Procedure 45 Dorsal Ulnar Artery Perforator Flap
Indications
Examination/Imaging
Clinical Examination
 Defect: The flap should be selected for defects that are free of infection. This is determined by looking at the wound bed and the surrounding skin for edema and erythema. This is a low-flow flap that is easily compromised by any residual infection. (Figure 45-3 shows predébridement appearance of the patient in Fig. 45-1.)
Defect: The flap should be selected for defects that are free of infection. This is determined by looking at the wound bed and the surrounding skin for edema and erythema. This is a low-flow flap that is easily compromised by any residual infection. (Figure 45-3 shows predébridement appearance of the patient in Fig. 45-1.)
 Perforator: There should be no injury in the vicinity of the selected perforator. Injuries that may disturb the perforator include ulnar head fractures or lacerations over the distal ulnar forearm with associated tendon, nerve, or vessel injury.
Perforator: There should be no injury in the vicinity of the selected perforator. Injuries that may disturb the perforator include ulnar head fractures or lacerations over the distal ulnar forearm with associated tendon, nerve, or vessel injury.
 Morbidity: This flap may require division of some branches or the main trunk of the dorsal sensory branch of the ulnar nerve. This will result in loss of sensation in the territory of the nerve and, rarely, a painful neuroma. Patients should be informed about these problems before surgery.
Morbidity: This flap may require division of some branches or the main trunk of the dorsal sensory branch of the ulnar nerve. This will result in loss of sensation in the territory of the nerve and, rarely, a painful neuroma. Patients should be informed about these problems before surgery.
Imaging
 A preoperative Doppler assessment of the perforator is essential to identify the location of the perforator. The Doppler probe is moved from distal to proximal along the ulnar border of the forearm beginning at the pisiform and staying ulnar to the flexor carpi ulnaris (FCU). The perforator is located 2 to 6 cm proximal to the pisiform.
A preoperative Doppler assessment of the perforator is essential to identify the location of the perforator. The Doppler probe is moved from distal to proximal along the ulnar border of the forearm beginning at the pisiform and staying ulnar to the flexor carpi ulnaris (FCU). The perforator is located 2 to 6 cm proximal to the pisiform.
Surgical Anatomy
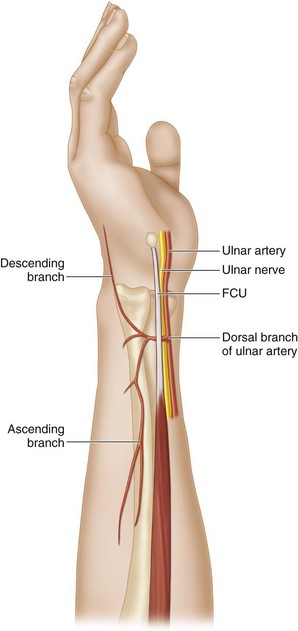
 Vascular basis: The flap is based on a perforator of the ulnar artery that arises 2 to 6 cm proximal to the pisiform. This vessel passes from palmar to dorsal under the FCU tendon and divides into an ascending branch (directed proximally toward the forearm) and a descending branch (directed distally toward the hand). This flap is based on the ascending branch of the dorsal ulnar artery (DUA) (Fig. 45-4). In addition to the ulnar artery perforator, this flap is also nourished by the dorsal carpal arch through its communications with the descending branch.
Vascular basis: The flap is based on a perforator of the ulnar artery that arises 2 to 6 cm proximal to the pisiform. This vessel passes from palmar to dorsal under the FCU tendon and divides into an ascending branch (directed proximally toward the forearm) and a descending branch (directed distally toward the hand). This flap is based on the ascending branch of the dorsal ulnar artery (DUA) (Fig. 45-4). In addition to the ulnar artery perforator, this flap is also nourished by the dorsal carpal arch through its communications with the descending branch.
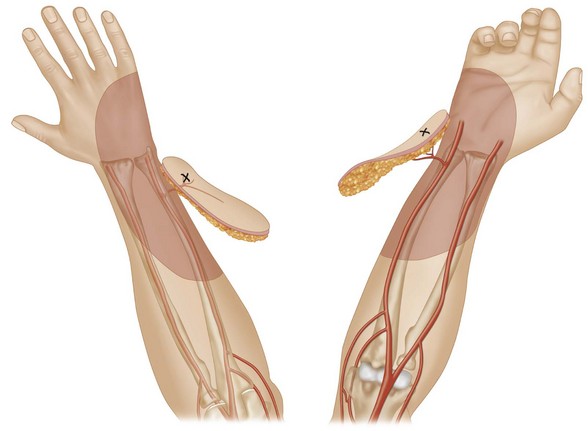
 Limits of the flap: We limit the proximal extent of the flap to the mid-forearm. This results in a 10- to 15-cm long flap, depending on the exact location of the perforator. Selective dye injection studies in cadavers have shown that the staining is limited to the distal third of the forearm skin. The maximum width of the flap is limited to 6 cm because this permits linear closure of the flap donor site. The arc of coverage of the flap is therefore limited to defects within 10 to 15 cm of the perforator (Fig. 45-5).
