CHAPTER 5
Cervical Radiculopathy
Ali Mostoufi, MD, FAAPMR, FAAPM
Definition
Cervical radiculopathy is dysfunction of a cervical nerve root resulting in pain in the neck and arm with associated sensory, motor, and reflex abnormalities. Involvement of the ventral root of the spinal nerve results in motor weakness, and involvement of the dorsal root of the spinal nerve results in sensory deficits. Involvement of either root may result in reflex abnormality because the reflex arc comprises both (pertinent to C5, C6, and C7). In most cases, both the ventral and dorsal roots are affected, resulting in motor and sensory cervical radiculopathy.
Cervical radicular pain refers to neck pain radiating to the arm in a specific nerve root pattern, but it is not necessarily associated with loss of sensation, motor deficit, or reflex abnormality. A patient could experience radicular neck pain without abnormal physical examination findings that are characteristic of radiculopathy.
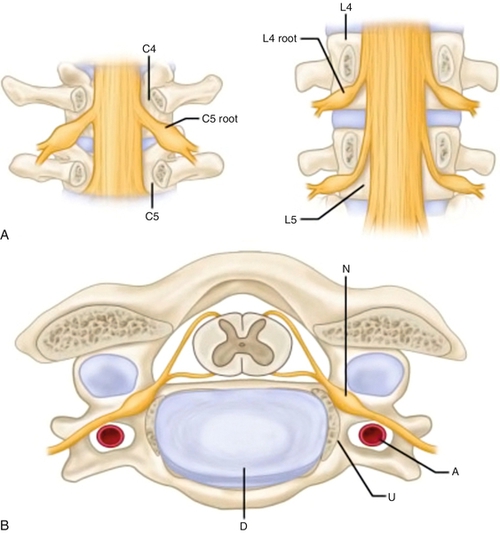
Cervical spine anatomy is complex (Fig. 5.1). There are seven cervical vertebrae (C1-C7). The C1 vertebra is ring shaped, and its lateral masses articulate with the occipital condyle of the skull. The vertebral body of C2 is marked by the cephalad extension of the dens, which is secured in place by the transverse ligament. There are six intervertebral discs (C2-C7) located anteriorly in between vertebral bodies of adjacent vertebrae. C2-C7 vertebrae articulate posterolaterally through facet joints, which are situated in the coronal plane with inferior angulations. C3-C7 vertebrae also have a unique articulation through the uncovertebral joint. There are eight pairs of cervical nerve roots. The names of the cervical nerves correspond to the vertebral body below the nerve, except C8. The C8 roots exit at the C7-T1 intervertebral foramen. The foramina are largest in the upper cervical spine and gradually narrow distally, with the C7-T1 foramen being the narrowest [1]. Cervical nerve roots exit through the inferior portion of the cervical intervertebral foramina [1]. The C1-C3 spinal nerves have dorsal innervations including suboccipital (C1), greater occipital (C2), and third occipital nerves (C3) [2]. The C1-C4 ventral primary rami form the cervical plexus, and the C5-C8 ventral primary rami contribute to the brachial plexus innervating the arm [3]. Each cervical intervertebral foramen is bordered posterolaterally by the zygapophyseal joint (facets), anteromedially by the uncovertebral joint, and inferiorly and superiorly by the pedicles of the adjacent vertebrae. Intervertebral discs are located anteriorly, and they separate vertebral bodies to lend height to the intervertebral foramina.
The most common radiculopathy is C7, followed by C6, C8, and C5 in descending order of incidence [4]. The most common reasons for cervical radiculopathy are posterolateral herniated disc (Fig. 5.2); narrowing of the neuroforamina due to facet spondylosis; hypertrophied uncinate process with neuroforaminal encroachment; and spondylolisthesis, with or without instability, narrowing adjacent neuroforamina. Less common causes include facet synovial cyst with encroachment of nerve root, extradural mass, spinal tumors, and abscess. Other medical conditions that resemble cervical radicular symptoms should be carefully ruled out as part of medical evaluation of neck and arm pain (Table 5.1). These include musculoskeletal, neurologic, and rheumatologic disorders.
