CHAPTER 45
Lumbar Degenerative Disease
Michael K. Schaufele, MD; Jordan L. Tate, MD, MPH
Definition
Degeneration of the anatomic structures of the lumbar spine is a process associated with aging. Degenerative processes may affect several anatomic structures, resulting in different clinical syndromes, or may be entirely asymptomatic. Approximately one third of asymptomatic and one half of symptomatic younger adults show degenerative changes on lumbar spine magnetic resonance imaging [1,2]. At ages older than 60 years, degenerative changes are found in more than 90% of adults [3]. Degeneration may be accelerated in patients with previous trauma or injury to the lumbar spine. Factors such as diabetes mellitus, smoking, and obesity have been associated with increased rates of lumbar spine degeneration. L4-L5 and L5-S1 are the most commonly involved lumbar levels, given that they undergo the greatest torsion and compressive loads during activity. There has not been a proven gender predominance; however, some studies suggest that disc degeneration may affect more men, whereas facet arthropathy may be more prevalent in women [4]. Genetic factors have been suggested to play a major role in determining presence and extent of spine degeneration [5]. Twin studies have shown heritabilities ranging from 52% to 68% for various lumbar disc degeneration phenotypes [6].
The intervertebral disc experiences progressive dehydration as part of the normal aging process. In certain patients, fissures in the anulus fibrosus may develop, causing an inflammatory response. Nociceptive pain fibers may grow into these fissures [7]. Further degeneration may result in progression of the disease or complete annular tears, which may be the source of discogenic low back pain, also referred to as internal disc disruption syndrome. Up to 39% of patients with chronic low back pain may suffer from internal disc disruption [8]. The loss of segmental integrity may lead to further degeneration of the disc, which results in narrowing of the intervertebral disc space. Because of increased loads on the posterior elements, facet degeneration may develop.
The facet (zygapophyseal) joints and sacroiliac joints, like other synovial joints in the body, may develop osteoarthritis [9].
Facet arthropathy may be an independent or concurrent source of low back pain. Further disc degeneration and subsequent loss of disc height may cause subluxation of the facet joints, resulting in degenerative spondylolisthesis, most commonly at the L4-L5 level [10].
Other conditions seen with lumbar degeneration include spondylosis deformans and diffuse idiopathic skeletal hyperostosis. Spondylosis deformans is a degenerative condition marked by formation of anterolateral osteophytes and is mainly a radiologic diagnosis. In spondylosis deformans, the intervertebral spaces are usually well preserved, unlike in degenerative disc disease. The initiating factor in the development of this condition may be degeneration of the anulus fibrosus, primarily in the anterolateral disc space [11]. Spondylosis deformans may become clinically symptomatic if excessive osteophyte formation leads to neural compression, such as in spinal stenosis. Diffuse idiopathic skeletal hyperostosis involves ossification of the ligamentous attachments to the vertebral bones (entheses). Radiologic features consist of multilevel excessive anterior osteophyte formation. Diffuse idiopathic skeletal hyperostosis affects 5% to 10% of patients older than 65 years [12]. This diagnosis is typically an incidental finding on radiologic studies [13].
Other factors associated with lumbar degeneration include environmental, occupational, and psychosocial influences. Environmental influences include cigarette smoking and occupational activities that involve repetitive bending and prolonged exposures to stooping, sitting, or vibrational stresses. These repetitive actions may result in degeneration of the lumbosacral motion segments [12]. Psychosocial factors are well known to contribute to significant disability in low back pain, often in patients with only minimal structural impairment [14].
Symptoms
Lumbar degenerative symptoms range from minor to debilitating. Common complaints include chronic back pain and stiffness. Patients may also report limited range of motion, especially with extension in the case of facet arthropathy or spinal stenosis. Pain with lumbar flexion, coughing, sneezing, or Valsalva maneuver is often associated with disc disease. Should the degenerative changes result in compression of neural structures, patients may develop radicular symptoms into the leg. This can be seen in conditions such as lumbar disc herniations and spinal stenosis.
Lumbar degenerative disease is probably entirely asymptomatic in the majority of cases. Approximately one third of subjects have substantial abnormalities on magnetic resonance imaging despite being clinically asymptomatic [1]. Because of factors not well understood, such as leakage of inflammatory factors from the disc, a chronic pain syndrome may develop in some patients, possibly from repetitive sensitization of nociceptive fibers in the anulus fibrosus [15].
