Procedure 49 Open Reduction and Internal Fixation of Phalangeal Shaft Spiral or Long Oblique Fractures
Indications
Examination/Imaging
Surgical Anatomy
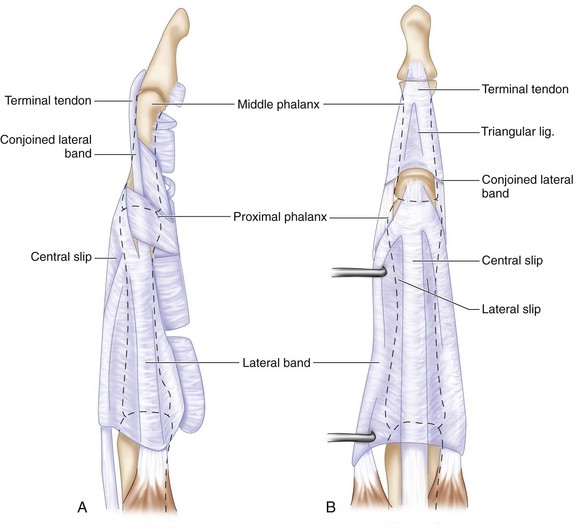
 The extensor tendons, consisting of both the extrinsic and intrinsic tendons, form a finely balanced complex over the finger (Fig. 49-3A).
The extensor tendons, consisting of both the extrinsic and intrinsic tendons, form a finely balanced complex over the finger (Fig. 49-3A).
 The central slip inserts to the base of the middle phalanx, and care should be taken not to violate this insertion during exposure.
The central slip inserts to the base of the middle phalanx, and care should be taken not to violate this insertion during exposure.
 The fibrous flexor sheath with its flexor tendons is closely applied to the volar surface of the phalanges (Fig. 49-3B). Hence, all screws must not protrude beyond the cortex, especially on the volar aspect, to avoid attrition of the flexor tendons.
The fibrous flexor sheath with its flexor tendons is closely applied to the volar surface of the phalanges (Fig. 49-3B). Hence, all screws must not protrude beyond the cortex, especially on the volar aspect, to avoid attrition of the flexor tendons.
Exposures
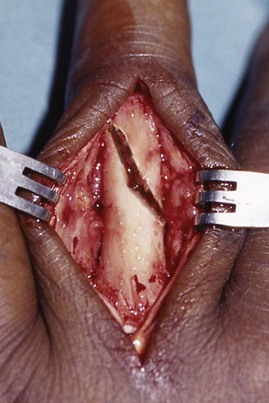
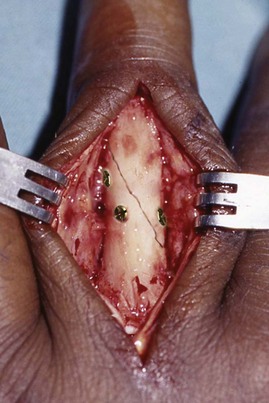
 For the proximal phalanx, the fracture is exposed through a direct dorsal longitudinal incision, splitting the extensor tendon in the midline (Fig. 49-4).
For the proximal phalanx, the fracture is exposed through a direct dorsal longitudinal incision, splitting the extensor tendon in the midline (Fig. 49-4).
 For the middle phalanx, the fracture is exposed through a direct dorsal longitudinal incision, and the lateral slips of the extensor tendon are mobilized by incising the triangular ligament in the midline and extending distally by splitting the tendon in the midline to its insertion into the distal phalanx.
For the middle phalanx, the fracture is exposed through a direct dorsal longitudinal incision, and the lateral slips of the extensor tendon are mobilized by incising the triangular ligament in the midline and extending distally by splitting the tendon in the midline to its insertion into the distal phalanx.
 The periosteum is incised and elevated. This layer is more prominent if fracture repair is delayed by a few days.
The periosteum is incised and elevated. This layer is more prominent if fracture repair is delayed by a few days.
Procedure
Step 1
Step 2
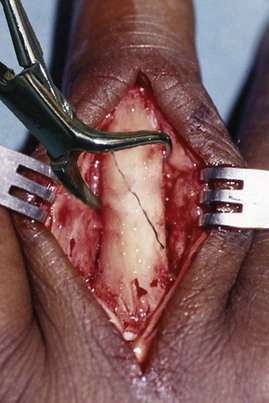
 A small, pointed bone reduction clamp is used to hold the fracture in position (Fig. 49-5). Sometimes, two clamps are required to control rotation.
A small, pointed bone reduction clamp is used to hold the fracture in position (Fig. 49-5). Sometimes, two clamps are required to control rotation.
Step 3
 Precompression of the fracture is achieved by using the pointed bone reduction clamp or artery forceps. This allows a bicortical screw to be inserted instead of a classic lag screw without compromising the compression across the fracture.
Precompression of the fracture is achieved by using the pointed bone reduction clamp or artery forceps. This allows a bicortical screw to be inserted instead of a classic lag screw without compromising the compression across the fracture.
 Usually, a 1.5- or 1.3-mm screw is chosen, according to the size of the bone and fragment. Sometimes, for very small fragments, 1-mm screws may be used. Alternatively, for larger bones, 2-mm screws may be used. There should be at least a one-diameter distance from the edge of the fracture to the drill hole.