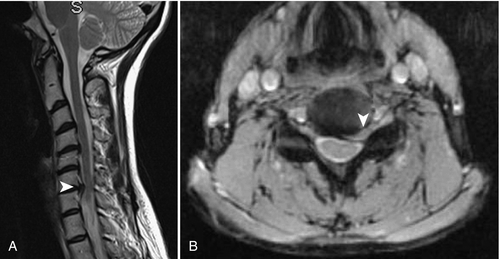
Table 5.1
Differential Diagnosis of Cervical Radiculopathy by System
| Musculoskeletal | Tendinopathy, tenosynovitis, epicondylitis, bursitis Peripheral joint disease (shoulder, elbow, wrist, hand) Rotator cuff tear Glenoid labral defect (Bankart or SLAP lesion) Shoulder impingement syndrome Adhesive capsulitis |
| Neurologic | Peripheral neuropathy Peripheral entrapments Brachial plexus injury Syringomyelia Demyelinating disease Neuromuscular disease Complex regional pain syndrome |
| Infections | Lyme disease Herpes |
| Tumors | Pancoast tumor Spinal tumors (primary or metastatic) |
| Vascular | Thoracic outlet syndrome Aortic arch syndrome |
| Rheumatologic | Polymyalgia rheumatica Fibromyalgia Myofascial pain syndrome |
SLAP, Superior labral tear from anterior to posterior.
Symptoms
The most common symptom of cervical radiculopathy is neck pain with associated unilateral arm pain in a specific nerve root pattern. Sensory complaints of numbness, tingling, burning, or electrical sensation follow a dermatomal pattern, and weakness follows the same anatomic-level myotomal pattern. Of the subjective complaints, the distribution of hand paresthesias appears to have the greatest localizing value [5]. Literature supports that suprascapular (C5-C6), interscapular (C7), and scapular (C8) pain suggests radiculopathy [6]. Symptoms can be aggravated by motion of the head toward the painful side, free hanging of the arm, lifting of heavier items, coughing, sneezing, and Valsalva maneuver. Pulling, pushing, and lifting of items are often not tolerated in the acute phase. Pain may improve when the head is tilted away from the painful side or if the affected arm is abducted over the head. Clumsiness, fine motor deficits, and mild grip weakness may precede gross weakness. Clinicians should routinely inquire about symptoms of myelopathy. Myelopathy symptoms are bilateral hand numbness or paresthesias, altered dexterity, poor balance, falls, and bowel or bladder dysfunction. These symptoms are not features of a discrete radiculopathy and should alert the clinician to rule out spinal cord compression.
Physical Examination
A complete musculoskeletal and neurologic examination is indicated in the evaluation of cervical radiculopathy. Special attention is needed to differentiate between objective findings compatible with radiculopathy and myelopathy signs. Physical examination needs to be expanded if other system involvement is suspected.
Visual Observation
Simple observation is a first step to proper diagnosis and treatment. A clinician’s eyes should be trained to notice poor posture, body mechanics, spinal deformity, muscle atrophy, asymmetric gait, use of assistive devices, skin abnormalities, and nonverbal behaviors.
Gait Evaluation
Examination of gait is an important step in differentiating radicular neck pain from myelopathy. Gait should be normal in cervical radiculopathy and could be abnormal in cervical myelopathic patients.
Palpation
In patients with radiculopathy, ipsilateral tenderness and muscle spasm are common. The clinician should examine muscles for taut bands or tender points.
Range of Motion
Range of motion (ROM) of the cervical spine in all planes should be examined and deficits should be documented. Clinicians should carefully reevaluate ROM of the cervical spine to monitor progress in treatment. The normal cervical ROM is as follows: extension, 55 degrees; flexion, 45 degrees; lateral bending, 40 degrees; rotation, 75 degrees [7]. Among activities of daily living, backing up a car requires the most available range. Personal hygiene, such as hand washing, shaving, and applying makeup, necessitates a significantly greater cervical ROM relative to mobility activities of daily living, including walking and negotiating stairs [7].
