CHAPTER 47
Lumbar Radiculopathy
Maury Ellenberg, MD; Michael J. Ellenberg, MD
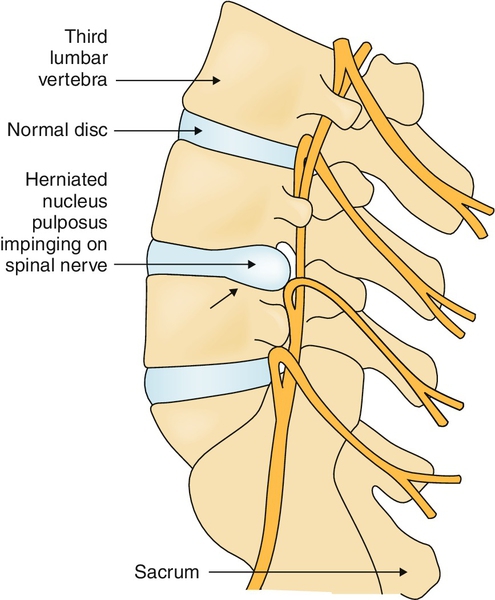
Definition
Lumbar radiculopathy refers to a pathologic process involving the lumbar nerve roots. Lumbar radiculitis refers to an irritation or inflammation of a nerve root. These terms should not be confused with disc herniation, which is a displacement of the lumbar disc from its anatomic location between the vertebrae (often into the spinal canal) (Fig. 47.1). Although lumbar radiculopathy is often caused by a herniated lumbar disc, this is not invariably the case. Many pathologic processes, such as bone encroachment, tumors, and metabolic disorders (e.g., diabetes), can also result in lumbar radiculopathy. It is of utmost significance that disc herniation is often an incidental finding on imaging of the lumbar spine of asymptomatic individuals [1,2]. Therefore, without a clear correlation with the history and physical examination, imaging studies alone can be more misleading than beneficial. When disc herniation results in radiculopathy, the precise cause of the pain is not fully understood. The two possibilities are mechanical compression and inflammation. It has been demonstrated that in a “nonirritated” nerve, mechanical stimulus rarely leads to pain. In contrast, an “irritated” nerve usually results in pain. Furthermore, inflammatory mediators have experimentally been shown to cause radicular pain in the absence of compression [3–5]. It is likely that both factors may be at work individually or together in any given patient. As a result of the imaging findings in asymptomatic individuals and the various causes of pain in radiculopathy, it should be no surprise that disc herniations and nerve root compression can be present in asymptomatic patients [2] and that patients can have radiculopathy without visible disc herniations or nerve root compression [6].
The prevalence of lumbar radiculopathy in the general population varies from 2.2% to 8%, depending on the study, and the incidence ranges from 0.7% to 9.6% [7,8]. One study found a higher incidence in men (67%), with the highest prevalence in individuals 45 to 65 years old [9], and an association with obesity and smoking as well as a correlation with occupations requiring very heavy physical activity.
Symptoms
The most common symptom in lumbar radiculopathy is pain, which may vary in severity and location. The pain may be severe and is often exacerbated or precipitated by standing, sitting, coughing, and sneezing. The location of the pain depends on the nerve root involved, with a great deal of overlap among the dermatomes. Most commonly, S1 radiculopathy produces posterior thigh and calf pain; L5, buttocks and anterolateral leg pain; L4, anterior thigh, anterior or medial knee, and medial leg pain; and L3, groin pain. The patient usually cannot pinpoint the precise onset of pain. Location of pain at onset may be in the back; however, by the time the patient is evaluated, the pain may be present only in the buttocks or limb.
Paresthesias are also common and occur in the dermatomal distribution of the involved nerve root (rarely is the sensory loss complete). On occasion, the patient may present with complaints of weakness. Rarely, there is bladder and bowel involvement, which may be manifested as urinary retention or bowel incontinence.
Physical Examination
The most important elements in the evaluation of lumbar radiculopathy are the history and physical examination [10].
A thorough musculoskeletal and peripheral neurologic examination should be performed. Examine the back for asymmetry or a shift over one side of the pelvis. Evaluate back motion and see whether radicular symptoms (pain radiating to an extremity) in the distribution of the patient’s complaints are produced. In an L5 or S1 radiculopathy, forward flexion of the back while standing is equivalent to a straight-leg raising test and may produce pain in the buttock or posterior thigh. In an L4 or L3 radiculopathy, extension may produce groin or anterior thigh pain.
