CASE 47



History: A patient presents with chest pain.
1. What are the causes of acute aortic syndrome? (Choose all that apply.)
B. Aneurysm
D. Dissection
2. What is the most likely diagnosis?
C. Aneurysm
D. Dissection
3. What complication does this patient have?
4. What is the most appropriate management of this patient?
A. No treatment
B. Antihypertensive medication
D. Surgery
ANSWERS
References
Chin AS, Fleischmann D. State-of-the-art computed tomography angiography of acute aortic syndrome. Semin Ultrasound CT MR. 2012;33(3):222–234.
Reddy GP, Gunn M, Mitsumori LM, et al. Multislice CT and MRI of the thoracic aorta. In: Webb WR, Higgins CB, eds. Thoracic Imaging: Pulmonary and Cardiovascular Radiology. ed 2 Philadelphia: Lippincott Williams & Wilkins; 2010.
Cross-Reference
Cardiac Imaging: The REQUISITES, ed 3, pp 378–387.
Comment
Acute Aortic Syndrome
Acute aortic syndrome is suspected in the setting of hypertension and chest pain radiating to the back. Acute aortic syndrome can be caused by aortic dissection, intramural hematoma, and penetrating aortic ulcer.
Etiology and Development
Aortic dissection is a separation of the aortic wall that results from intimal disruption. Blood can enter the aortic wall through a tear in the intima, extending proximally and distally in the media, displacing the intima inward. Typically, blood flows in both the true and the false lumina, although the false channel is sometimes thrombosed. The most common predisposing factor for aortic dissection is hypertension. Other etiologies include annuloaortic ectasia (which is associated with connective tissue disorders such as Marfan syndrome or Ehlers-Danlos syndrome), bicuspid aortic valve, aortic aneurysm, and arteritis.
Classification, Complications, and Management
Aortic dissection can be classified as Stanford type A (involving the ascending aorta) or type B (not involving the ascending aorta). The DeBakey classification system identifies three types of dissection: type I involves the ascending aorta and extends into the descending aorta; type II involves the ascending aorta only; and type III involves the descending aorta only, beyond the origin of the left subclavian artery. There are four major life-threatening complications of type A dissection: dissection of the coronary arteries resulting in myocardial infarction, dissection of the carotid arteries resulting in stroke, pericardial hemorrhage causing tamponade, and aortic valve rupture resulting in acute aortic regurgitation. Because of these potential complications, patients with type A dissection are usually treated surgically, with an ascending aortic graft. If the aortic valve is abnormal, the valve is replaced. In contrast, type B dissection usually can be managed medically, including the use of antihypertensive medications.
Imaging
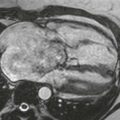
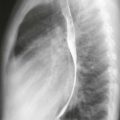
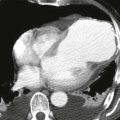
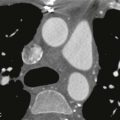
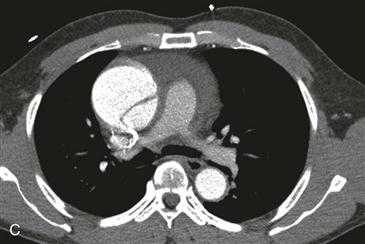
Radiography can demonstrate aortic enlargement (Fig. A) and displacement of calcification; it has relatively low sensitivity and specificity for aortic dissection. CT has high accuracy for the diagnosis of aortic dissection and its complications (Figs. B–D). MRI has similar accuracy and can serve as an alternative imaging modality, especially when CT is contraindicated or in the setting of a chronic dissection. Transesophageal echocardiography (TEE) can be useful but may have lower specificity than CT or MRI. Even when it is not used to establish the diagnosis, TEE is often performed preoperatively to assess the status of the aortic valve.