Limits of the flap: We limit the proximal extent of the flap to the mid-forearm. This results in a 10- to 15-cm long flap, depending on the exact location of the perforator. Selective dye injection studies in cadavers have shown that the staining is limited to the distal third of the forearm skin. The maximum width of the flap is limited to 6 cm because this permits linear closure of the flap donor site. The arc of coverage of the flap is therefore limited to defects within 10 to 15 cm of the perforator (Fig. 45-5).
Exposures
 Flap design: The location of the DUA perforator is determined by Doppler and marked preoperatively. The location of the perforator represents the pivot point of the flap. A line drawn between the pisiform and the medial epicondyle represents the axis of the flap. The distance between the perforator and the proximal edge of the defect represents the bridge segment of the flap. Based on the size of the soft tissue defect, a flap is designed proximal to the perforator at a distance that equals the bridge segment. The flap may be designed as wholly fasciocutaneous, fasciocutaneous with an adipofascial bridge segment, or wholly adipofascial.
Flap design: The location of the DUA perforator is determined by Doppler and marked preoperatively. The location of the perforator represents the pivot point of the flap. A line drawn between the pisiform and the medial epicondyle represents the axis of the flap. The distance between the perforator and the proximal edge of the defect represents the bridge segment of the flap. Based on the size of the soft tissue defect, a flap is designed proximal to the perforator at a distance that equals the bridge segment. The flap may be designed as wholly fasciocutaneous, fasciocutaneous with an adipofascial bridge segment, or wholly adipofascial.
 Flaps with an adipofascial bridge segment can reach the defect by passing the bridge segment under a wide skin tunnel or by laying open the intervening skin segment.
Flaps with an adipofascial bridge segment can reach the defect by passing the bridge segment under a wide skin tunnel or by laying open the intervening skin segment.
Procedure
Step 1
 A 4-cm vertical incision centered on a previously marked perforator is made ulnar to the FCU.
A 4-cm vertical incision centered on a previously marked perforator is made ulnar to the FCU.
 Skin and soft tissue are divided to identify the FCU.
Skin and soft tissue are divided to identify the FCU.
 The FCU is retracted ulnarly to identify the ulnar neurovascular bundle, and the DUA perforator is identified.
The FCU is retracted ulnarly to identify the ulnar neurovascular bundle, and the DUA perforator is identified.
 Based on the location of the perforator, the preoperative flap design is confirmed or modified as required.
Based on the location of the perforator, the preoperative flap design is confirmed or modified as required.
Step 2
 The proximal border of the flap is incised, followed by the lateral borders.
The proximal border of the flap is incised, followed by the lateral borders.
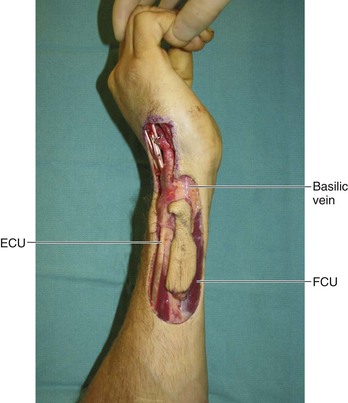
 The flap is elevated in the plane superficial to the epimysium of the FCU and extensor carpi ulnaris (ECU) muscle bellies (Fig. 45-7).
The flap is elevated in the plane superficial to the epimysium of the FCU and extensor carpi ulnaris (ECU) muscle bellies (Fig. 45-7).
Step 2 Pearls
Veins at the lateral borders of the flap are avoided because these veins only add to stasis within the flap. Veins and dorsal sensory nerve branches that pass through the midsubstance of the flap cannot be avoided, are divided, and are included with the flap.
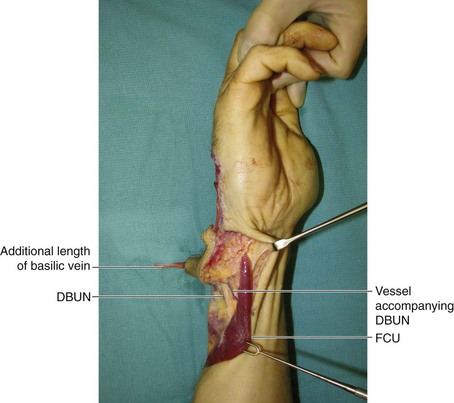
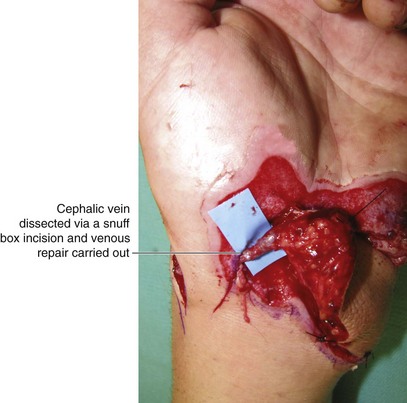
The basilic vein usually travels within the flap. An additional 2 to 3 cm of this vein can be harvested by dissection proximal to the flap margins. This additional length can be used for a venous anastomosis at the recipient site (Fig. 45-8).