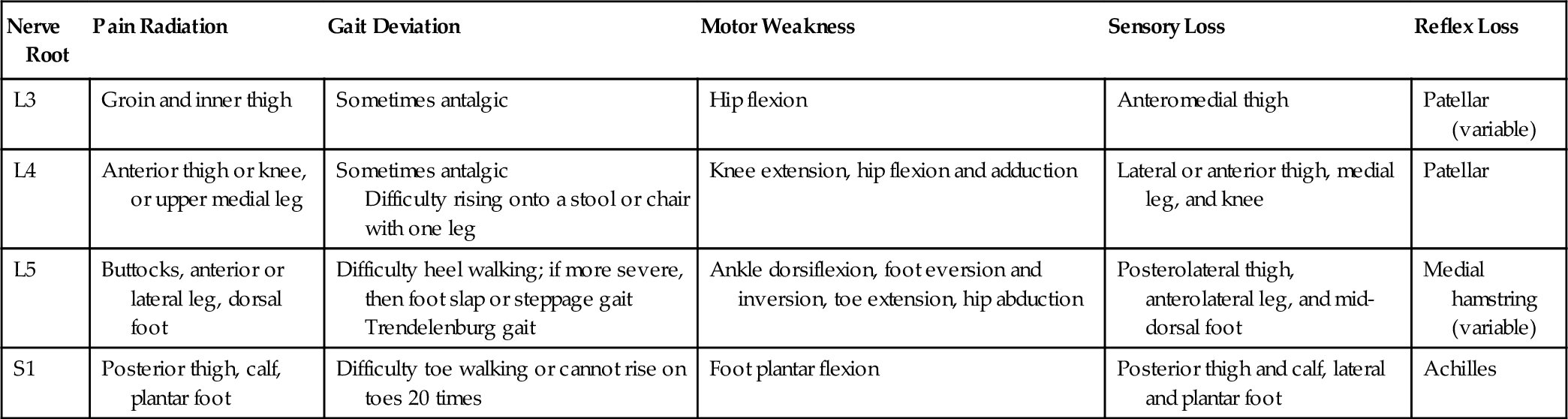
Manual muscle testing is a vital part of the examination for radiculopathy. The major muscle weakness in relation to the nerve root involved is as follows: L3, hip flexors; L4, knee extensors and hip adductors; L5, hip abductors, knee flexors, ankle dorsiflexors, foot evertors, foot inverters, and great toe extensor; S1, ankle plantar flexors (Table 47.1). Try to detect weakness in the distribution of two peripheral nerves arising from the same nerve root. Proximal muscle weakness in the appropriate nerve root distribution is useful in distinguishing bilateral radiculopathy from peripheral neuropathy.
The straight-leg raising test can be performed with the patient sitting or supine. The leg is raised straight up by the examiner, and the test result is positive if the patient complains of pain in the extremity (not the back), typically in a specific nerve root distribution. If pain occurs only in the back, this is not an indicator of radiculopathy and is most often seen with nonspecific low back pain. On occasion, the process of lumbar radiculopathy may start with low back pain, and several days or weeks later, the symptom will occur in the leg. It is possible that the initial process of nucleus pulposus rupture through the anulus may result in the initial back pain, but the pathogenesis is not completely known at this time. Compare side to side to confirm a positive response to the straight-leg raise as opposed to the pain associated with passive hamstring stretch. Rectal examination and perianal and inguinal sensory testing should be done if there is history of bowel or bladder incontinence or retention or recent onset of erectile dysfunction.
Waddell signs are a group of indicators that a nonorganic process is interfering with the accuracy of the physical examination. The signs are superficial—nonanatomic tenderness; simulation—axial loading or rotation of the head causes complaints of back pain; distraction—sitting straight-leg raising versus supine; regional disturbance—weakness or sensory loss in a region of the body that is in a nonanatomic distribution; and overreaction—what is described commonly as excessive pain behavior. These signs are often present in patients with compensation, litigation, or psychoemotional issues [11]. Evaluation for presence of Waddell signs should be a routine part of the examination in patients with pain complaints, particularly if they are long-standing or the history reveals that some of these issues are present.
