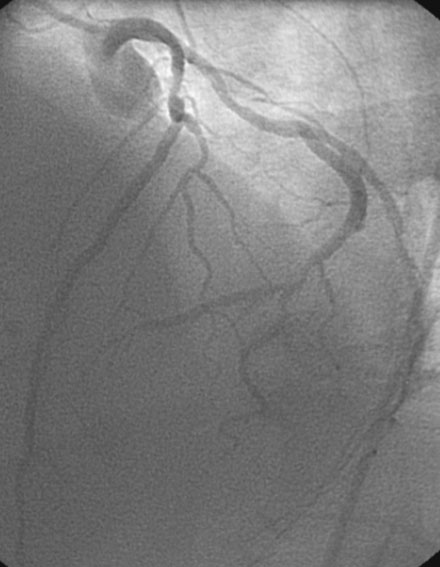
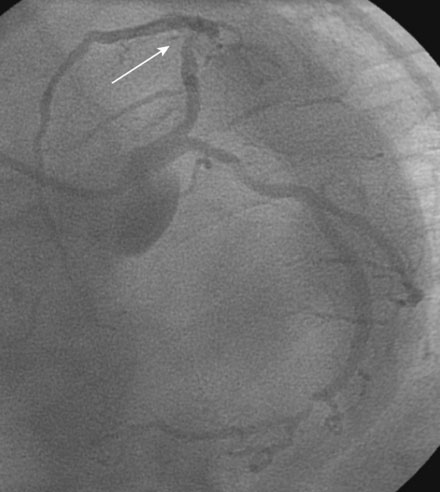
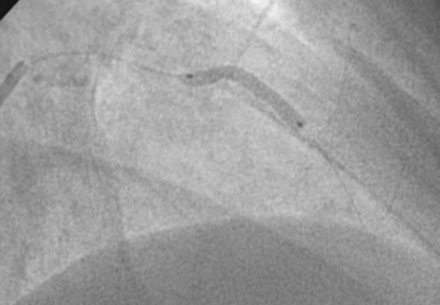
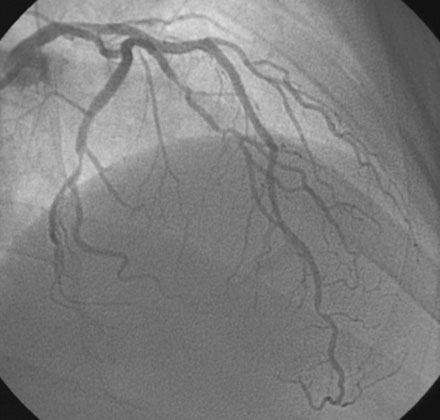
Ventriculography revealed normal left ventricular function. Coronary angiographic findings included a codominant circulation, with a diffusely diseased but small right coronary artery (Figure 5-1) and moderate distal disease in the left circumflex and obtuse marginal branches (Figures 5-2, 5-3). The proximal segment of the left anterior descending artery contained moderate disease (Figure 5-2 and Video 5-1) that in some views appeared nonobstructive (Figures 5-2, 5-3) but in other views appeared more concerning (Figure 5-4 and Video 5-2). Much of the disease present on this study appeared similar to the appearance on angiography 4 years earlier, leaving the operator at a loss for the dramatic change in symptoms.