Sensory Testing
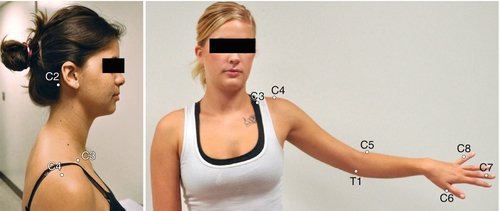
Radiculopathy results in dermatomal sensory abnormality in the neck, shoulder girdle, and ipsilateral arm. On the basis of the specific dermatomal deficits, a clinician can localize the anatomic level of nerve root impingement. Light touch, pinprick, two-point discrimination, proprioception, and vibration sense should be tested in both the symptomatic and symptom-free arm. There is a degree of overlap between dermatomal innervations of the arm. To date, the International Standards for Neurological Classification of Spinal Cord Injury is the most standardized sensory testing guideline [8]. For consistent examination, the use of these guidelines is recommended to examine sensory function in the upper limb (Fig. 5.3).
Deep Tendon Reflexes
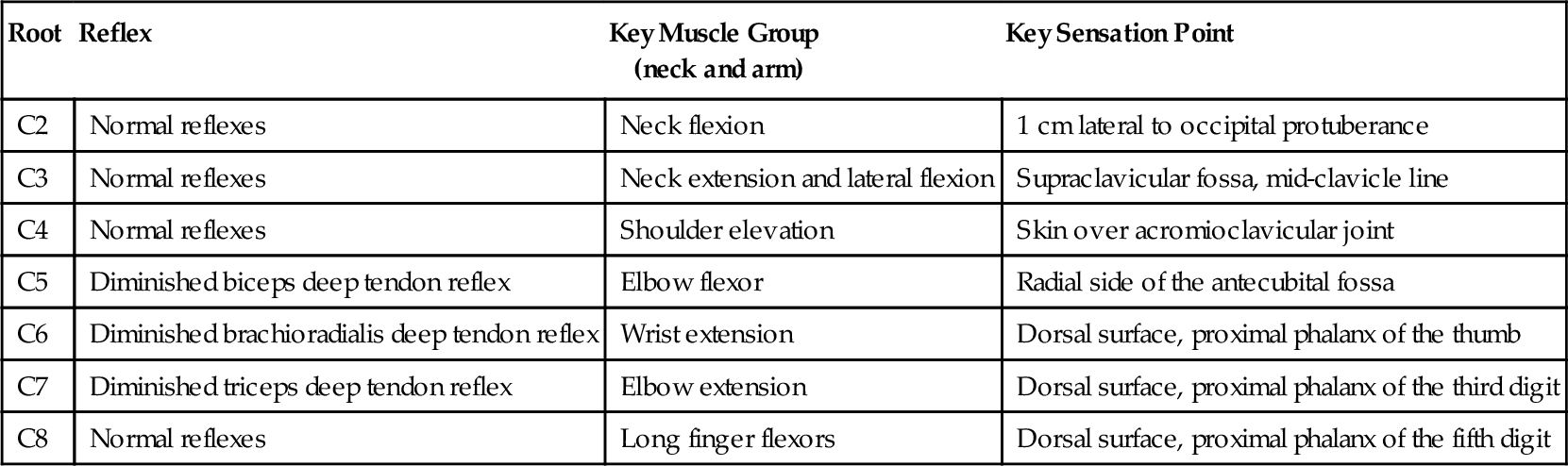
The most frequently tested reflexes in the upper limb are the biceps brachii (innervation C5/6, C5 primary), the brachioradialis (C5/6, C6 primary), and the triceps (C7 primary). Reflexes are tested bilaterally and compared. Hyporeflexia (diminished) or areflexia (complete absence) indicates involvement of the lower motor neuron, including the specific nerve root tested. Hyperreflexia (increased or brisk reflex) is an indication of central nervous system involvement. The response levels of deep tendon reflexes are graded 0 to 4 +, with 2 + being normal (Table 5.2 and Fig. 5.4).