Functional Limitations
The functional limitations depend on the severity of the symptoms and weakness. Limitations usually occur because of pain but may occasionally occur because of weakness. Standing and walking may be limited, and sitting tolerance is often decreased. Patients with an L4 radiculopathy are at risk of falling down stairs if the involved leg is their “trailing” (power) leg on the stairs. They would also have difficulty ascending stairs or rising from a seated position, depending on the degree of weakness (although that is not as dangerous as descending stairs). Patients with a severe S1 radiculopathy will be unable to run because of calf weakness, even when the pain resolves. Patients with L5 radiculopathy may catch the foot on curbs or, if weakness is severe, on the ground. They may require a brace (ankle dorsiflexion assist). In patients with acute radiculopathy that is severe, the pain will usually preclude them from a whole range of activities—household, recreation, and work. In the majority of patients, once the acute process is ameliorated, they can return to most activities except for heavy household and work activity. After about 3 to 6 months, they can return to all activities unless there is residual weakness, in which case they would be functionally limited as noted before, depending on the radiculopathy level.
Diagnostic Studies
Diagnostic testing takes two forms: one to corroborate the diagnosis and the second to determine the etiology. For simple cases, despite the current “rush toward imaging,” diagnostic testing is usually not needed and the clinical picture can guide the treatment. A history that includes trauma, cancer, bacterial infection, human immunodeficiency virus infection, or diabetes would be an indication for earlier diagnostic testing.
Electromyography
Electromyography and nerve conduction studies, when performed by an individual well versed in the diagnosis of neuromuscular disorders, can be valuable in the diagnosis of lumbar radiculopathy. They can also help with differential diagnoses and in clarifying the diagnosis in patients whose physical examination is not reliable. Electromyography has the advantage over imaging techniques of high specificity, and recordings will rarely be abnormal in asymptomatic individuals [12]. Electrodiagnostic studies, however, do not give direct information about the cause of the radiculopathy.
Imaging
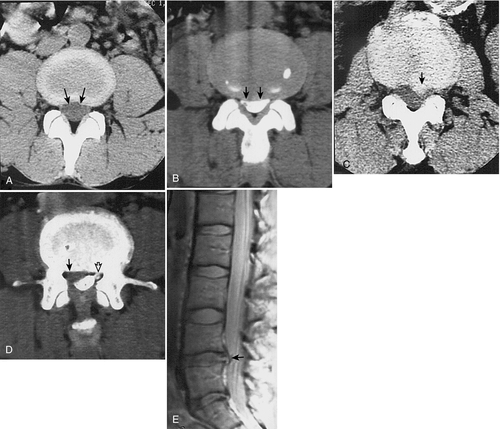
Imaging techniques in relation to lumbar radiculopathy usually refer to lumbosacral spine radiography, computed tomography (CT) scan, and magnetic resonance imaging (MRI).
Plain radiography can be useful to exclude traumatic bone injury or metastatic disease. It allows visualization of the disc space but not the contents of the spinal canal or the nerve roots. CT and MRI allow visualization of the disc, spinal canal, and nerve roots (Fig. 47.2). There is a high incidence of abnormal findings in asymptomatic people, with rates of disc herniation ranging from 21% in the 20- to 39-year age group to 37.5% in the 60- to 80-year age group [2]. In fact, in one study, only 36% of asymptomatic individuals had normal discs at all levels. In other words, it is “normal” to have some disc abnormality, which occurs as part of normal aging [1]. To be meaningful, CT and MRI must clearly correlate with the clinical findings. Perform these studies if tumor is suspected or surgery is contemplated. They also may be useful in precisely locating pathologic changes for transforaminal epidural steroid injection. The most accurate study is MRI, and gadolinium enhancement is not needed unless a tumor is suspected or the patient has undergone prior surgery. Gadolinium enhancement is useful postsurgically to distinguish disc herniation from scar tissue.
Treatment
Initial
The treatment goal is to reduce inflammation and thereby relieve the pain and allow resolution of the radiculopathy regardless of the underlying anatomic abnormalities. Bed rest, which had been the mainstay of nonoperative treatment, is now recommended only for symptom control. In previous studies, bed rest has not been shown to have an effect on the final outcome of the disorder [13]. As long as patients avoid aggravating activities or bending or lifting, which tend to increase intradiscal pressure, they can carry on most everyday activities.