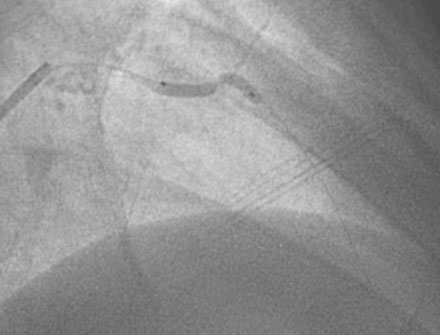
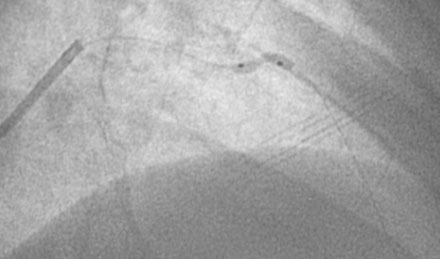
The concerning symptoms, along with an ambiguous lesion in the proximal left anterior descending artery, prompted the operator to measure fractional flow reserve of this vessel (Figure 5-5). After a 6 French guide catheter was inserted, a pressure wire was advanced past the lesion and hyperemia induced with 100 μg of intracoronary adenosine; fractional flow reserve measured 0.69. Thus, the angiographically-moderate disease represented a flow-limiting lesion, and the operator decided to treat the lesion percutaneously. Following the administration of intravenous heparin and eptifibatide, the procedure began with balloon predilatation, using a 2.5 mm by 20 mm long compliant balloon. At nominal inflation pressure, a significant waist remained in the compliant balloon (Figure 5-6 and Video 5-3). Switching to a 2.5 mm by 10 mm noncompliant balloon inflated to 18 atmospheres failed to fully expand the balloon (Figure 5-7). Although these balloon inflations did not improve the luminal appearance, there was no evidence of dissection or perforation (Figure 5-8 and Video 5-4).
Faced with a rigid and undilatable lesion, the operator chose to perform rotational atherectomy with a 1.5 mm burr. Three 30-second runs at 160,000 rpm successfully allowed the burr to pass the diseased area without deceleration (Video 5-5). Following this, a 2.5 mm by 20 mm long compliant balloon fully inflated at nominal pressure (Figure 5-9). Two, everolimus-eluting stents (2.5 mm diameter by 23 mm long and 2.5 mm by 18 mm long) easily crossed and expanded fully at 16 atmospheres of pressure, resulting in an excellent final angiographic appearance (Figure 5-10 and Videos 5-6, 5-7).
Discussion
This case provides two valuable lessons to a budding interventional cardiologist. First, it is an excellent example of one of the important limitations of coronary angiography. The hemodynamic significance of many lesions of only moderate severity may be very difficult to assess by angiography alone, potentially leading to a wrong decision.1 Although the patient presented with a convincing history of crescendo angina pectoris, on first glance, the angiogram did not reveal an obvious culprit lesion. In fact, the angiogram appeared very similar to one he had 4 years earlier. Despite careful review of the angiogram and multiple angiographic views, the operator was unable to decide if the disease in the left anterior descending artery represented a significant lesion. This is the ideal time to consider further assessment of the artery by either intravascular ultrasound or fractional flow reserve. In this case, fractional flow reserve confirmed the hemodynamic significance of the disease and led to a revascularization decision that successfully eliminated the patient’s symptoms.
This case also provides an example of a potential risk of direct stenting (i.e., without balloon predilatation). Some operators choose this tactic in an effort to save time and reduce equipment cost. However, in this case, this approach would have resulted in an underexpanded and poorly-deployed stent. When this occurs, options are limited, which might have led to aggressive balloon inflations at very high pressures in a desperate effort to expand the stent, potentially causing a perforation or dissection in adjacent segments. Failure to fully expand the stent, in spite of these measures, often leads to an adverse outcome, including stent thrombosis or restenosis.2,3
1 Fischer J.J., Samady H., McPherson J.A., Sarembock I.J., Powers E.R., Gimple L.W., Ragosta M. Comparison between visual assessment and quantitative angiography versus fractional flow reserve for native coronary narrowings of moderate severity. Am J Cardiol. 2002;90:210-215.
2 Fujii K., Carlier S.G., Mintz G.S., Yang Y.M., Moussa I., Weisz G., Dangas G., Mehran R., Lansky A.J., Kreps E.M., Collins M., Stone G.W., Moses J.W., Leon M.B. Stent underexpansion and residual reference segment stenosis are related to stent thrombosis after sirolimus-eluting stent implantation: an intravascular ultrasound study. J Am Coll Cardiol. 2005;45:995-998.
3 Fujii K., Mintz G.S., Kobayashi Y., Carlier S.G., Takebayashi H., Yasuda T., Moussa I., Dangas G., Mehran R., Lansky A.J., Reyes A., Kreps E., Collins M., Colombo A., Stone G.W., Teirstein P.S., Leon M.B., Moses J.W. Contribution of stent underexpansion to recurrence after sirolimus-eluting stent implantation for in-stent restenosis. Circulation. 2004;109:1085-1088.