Table 5.2
Muscle Group and Sensory Point Testing in Cervical Radiculopathy [8]: Upper Extremity Key Reflexes
| Root | Reflex | Key Muscle Group (neck and arm) |
Key Sensation Point |
| C2 | Normal reflexes | Neck flexion | 1 cm lateral to occipital protuberance |
| C3 | Normal reflexes | Neck extension and lateral flexion | Supraclavicular fossa, mid-clavicle line |
| C4 | Normal reflexes | Shoulder elevation | Skin over acromioclavicular joint |
| C5 | Diminished biceps deep tendon reflex | Elbow flexor | Radial side of the antecubital fossa |
| C6 | Diminished brachioradialis deep tendon reflex | Wrist extension | Dorsal surface, proximal phalanx of the thumb |
| C7 | Diminished triceps deep tendon reflex | Elbow extension | Dorsal surface, proximal phalanx of the third digit |
| C8 | Normal reflexes | Long finger flexors | Dorsal surface, proximal phalanx of the fifth digit |
Motor Testing
Subjective weakness in the upper limb is a common complaint in patients with radiculopathy. Patterns of weakness can help localize a lesion to a particular spinal cord level, nerve root, peripheral nerve, or muscle. Comparison of the strength of each muscle group with its contralateral counterpart allows the detection of any asymmetries. The degree of pain and the patient’s effort can be limiting factors in the examination of muscle strength. Relevant to cervical radiculopathy, strength testing is often focused on muscles innervated by the C4-C8 nerve roots. The International Standards for Neurological Classification of Spinal Cord Injury has standardized and recommends testing of five key muscles in the upper limb: C5 elbow flexors, C6 wrist extensors, C7 elbow extensor, C8 long finger flexors, and T1 small finger abductor [8] (Table 5.3). Muscle strength is rated on a scale of 0/5 to 5/5. When weakness is detected in one of the key muscle groups, the clinician has to reexamine individual muscles in the arm to further localize the lesion (brachial plexus roots vs trunks vs divisions vs cord).
Table 5.3
Sample of Neck and Arm Muscles or Muscle Groups Innervated by Cervical Roots [3,33]
| Root | Muscle or Muscle Group |
| C2 | Sternocleidomastoid, rectus capitis, longus colli |
| C3 | Trapezius, splenius capitis |
| C4 | Trapezius, levator scapulae |
| C5 | Elbow flexors, deltoid, biceps, supraspinatus, infraspinatus |
| C6 | Wrist extensors, biceps, brachioradialis, supinator |
| C7 | Elbow extensors, wrist flexors, triceps |
| C8 | Flexor digitorum superficialis, thumb extensor and adductors, wrist ulnar deviators |
Joint Examination
Cervical facets can be examined by ROM testing and also by localized external pressure on them. These maneuvers may reproduce neck pain or head pain concordant with the patient’s nonradicular complaint. Referred pain from facets to the shoulder girdle or scapular region may be confused with radicular pain of similar distribution. Careful examination of the shoulder as well as of the elbow and wrist is also important in differentiating radicular neck pain from other musculoskeletal causes of arm pain.
Special Maneuvers
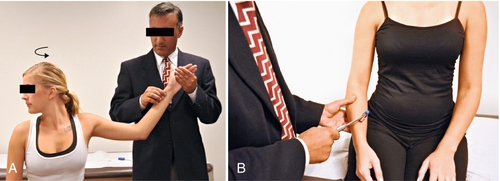
The Spurling maneuver is a classic test used to identify nerve root irritation (Fig. 5.5). This test is a combination of ipsilateral tilt and forward flexion of the neck while the examiner exerts axial load. The modified Spurling test is a combination of ipsilateral rotation, extension, and axial compression of the head. Reproduction of the patient’s radicular symptoms (distal to the shoulder) in either maneuver is considered a positive test result. Several studies have shown that the Spurling test has a low sensitivity (30%-40%), high specificity (80%-90%), and fair to good interexaminer reliability [9,10]. The Spurling test should be avoided if fracture or instability is suspected.
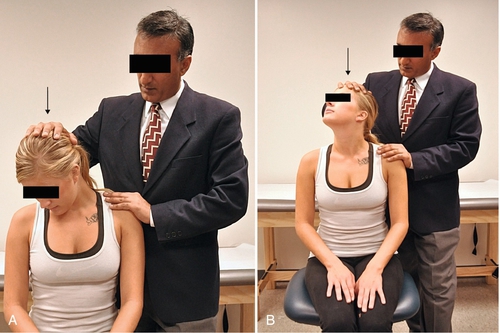
Clinicians should be familiar with the Adson and Roos tests in examining patients with neck and arm pain (see Fig. 5.4). Pain, weakness, and neurovascular deficits are associated with thoracic outlet syndrome, part of the differential diagnosis of cervical radiculopathy.