Usually, a 1.5- or 1.3-mm screw is chosen, according to the size of the bone and fragment. Sometimes, for very small fragments, 1-mm screws may be used. Alternatively, for larger bones, 2-mm screws may be used. There should be at least a one-diameter distance from the edge of the fracture to the drill hole.
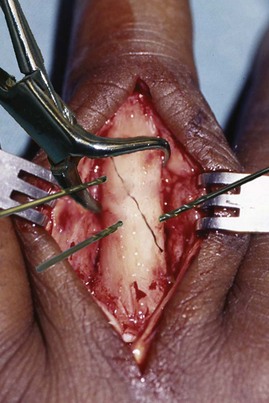
 The direction of the screw should be perpendicular to the fracture line for maximal compression. Screws should also be placed perpendicular to the rotational plane of the fracture (Fig. 49-6).
The direction of the screw should be perpendicular to the fracture line for maximal compression. Screws should also be placed perpendicular to the rotational plane of the fracture (Fig. 49-6).
 The fracture is held in a precompressed position while the drill hole is made. With precompression, the fracture is not likely to slide and displace during tightening of the screws.
The fracture is held in a precompressed position while the drill hole is made. With precompression, the fracture is not likely to slide and displace during tightening of the screws.
Step 3 Pearls
Precompression helps to interdigitate the fracture to lessen the risk for fracture displacement during screw placement.
Smaller screws should be used nearer the apex of the fracture fragments to lessen the risk for fractures.
Ensure that the drill is sharp and that irrigation is done during drilling to reduce the amount of heat produced and the risk for osteonecrosis.
Step 4
 The drill hole is countersunk so that the screw head will sit better. This will also lessen soft tissue irritation as well as ensuring that the direction of the screw is maintained, preventing the screw head from being pushed eccentrically when one side of it comes into contact with the phalanx, as is usually the case with a spiral or long oblique fracture.
The drill hole is countersunk so that the screw head will sit better. This will also lessen soft tissue irritation as well as ensuring that the direction of the screw is maintained, preventing the screw head from being pushed eccentrically when one side of it comes into contact with the phalanx, as is usually the case with a spiral or long oblique fracture.
Step 5
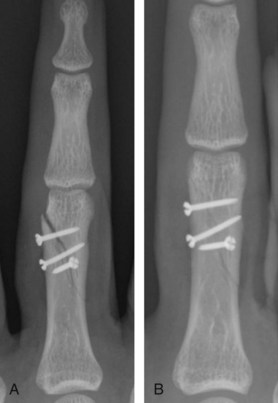
 A minimum of two, and, if possible, three, such screws are inserted, each perpendicular to the rotational plane of the fracture (Fig. 49-7).
A minimum of two, and, if possible, three, such screws are inserted, each perpendicular to the rotational plane of the fracture (Fig. 49-7).
 The fixation is checked using the mini C-arm to confirm the reduction, positioning, and length of the screws as well as the stability through the full range of motion of the finger.
The fixation is checked using the mini C-arm to confirm the reduction, positioning, and length of the screws as well as the stability through the full range of motion of the finger.
Step 5 Pitfalls
The screw length must be perfect. If too long, it may impinge on the flexor tendons. If too short, the fixation will become unstable.
The direction of the screw during insertion must be correctly aligned with the drill hole. Otherwise, the screw will push the distal cortex away and cause a loss of reduction of the fracture (Fig. 49-8A). Figure 49-8B shows screws readjusted with effective interfragmentary compression.
Postoperative Care and Expected Outcomes
 Immediate active assisted range-of-motion exercises are started.
Immediate active assisted range-of-motion exercises are started.
 Sutures are removed at 12th to 14th postoperative day.
Sutures are removed at 12th to 14th postoperative day.
 Fracture healing is monitored at 2-, 6-, and 12-week intervals with radiographs.
Fracture healing is monitored at 2-, 6-, and 12-week intervals with radiographs.
 Progression to passive range-of-motion exercises and strengthening are started as the fracture heals.
Progression to passive range-of-motion exercises and strengthening are started as the fracture heals.
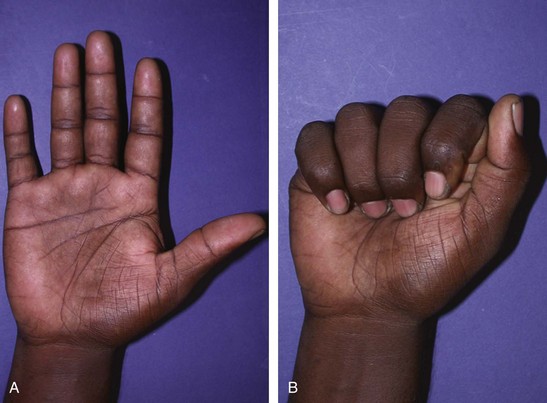
 Figure 49-9: Good range of motion of the middle finger is achieved.
Figure 49-9: Good range of motion of the middle finger is achieved.
Black DM, Mann RJ, Constine RM, Daniels AU. The stability of internal fixation in the proximal phalanx. J Hand Surg [Am]. 1986;11:672-677.
Ford DJ, el-Hadidi S, Lunn PG, Burke FD. Fracture of phalanges: results of internal fixation using 1.5 mm and 2 mm A.O. screws. J Hand Surg [Br]. 1987;12:28-33.
Kawamura K, Chung KC. Fixation choices for closed simple unstable oblique phalangeal and metacarpal fractures. Hand Clin. 2006;22:287-295.