Use nonsteroidal anti-inflammatory drugs (NSAIDs) to help reduce inflammation and to provide pain relief. NSAIDs have been shown to be effective in acute low back pain [14]. However, a review that included pooling of three randomized clinical trials using NSAIDs showed no effectiveness over placebo [15]. It is still reasonable to give NSAIDs a short trial in acute lumbar radiculopathy for pain relief, although they will not shorten the course of the disorder. The use of oral steroids remains controversial and has not passed the scrutiny of well-controlled studies, even in acute low back pain. In a recent meta-analysis of the use of NSAIDS, corticosteroids, tricyclic antidepressants, and anticonvulsants, although the pooled data showed no efficacy with any of these medications over placebo in chronic radiculopathy [16], there was one study that found short-term efficacy for gabapentin [17]. There were two studies in patients with acute radiculopathy in which oral corticosteroids seemed to be effective in the short-term treatment of radicular pain [16]. Other medications, such as cyclobenzaprine, metaxalone, methocarbamol, and chlorzoxazone, some of which may have effectiveness in acute low back pain, have not been shown to be effective in acute radiculopathy [18].
Clinically, for acute radiculopathy, there are several options. If the pain is severe, early epidural steroid injection (see the section on procedures) and testing with imaging and electromyography are reasonable. Another option is oral steroids, such as methylprednisolone (Medrol) dose pack, and the use of opioids for short-term pain control. For more chronic radicular pain, it would be reasonable to try anticonvulsants, such as gabapentin, or a combination of gabapentin and a tricyclic antidepressant, such as amitriptyline or nortriptyline. Start treatment with a low dose and titrate up gradually to determine the minimally effective dose.
Opioids may be used for pain relief, although their effectiveness is suboptimal in neuropathic pain, with some suggestion that they should be used only in severe cases [19]. There is no major concern for addiction in acute care of patients who have not demonstrated past addictive behavior. The needs range from none to relatively high doses, such as the equivalent of 60 to 100 mg of morphine (e.g., MS Contin) a day. Start with hydrocodone or oxycodone and titrate up as needed. For more severe pain, use a long-acting opioid, such as oxycodone (OxyContin) or MS Contin, and for breakthrough pain, use a shorter acting opioid, such as hydrocodone, oxycodone, or short-acting morphine. These treatments should be short term to avoid the risks of dependency or addiction. There seems to be no efficacy of opioids versus placebo for symptom relief or decrease in disability in chronic radiculopathy [20].
Rehabilitation
With an acute painful radiculopathy, it is generally best to wait for some of the acute stage to subside before ordering physical therapy. In a longer standing problem, therapy may be the best first approach.
Physical methods are a useful adjunct to the medication treatment. Various methods, which include flexion and extension exercises (often called a lumbosacral stabilization program), have been tried. Whatever method is used, if radicular pain is produced, the exercises should be stopped. After the radiculopathy resolves, the patient should be prescribed a proper exercise regimen to improve flexibility and muscle strength. Lumbar stabilization exercises, core muscle strengthening, and remaining active may be the most effective of the various methods studied carefully in lumbar radiculopathy. One study showed no effectiveness of lumbar traction [21]. Other modalities, such as transcutaneous electrical nerve stimulation, acupuncture, massage, and manipulation, are not well studied with randomized clinical trials in lumbar radiculopathy [6]. Because they are not likely to cause injury, they can be given a short trial. The manipulation should be done cautiously.
Procedures
Epidural steroid injections are beneficial in acute radiculopathy in patients with or without disc herniation [21,22]. The results in chronic radiculopathy are less convincing. The most effective technique and material to be used for epidural steroid injection are controversial [23,24]. Some literature suggests that either steroid preparations or local anesthetics are superior to placebo for long-term effects. Short-term effects, however, favored the steroid group [24,25]. Some studies show that transforaminal epidural steroid injections have a marginally greater improvement in pain scores compared with lumbar epidural steroid injections. However, on the basis of the preferred safety profile, greater procedural comfort of lumbar epidural steroid injections, and nearly equal functional gains of the two procedures, a reasonable clinical approach is to attempt a lumbar epidural steroid injection initially and then, in the absence of significant improvement or resolution in 2 weeks, to attempt a transforaminal epidural steroid injection [22,23].
Whereas the scientific literature shows that the effects of these interventions are relatively short-lived [21,23], the intervention is beneficial because it limits opiate use [23] and referral for surgical management.
These procedures should be performed under fluoroscopic guidance [26]. It is advisable to perform one injection and to re-evaluate the patient in 1 or 2 weeks to determine whether further injections are required. It is not appropriate to perform a “series of three injections.” On the other hand, a maximum of three injections should be performed for any one episode of radiculopathy. It is reasonable to repeat this procedure for recurrent episodes of radiculopathy after 3 to 6 months.
Nonoperative treatment allows resolution of the radiculopathy in up to 90% of cases [15,27,28]. More interestingly, studies have demonstrated that when radiculopathy is the result of disc herniation, the actual herniation will resolve in the majority of cases, and even when the herniation remains, the symptoms often will still abate [29–31].