Lhermitte sign is a sudden painless electric shock–like sensation originating in the neck and spreading down the spine into the limbs when the patient’s neck is flexed. This test was described in a 1924 publication by Lhermitte [11]. Although nonspecific, it is most commonly seen in multiple sclerosis as well as in myelopathy due cervical spondylosis, spinal cord tumors, epidural bleed, and postirradiation therapy.
The neck distraction sign and shoulder abduction test can also determine nerve root irritation [10]. Babinski response, Hoffmann sign, and clonus are also part of the examination of the patient with cervical radiculopathy and may suggest involvement of the central nervous system.
Functional Limitations
Pain commonly interferes with sleep, work, or social activities. With restriction in ROM, driving, overhead activity, and reading may be difficult. Desktop computer work and use of tablet computer and smartphone may result in increased pain. Loss of sensation in the fingers may negatively affect individuals who rely on tactile function for their work. Grip weakness may lead to dropping of items, and proximal muscle weakness will affect the ability to carry items or to pull and push objects. Patients with failed medical and surgical treatments often experience permanent impairment resulting in chronic disabilities.
Diagnostic Studies
Radiography
Radiography is seen as the initial imaging modality to evaluate anatomic changes in the bone structure of the cervical spine. It is sensitive to evaluate fractures, misalignment, spondylolisthesis, facet arthrosis, and disc space narrowing. It can identify instability of the cervical spine by means of dynamic and open mouth views. Although it is often used in urgent care settings for patients with radicular pain, apart from showing the bone narrowing of the neuroforamina and disc space narrowing, it is of little value.
Computed Tomography
Computed tomography (CT) provides exquisite depiction of bone detail of the cervical spine. It is particularly useful in and is considered a primary imaging evaluation for acute spine trauma in adults [12]. It is an excellent modality in multitrauma workup of fractures (C1, C2, and distal cervical segments) and possible bleeding in or around the spinal canal. Because it is a cross-sectional imaging technique, it is able to identify bone narrowing of the central canal and neuroforamina and thickening of the ligamentum flavum. CT is the modality of choice in patients with implanted pacemakers and other devices that do not allow the use of magnetic resonance imaging (MRI). CT with axial and coronal reconstruction is used to identify proper fusion of the adjacent vertebrae after spinal fusion surgery. CT myelography has some indications in complex surgical revisions or postsurgical cases with persistent arm symptoms. CT is used after discography is performed to better visualize internal disc derangements, including radial tears. CT is also used in the workup of possible infection, as in spinal abscess.
Magnetic Resonance Imaging
Compared with CT, MRI is a clinically superior diagnostic test in the evaluation of patients with suspected disc herniation. It should be the diagnostic study of choice when it is available.
MRI is the “gold standard” imaging study for patients with radicular symptoms. It can clearly identify soft tissue abnormalities, including the cord, muscles, and ligaments. With axial images, clinicians can gauge the caliber of the spinal canal and the neuroforamina. With T1- and T2-weighted images, signal abnormality within the spinal cord substance (myelomalacia) and bone marrow can also be evaluated. Acuity of cervical spine fractures as well as primary or metastatic tumors of the spinal column can be assessed by this imaging modality. MRI before and after the administration of a contrast agent is necessary to define certain conditions like cancerous lesions and postsurgical scarring. In workup of a possible infection, MRI can help identify soft tissue signal abnormality, local fluid collection, osteomyelitis, discitis, and abscess formation. Interpretation of the MRI study is difficult after spinal instrumentation because of metallic artifact. In such cases, CT becomes the imaging of choice.
Bone Scan
The utility of the bone scan in spine care is limited to spondylolysis, infection, and metastatic or primary spinal tumors.
Electrodiagnosis
Nerve conduction studies and electromyography are considered an extension of the physical examination. In patients with clear cervical radicular symptoms, supportive MRI, and concordant examination findings, there is no indication for electrodiagnosis. Nerve conduction studies and electromyography can be useful if there is clinical suspicion of peripheral neuropathy or peripheral entrapment that is manifested with symptoms similar to cervical radicular pain. Electromyography can be an additional tool in those cases in which symptoms, physical examination findings, and imaging results are not concordant [13].