Clinicians should inquire about atypical symptoms of back pain, including night pain, fever, and recent weight loss. These may lead to the diagnosis of malignant neoplasm or infection.
Clinicians should also inquire about symptoms of chronic pain, including sleep disturbances and depression.
Physical Examination
The purpose of the physical examination is to direct further evaluation and therapy toward one of the five most common sources of low back pain: discogenic, facet arthropathy or instability, radiculopathy or neural compression, myofascial or soft tissue, and psychogenic. Combinations of these sources of back pain often exist. A diagnosis based on physical findings will allow the use of advanced diagnostic tests and therapeutic options in the most cost-effective approach.
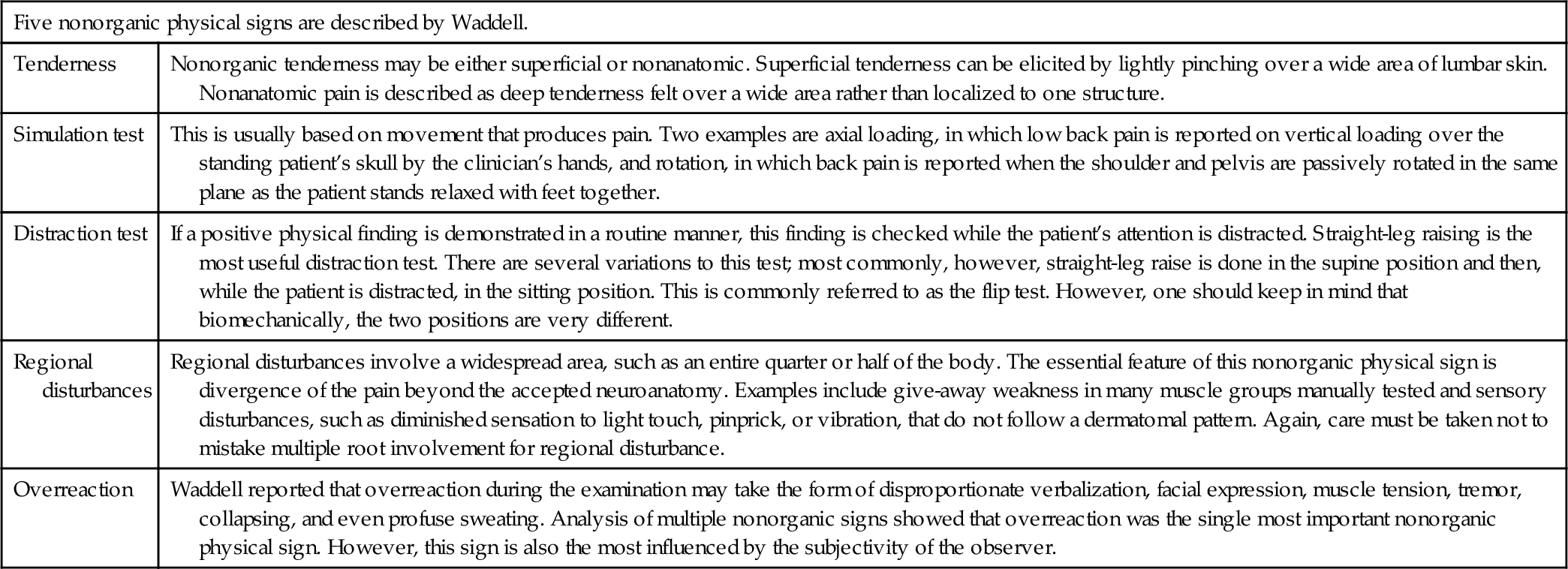
A standardized low back examination should include assessment of flexibility (lumbosacral flexion, extension, trunk rotation, finger-floor distance, hamstring and iliopsoas range of motion, and hip range of motion). An inclinometer (Fig. 45.1) may assist in standardizing lumbar range of motion measurements [16]. A complete examination includes inspection of lower extremities for atrophy and vascular insufficiency, muscle strength testing, and assessment for sensory abnormalities and their distribution. It is important to note asymmetries in deep tendon reflexes (patellar tendon [L4], hamstring tendon [L5], and Achilles tendon [S1]), which may be the most objective finding. Upper motor neuron signs, such as Babinski and ankle clonus, should also be tested. Functional strength testing should include heel to toe walking, calf and toe raises, single-leg knee bends, and complete gait evaluation. Specific testing for lower back syndromes includes straight-leg raising, femoral stretch sign, dural tension signs, and sacroiliac joint provocative maneuvers (e.g., FABER, Gillet, Yeoman, and Gaenslen tests) as well as specific evaluation techniques, such as the McKenzie technique. Assessment of the patient for nonorganic signs of back pain (Waddell signs; Table 45.1) will help the clinician to recognize patients in whom psychological factors may contribute to the pain syndrome [17].