Surgery
Surgery is appropriate under two conditions. First, surgery is performed on an emergency basis when a patient presents with a central disc herniation with bowel and bladder incontinence or retention and bilateral lower extremity weakness. In this very rare condition, a neurosurgeon or orthopedic spine surgeon must be consulted immediately and the patient operated on, preferably within 6 hours. Second, surgery is an option if a patient continues to have pain that limits function after an adequate trial of nonoperative treatment.
Patient selection is extremely important to achieve a good surgical outcome. The best outcomes occur in patients with single-level root involvement; with pain experienced more in the limb than in the back; and when an anatomic abnormality on imaging corresponds to the patient’s symptoms, physical examination findings, and electromyographic findings in patients without psychological or secondary gain issues [32,33].
A recent update of a Cochrane review on the subject of surgery versus conservative care concluded that in selected patients, surgery can provide faster relief, but there remains no convincing evidence of a difference in long-term outcomes [34].
The type of surgery depends on the cause of the radiculopathy. For cases of disc herniation, simple laminectomy and discectomy suffice; there seems to be no difference between the standard, microdiscectomy, and newer minimally invasive procedures on outcome or time to return to activity [35]. Fusion should be avoided in these instances. With spinal stenosis, a more extensive laminectomy with foraminotomy may be needed. Fusion should be reserved for the relatively infrequent case of well-demonstrated spinal instability together with radiculopathy or if the surgical procedure will result in spinal instability. One study [36] suggested that fusion is needed in the case of spondylolisthesis, but this has not been confirmed with any randomized clinical trials.
Potential Disease Complications
Complications relate to involvement of the nerve roots in the cauda equina. The most serious is the “paraplegic disc.” In this case, the herniated disc can cause paralysis, but this is very rare. More common, but still unusual, is a disc that causes lower limb weakness and involvement of bowel and bladder function. Residual lower limb weakness may occur either spontaneously or after surgery. Patients may progress to a chronic low back pain syndrome; this is particularly likely to occur in patients with secondary gain issues.
Potential Treatment Complications
NSAIDs can cause gastrointestinal bleeding, mouth ulcers, and renal and hepatic complications. Newer cyclooxygenase 2 inhibitors may avoid gastrointestinal bleeding. There have been associations attributed to the use of cyclooxygenase 2 inhibitors and other NSAIDs with cardiovascular disease. These medications should always be used cautiously, in proper doses, and for limited periods.
Corticosteroids, when used long term, have myriad complications, including weight gain, fat redistribution, osteoporosis, and diabetes mellitus, among others. The short-term use should cause few complications in healthy individuals. Those with diabetes will experience a rise in blood glucose concentration, and some patients may experience mental and emotional difficulties that can include psychosis. Steroids may also lead to gastrointestinal bleeding.
Use of opioids can lead to dependency in some patients. Although they may be of use in patients with lumbar radiculopathy, their use with low back pain and chronic nonmalignant pain, in which effectiveness is questionable [37], has led to an epidemic of the use and abuse of these drugs [38,39].
Epidural steroid injections can (rarely) result in epidural abscess and epidural hematoma. Patients should not take aspirin for 7 days before the injection. Some centers recommend that NSAIDs not be taken for 3 to 5 days before the procedure, although there is no literature documenting an increased incidence of bleeding complications from epidural or spinal injections when patients are taking NSAIDs. Warfarin should be discontinued, and if in doubt, the international normalized ratio should be checked. Clopidogrel (Plavix) and similar antiplatelet agents should be discontinued for a week before injection. The injection can produce local pain, and if it is performed without fluoroscopy, it can often result in spinal headache from piercing of the dura and a resultant spinal fluid leak. This occurs considerably less often when fluoroscopic guidance is used. Contamination of injectable material from a compounding pharmacy, has led to central nervous system infections, primarily with Exserohilum rostratum, and Aspergillus. Twenty-two other pathogens have also been identified. As of June 2013 this has resulted in 745 confirmed infections and 58 deaths. Currently the scope of regulatory oversight within the compounding industry is under review [40].
Surgical complications include infection, nerve root injury, paralysis, local back pain, and the usual postoperative complications (e.g., thrombophlebitis, bladder infection). More serious surgical complications include nerve root or cauda equine injury, arachnoiditis, and post-laminectomy pain syndromes. These complications may lead to repeated surgery, which may be more extensive.