Myelography
Before the advent of MRI, myelography was a useful test to examine the caliber of the central canal and intervertebral foramen and possible compression on the nerve root. Its use is currently limited to complex postsurgical cases, surgical revisions, and evaluation of spinal tumors.
Diagnostic Spinal Injections
Fluoroscopically guided contrast-enhanced procedures can deliver medications to a desired target. In complex cases in which multilevel degenerative changes are seen and there is a question of which segment is contributing to the arm pain, spine surgeons may ask for a diagnostic selective nerve root injection. The degree of pain relief within the half-life of the injected anesthetic can provide valuable preoperative information to the surgeon and increase the likelihood of successful surgical treatment. The evidence for selective nerve root blocks in the preoperative evaluation of patients with normal or inconclusive imaging studies is moderate [14].
Provocative discography has been used to diagnose discogenic axial pain. For cervical discogenic pain, discography has a level II-2 support (U.S. Preventive Services Task Force classification, evidence obtained from well-designed cohort or case-control analytic studies, preferably from more than one center or research group) [15]. Complications associated with cervical discography because of the surrounding anatomy include injury to the trachea, esophagus, carotid artery, and jugular veins; nerve root or spinal cord injury; and pneumothorax [3]. The potential complication of discitis is also of concern in considering diagnostic discography [3]. Because there are no well-designed studies to support cervical discography as a diagnostic tool for discogenic neck pain, such a procedure should be considered with utmost caution.
Treatment
Initial
With conservative care, 70% to 80% of patients with cervical radicular symptoms improve [16]. Pain reduction and patient education are important initial goals. For the acute phase, one can consider the use of ice as well as passive treatment consisting of semihard cervical collar immobilization and rest from activities that aggravate the condition. Nonsteroidal anti-inflammatory drugs, muscle relaxants, and, at times, short tapering doses of an oral steroid can be the initial recommended medication treatment for most patients. Stronger pain medications are indicated on the basis of the severity of the pain. In some cases, adjunct medication like anticonvulsants, tricyclic antidepressants, or selective norepinephrine reuptake inhibitors may be used.
Timely involvement of a physical therapist appears beneficial. Manual therapy techniques in conjunction with therapeutic exercise are effective in increasing function, improving active ROM, and decreasing pain and disability [17]. The scientific literature supports the use of cervical traction for management of pain as well as improvement in function and strength in patients with cervical radiculopathy [18,19]. Acupuncture and massage can help reduce muscle tension and pain. There is moderate quality evidence that spinal manipulation is effective for the treatment of acute radiculopathy [20]. It is the responsibility of health care providers to educate patients about their condition and to suggest ways to prevent worsening and recurrence of the symptoms by activity modification, appropriate body mechanics (neutral spine), proper lifting techniques, suitable pillow and mattress use, and appropriate exercises.
Rehabilitation
In the management of cervical radicular pain, early involvement of physical and occupational therapy services is encouraged. The rehabilitation program should focus on reduction of muscle spasm, improvement in ROM, and improvement of muscle strength. Cervical stabilization, stretching (passive and active), static strengthening, and progressive resistive exercises are incorporated in the rehabilitation phase and should be transitioned to a home exercise program [21]. Thermal modalities, manual traction, and transcutaneous electrical nerve stimulation are often used by physiotherapists for temporary pain reduction during this phase. Interventional procedures and medications can reduce pain and increase the patient’s compliance with rehabilitation. Within the framework of rehabilitation, the patient is educated on body mechanics, proper desk ergonomics, and use of adaptive equipment (e.g., book stand, hands-free phone or headset, and document holder).
Procedures
Interlaminar Epidural Steroid Injections
Cervical epidural steroid injection is indicated in persistent painful cervical radiculopathy despite appropriate initial medical and rehabilitation treatments. In the hands of trained physicians, when it is done with image guidance, it is a safe and effective treatment. On the basis of a systematic review of the literature, the evidence for treatment of cervical radicular pain with interlaminar epidural steroid injection is good [22,23]. There is no indication for performing these injections in a series.