Functional Limitations
Functional limitations in degenerative diseases of the lumbar spine depend on the anatomic structures involved. All aspects of daily living, including self-care, work, sports activities, and recreation, may be affected.
Symptoms are typically exacerbated during bending, twisting, stooping, and forward flexion in patients with primary discogenic pain. Patients with facet arthropathy or instability report increased pain with extension-based activity, including standing and walking. Pain is often relieved with sitting and other similar forward-flexed positions. Patients with myofascial or soft tissue syndromes report pain that is worsened with static and prolonged physical activity. Symptomatic improvement may be associated with rest and modalities including heat, cold, and pressure. Patients with contributing psychological factors, such as depression and somatization disorders, typically report pain out of proportion to the underlying pathologic process, poor sleep, and significant disability in their daily activities.
Diagnostic Studies
Diagnostic testing is directed by the history and physical examination and should be ordered only if the therapeutic plan will be significantly influenced by the results. Anteroposterior and lateral lumbar spine radiographs are helpful for identifying loss of disc height as a result of disc degeneration, spondylosis or osteophyte formation, spondylolisthesis, scoliosis, and facet arthropathy (Fig. 45.2). Oblique views are helpful to identify spondylolysis. Flexion-extension films are necessary to identify dynamic instability and can assist in the selection of appropriate surgical candidates for fusion procedures. Significant degenerative instability usually does not occur before the age of 50 years, but it should be included in the differential diagnosis in patients with clinical symptoms suggestive of advanced facet arthropathy and disc degeneration [11]. Magnetic resonance imaging of the lumbar spine is used because of its sensitivity for identification of abnormalities of the soft tissues and neural structures. It is particularly helpful in identifying various stages of degenerative disc disease as well as annular tears and disc herniation. Other significant sources of back pain, such as neoplasms, osteomyelitis, and fractures, can also be identified with magnetic resonance imaging. Computed tomography is a valuable diagnostic tool in assessing fractures and other osseous abnormalities of the lumbar spine. Computed tomographic imaging in combination with myelography (computed tomographic myelography) aids in presurgical planning by allowing identification of osseous structures causing neural compression, especially in spinal stenosis.

Discography is currently the only technique to correlate structural abnormalities of the intervertebral disc seen on advanced imaging studies with a patient’s pain response. Reproduction of painful symptoms with intradiscal injection of radiopaque contrast material aids in the localization of specific disc levels as pain generators and can be useful in separating painful disc degeneration from painless degeneration. Exploratory studies on blockade of the sinuvertebral nerve, which is thought to carry nociceptive sensation to the intervertebral disc, have been undertaken as an alternative means for diagnosis of discogenic pain [18]. Electrodiagnostic studies may become necessary in cases of peripheral neurologic deficits not clarified by physical examination or imaging. They allow identification of compression neuropathy, radiculopathy, or systemic motor and sensory diseases.