Selective Nerve Root Block
Cervical selective nerve root block is a diagnostic procedure. If a patient has substantial decrease in pain with image-guided contrast-enhanced injection of anesthetics at a specific nerve root, the clinician can consider that specific nerve root to be the main cause of arm pain. Surgeons use such information to plan for surgical management of radiculopathy [24]. Selectivity of such injection is lost if there is epidural spread of the injectate. Some interventional practitioners use particulate steroids when performing a selective nerve root block to treat cervical radicular pain. Given the probability of vascular injection of steroid in this technique and potential catastrophic complications (brain and spinal cord infarction), clinicians should carefully gauge the benefit versus risk when choosing transforaminal epidural injection as a treatment for their patients [25,26]. Use of digital subtraction imaging and nonparticulate steroids is encouraged. Like all interventions, this procedure should be done by fellowship-trained physicians.
Surgery
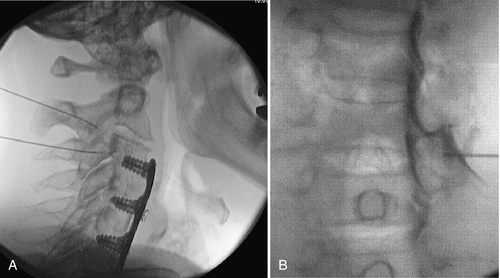
Progressive neurologic deficit, development of myelopathy, and failed conservative care are indications for spinal surgery. Surgical intervention has been shown to provide faster improvement in pain, sensory disturbance, and muscle strength at 3 months postoperatively than conservative treatment [27]. It is not clear from the evidence that long-term outcomes are improved with the surgical treatment of cervical radiculopathy compared with nonsurgical measures [28]. It is not evident that one open surgical technique is clearly superior to others for radiculopathy [28]. Decision-making for discectomy alone or discectomy and fusion with or without foraminotomy is affected by the degree of anatomic change, previous spine surgery, existence of instability, coexisting spondylolisthesis, amount of neck pain in addition to arm pain, and preference of the surgeon. Fusion can be achieved anteriorly (anterior cervical discectomy and fusion) (Fig. 5.6) or posteriorly (posterior cervical fusion). Disc arthroplasty is a newer technique for management of cervical disc diseases; it maintains segmental height and motion. These devices have been shown to have efficacy similar to that of anterior cervical discectomy and fusion [29].
Potential Disease Complications
Possible complications of cervical radiculopathy are persistent or progressive neurologic weakness, residual neck or radicular pain, chronic pain syndrome, disability, and myelopathy (rare, usually associated with spondylosis or large central disc herniation).
Potential Treatment Complications
Medications used to treat cervical radiculopathy can result in class-specific side effects. Nonsteroidal anti-inflammatory drugs commonly have gastrointestinal and renal side effects. Muscle relaxants, selective norepinephrine reuptake inhibitors, and tricyclics can cause central nervous system suppression. Steroids result in endocrine side effects, including hyperglycemia, hypothalamus-pituitary-adrenal axis impact, and amenorrhea. Narcotics can cause nausea, constipation, respiratory suppression, mental status changes, and suppression of endogenous opioids; dependence, tolerance, and abuse may also result.
Manipulation may exacerbate symptoms. Although rare, progressive weakness, carotid dissection, and recurrence of herniation have been reported in connection with cervical spine manipulation [30].
Interventional injections may result in transient increased pain, facial flushing, hyperglycemia, allergic reaction to injectate, and vasovagal reaction. Vasovagal reaction is the most common minor complication [31]. Infection, nerve injury, vascular insult, epidural hematoma, and spinal cord injury are rare but more serious complications that may occur after such invasive procedures. Experienced interventionalists can limit such complications by exercising sterile technique, performing image-guided contrast-enhanced procedures, and withholding anticoagulants and antiplatelets before elective procedures. Cervical transforaminal steroid injection carries the additional risk of vascular injection of steroid, which may lead to brain and spinal cord infarction due to the embolic phenomenon of particulate steroids [26]. Use of digital subtraction imaging and nonparticulate steroids may reduce such risk [32]. Interventional spine procedures should be performed only by fellowship-trained physicians specifically trained in such procedures.
Acknowledgment
The author would like to acknowledge Dr. Asif Jillani for his assistance with this chapter.