Table 45.2
Pseudospine Pain: Diagnostic Keys
| Condition | Diagnostic Keys | |
| Vascular | Abdominal aortic aneurysm | Older than 50 years Abdominal and back pain Pulsatile abdominal mass |
| Gynecologic | Endometriosis | Woman of reproductive age Cyclic pelvic and back pain |
| Pelvic inflammatory disease | Young, sexually active woman Systemically ill (fever chills) Discharge, dysuria |
|
| Ectopic pregnancy | Missed period Abdominal or pelvic pain Positive pregnancy test result |
|
| Genitourinary | Prostatitis | Men older than 30 years Dysuria Low back and perineal pain |
| Nephrolithiasis | Flank and groin pain Hematuria |
|
| Gastrointestinal | Pancreatitis | Abdominal pain radiating to back Systemic signs (fever, nausea, vomiting) Elevated serum amylase |
| Penetrating or perforated duodenal ulcer | Abdominal pain radiating to back | |
| Rheumatologic | Fibromyalgia | Young to middle-aged woman Widespread pain Multiple tender points Disrupted sleep, fatigue Normal radiographs and laboratory values |
| Polymyalgia rheumatica | Older than 50-60 years Hip or shoulder girdle pain and stiffness Elevated erythrocyte sedimentation rate Dramatic response to low-dose prednisone |
|
| Seronegative spondyloarthropathies (ankylosing spondylitis, Reiter syndrome, psoriatic, enteropathic) | Younger man (ankylosing spondylitis, Reiter syndrome) Lower lumbosacral pain Morning stiffness (“gel”) Improvement with activity Radiographic sacroiliitis |
|
| Diffuse idiopathic skeletal hyperostosis (Forestier disease) | Older than 50-60 years Thoracolumbar stiffness or pain Flowing anterior vertebral calcification |
|
| Piriformis syndrome | Buttock and leg pain Pain on resisted hip external rotation and abduction Transgluteal or transrectal tenderness |
|
| Scheuermann kyphosis | Age 12-15 years Thoracic or thoracolumbar pain Increased fixed thoracic kyphosis 3 or more wedged vertebrae with end-plate irregularities |
|
| Trochanteric bursitis, gluteal fasciitis | Pain or tenderness over greater trochanter | |
| Adult scoliosis | Back pain Uneven shoulders, scapular prominence Paravertebral hump with forward flexion |
|
| Metabolic | Osteoporosis | Woman older than 60 years Severe acute thoracic pain (fracture) Severe weight-bearing pelvic pain (fracture) Aching, dull thoracic pain; relieved in supine position (mechanical) Loss of height, increased thoracic kyphosis |
| Osteomalacia | Diffuse skeletal pain or tenderness Increased alkaline phosphatase |
|
| Paget disease | Bone pain: low back, pelvic, tibia Increased alkaline phosphatase Characteristic radiographic appearance |
|
| Diabetic polyradiculopathy | Older than 50 years Diffuse leg pain, worse at night Proximal muscle weakness |
|
| Malignant neoplasia | Older than 50 years Back pain unrelieved by positional change—night pain Previous history of malignant disease Elevated erythrocyte sedimentation rate |
Modified from Mazanec D. Pseudospine pain: conditions that mimic spine pain. In Cole AJ, Herring SA, eds. The Low Back Pain Handbook. Philadelphia, Hanley & Belfus, 1997.
Treatment
Initial
The most important treatment of any low back pain condition is education and reassurance of the patient. Most of the acute low back symptoms are self-limited and typically resolve within 4 to 6 weeks. The mostly benign nature of degenerative conditions of the spine should be emphasized as well as the fact that acute exacerbations tend to improve over time regardless of therapy. Therapy is directed toward management of the symptoms rather than “cure” of the disease. Initial therapy for lumbar degenerative disease should consist of anti-inflammatory medications, muscle relaxants (Table 45.3), occasionally opioid medications for severe symptom exacerbation, and a functionally oriented physical therapy program. Most patients do well with these measures and do not require any invasive procedures. Other useful initial treatments may include trigger point injections as well as physical modalities such as heat and cold. Low-dose tricyclic antidepressants can help with improvement of sleep.
Table 45.3
Commonly Used Drugs for Muscle Relaxation
| Generic Name | Brand Name | Common Doses |
| Cyclobenzaprine | Flexeril | 5-20 mg po tid |
| Carisoprodol | Soma | 350 mg po tid |
| Baclofen | Lioresal | 10-20 mg po q6h |
| Methocarbamol | Robaxin | 500-750 mg po tid |
| Chlorzoxazone | Parafon Forte | 250-500 mg po tid |
| Orphenadrine | Norflex | 100 mg po bid |
| Metaxalone | Skelaxin | 800 mg tid-qid |
Modified from Schofferman J. Medications for low back pain. In Cole AJ, Herring SA, eds. The Low Back Pain Handbook. Philadelphia, Hanley & Belfus, 1997.
Rehabilitation
Rehabilitation of lumbar degenerative disc disease includes a detailed assessment of functional limitations and functional goals for every patient. A full assessment of occupational and leisure activity demands and goals should also be obtained. For example, patients with advanced degenerative disc disease may benefit from early vocational rehabilitation and counseling with the goal of avoiding future occupational disability and surgical procedures.
On occasion, lumbar orthotics are prescribed, but these are generally not thought to be beneficial in the treatment of degenerative low back pain unless there is significant spondylolisthesis or some other specific indication.
Therapy goals focus on normalization of impairments in flexibility, strength, and endurance and should emphasize healthy lifestyle modifications. A basic lumbar stabilization program with a focus on posture, footwear modifications (if necessary), workplace modifications (if appropriate), and general conditioning works for most patients. Modalities such as ultrasound and electrical stimulation can be used for acute low back pain; however, the focus of supervised therapy should be on an active program rather than the passive treatment that modalities provide.
In patients whose condition does not improve with the outlined initial therapeutic measures, a more intensive, functional restoration approach may be helpful. This commonly includes comprehensive physical rehabilitation with psychological support. These programs can be called many things (e.g., comprehensive spine program, chronic pain program, work conditioning program). Although most of these programs are traditionally considered later in the course of degenerative diseases, early referral may be helpful in decreasing related disability [19]. Another common functional rehabilitation technique is the dynamic lumbar stabilization approach [20]. This muscle stabilization program uses static and dynamic postural exercises to improve the patient’s overall function. It includes education about proper body mechanics during activities of daily living, improved extremity strength and endurance, and muscle stabilization through gym training and healthy lifestyle activities. The hallmark of this program is that postural control is attained through pelvic tilting to control the degree of lumbar lordosis in a pain-free range. The program is designed to advance the patient toward increasingly demanding exercises and to incorporate these exercises into activities of daily living. The program progresses through the building of static strength into dynamic stabilization for patients with more physically demanding athletic activities and occupational demands. This program is supported by a home exercise program.
Core strengthening expands on the concept of lumbar stabilization and has become a key component of rehabilitation programs for all patients, not only for athletes. Core stability is the ability of the lumbo-pelvic-hip complex to prevent buckling and to return to equilibrium after perturbation. Although bone and soft tissues contribute, core stability is predominantly maintained by the dynamic function of the trunk musculature. Decreased core stability may predispose to injury, and appropriate training may reduce injury [21,22].
Postoperative rehabilitation should focus on strength retraining with increasing aerobic exercise while maintaining neutral spine alignment. There is no consensus on when to initiate rehabilitation after surgery, but strong evidence exists for enrolling patients in intensive programs within 6 weeks of surgery to improve functional outcomes and rates of return to work [23].
Procedures
Spinal injection procedures have become an increasingly important part of the overall treatment program for lumbar degenerative disease. These procedures have diagnostic, therapeutic, and even prognostic benefits. It is now commonly agreed that injections should ideally be performed with x-ray guidance and contrast enhancement [24]. The most commonly used procedures are epidural steroid injections, which are beneficial primarily for temporary relief of radicular symptoms [25]. Injection techniques, such as the transforaminal approach, ensure that the medication, usually a corticosteroid, is delivered into the anterior epidural space [26]. Theoretically, medication delivery to the anterior epidural space would decrease inflammatory processes in local structures, such as degenerative discs. However, recent meta-analyses have found good evidence for epidural steroid injections for radicular pain but only fair evidence for axial pain. Moreover, studies have suggested that epidural injections with local anesthesia but without steroid have rates of efficacy similar to those of injections with steroid [27]. Facet (zygapophyseal joint) anesthesia can be obtained through injections done intra-articularly or by blocking the innervating nerves (medial branches) to these joints. Intra-articular facet injections may allow temporary pain relief in cases of synovitis and facet joint cysts. Medial branch injections are used to establish the diagnosis of facet-mediated pain by temporary blockade of the supplying nerve branches of the affected joint [28]. Medial branch neurotomies (“facet rhizotomies”) by radiofrequency ablation may provide longer symptomatic relief for patients with clearly identified facet pain [29]. On occasion, intradiscal steroid injections are applied, but their use is debated because intradiscal steroid may cause discitis, progression of disc degeneration, and calcification of the intervertebral disc [30,31].
Minimally invasive intradiscal therapies (e.g., chemonucleolysis, laser, percutaneous disc decompression) have been used since the 1970s with various clinical successes. Treatment techniques including intradiscal electrothermal therapy involve controlled thermal application to the posterior anulus through an intradiscal catheter. Research data show conflicting results about the therapeutic efficacy of these treatment modalities [32]. There are promising biologic agents currently being studied (e.g., bone morphogenetic protein, mesenchymal stem cell, fibrin adhesive, juvenile chondrocytes) for injection into discs that aim to reverse degenerative and inflammatory changes. Animal studies have revealed augmentation of disc height on imaging studies after intradiscal administration of stem cells [33].
Surgery
The surgical indications for degenerative disc disease of the lumbar spine are highly debated and evolving. Some U.S. insurance companies have recently declared lumbar spine fusion surgery to not be medically necessary if the sole indication is degenerative disc disease. Most insurance carriers require prior authorization of lumbar spine fusion and will consider approval for surgery only when intensive nonsurgical therapy, including physical therapy, injection procedures, and semi-invasive procedures, have failed and the patient continues to have functionally limiting pain. Confounding psychological factors and mental disorders should be excluded before any surgical procedure [34]. Current data are incomplete to judge the scientific validity of spinal fusion for low back pain syndromes [35]. However, if the intervertebral disc is clearly identified as the source of low back pain, interbody fusion with excision of the diseased disc appears to have favorable results. In general, surgical options include posterior fusion procedures with or without pedicle screw instrumentation, anterior interbody fusion with or without pedicle screws, and a combination of these procedures. In case of neural compression, additional decompression procedures may be required. Disc arthroplasty (“artificial disc”) became available in the United States after more than a decade of positive experience in Europe [36,37]. The indication for this surgery is chronic low back pain due to symptomatic degenerative disc disease without significant radiographic instability, neural compression, and facet joint arthropathy. Current outcome studies do not show a clear benefit in pain and functional improvement over fusion surgeries, and questions about the longevity of the implants remain.
Recent developments in endoscopic and minimally invasive surgical techniques have expanded surgical management options. Current research maintains insufficient data for firm conclusions to be drawn about the therapeutic efficacy of these surgical techniques [38].
Potential Disease Complications
In general, degenerative lumbar disease is a benign condition. However, increasing functional limitations can occur, especially if advanced segmental degeneration leads to neural compression and symptoms of spinal stenosis, neural claudication, and segmental instability develop. Persistent neurologic deficits from these conditions are rare and can be avoided if the conditions are diagnosed early and appropriate treatment is begun. A small number of patients may develop chronic pain syndromes. Low back pain is the most common cause of the chronic pain syndrome. Not surprisingly, the incidence of mental disorders, such as depression and somatoform disorders, is high, and these disorders commonly respond better to a behavioral psychology approach than to disease-oriented medical treatment approaches. Early detection of patients with mental disorders will help avoid unnecessary medical treatment and allow appropriate psychological and psychiatric interventions.
Potential Treatment Complications
As with any medications, clinicians must be fully aware of their risks and unwanted side effects. Analgesics and nonsteroidal anti-inflammatory drugs have well-known side effects that most commonly affect the gastric, hepatic, and renal systems. Muscle relaxants can cause sedation. Low-dose tricyclic antidepressants can cause sedation and urinary retention in men with benign prostatic hypertrophy. Some patients require chronic opioid therapy, and issues of constipation and dependence arise. Risks associated with spinal injection include cortisone flare, hyperglycemia, dural puncture, and, rarely, hematoma, infection, and neurologic damage. All potential complications should be thoroughly discussed with the patient before treatment. Potential surgical complications, including nerve damage, malpositioned hardware, wound infection, and medical complications (pulmonary embolism, pneumonia, acute kidney injury), will vary with the procedure but can be as high as 17% for lumbar fusion procedures for degenerative disc disease [39].