Step 2 Pitfalls
The dorsal branch of the ulnar nerve takes off from the ulnar nerve about 5 to 8 cm proximal to the pisiform. Depending on the course of the nerve, it may occasionally be possible to separate the main nerve trunk or some of the branches from the flap.
A large perforator of the ulnar artery travels along with the dorsal branch of the ulnar nerve, but this will need to be ligated to allow the flap movement (see Fig. 45-8).
Step 3
Step 3 Pearls
The flap can be elevated rapidly in the proximal two thirds; however, once the dorsal branch of the ulnar nerve is visualized, elevation should proceed slowly.
A flap designed with a dermoadiposal bridge segment is created by raising thick epidermal skin flaps and keeping the bridge segment as wide as the widest portion of the cutaneous flap.
Step 3 Pitfalls
Although the cutaneous distal portion of the flap in a teardrop design is narrow, one must elevate a wider adipofascial portion to ensure that the cutaneous branches of the perforator are included.
The perforator should not be skeletonized because the connective tissue surrounding the artery contains the draining veins.
Step 5
 The tourniquet is released with the flap in its native position, and the flap is allowed to perfuse for 10 to 15 minutes. This time is used to achieve excellent hemostasis (Fig. 45-9).
The tourniquet is released with the flap in its native position, and the flap is allowed to perfuse for 10 to 15 minutes. This time is used to achieve excellent hemostasis (Fig. 45-9).
Step 5 Pearls
This flap is now dependent only on the perforating vessel for blood supply. Allowing it to perfuse for 10 to 15 minutes gives it time to get accustomed to the new vascular flow pattern.
The pedicle of the flap has to be twisted to allow the flap to reach the defect. This should be done after tourniquet release because an empty vessel is more likely to become kinked than a vessel with flow.
Step 6
 The flap is then rotated into the defect and loosely anchored to the edges of the defect using 5-0 nylon sutures (Fig. 45-11).
The flap is then rotated into the defect and loosely anchored to the edges of the defect using 5-0 nylon sutures (Fig. 45-11).
Step 6 Pearls
Keeping the wrist in slight flexion will decrease the stretch on the pedicle when the flap is used for palmar defects. The wrist can be maintained in extension, if the flap is being used for dorsal defects.
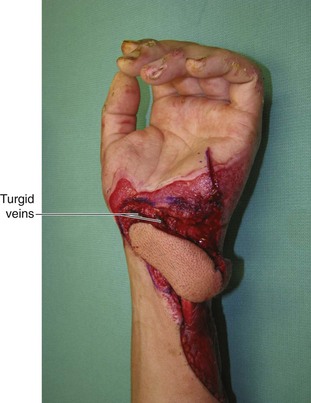
In larger flaps, it may be better to do a venous anastomosis (Fig. 45-10). If a suitable recipient vein cannot be found for anastomosis, one should consider ligating the large superficial vein within the flap at the level of the wrist (distal to the perforator). This will make rotating the flap easier and decrease the venous congestion caused by these veins (Fig. 45-11).
Postoperative Care and Expected Outcomes
 A volar splint is used for 1 week. Patients are discharged on the first postoperative day and advised to keep the limb elevated. They are started on range-of-motion exercises at 1 week, the sutures are removed at 2 weeks, and patients are then allowed to resume normal activities.
A volar splint is used for 1 week. Patients are discharged on the first postoperative day and advised to keep the limb elevated. They are started on range-of-motion exercises at 1 week, the sutures are removed at 2 weeks, and patients are then allowed to resume normal activities.
 The DUA perforator flap is easy to raise and has minimal donor site morbidity. It provides single-stage like-for-like reconstruction (color match, skin thickness, and texture) for dorsal defects. (Figure 45-13 shows the late result of the patient in Figure 45-2.) It has a valuable role in resurfacing palmar defects, especially over the carpal tunnel, although the color match is not very good for palmar coverage. (Figure 45-14 shows the late result of the patient in Figure 45-1.)
The DUA perforator flap is easy to raise and has minimal donor site morbidity. It provides single-stage like-for-like reconstruction (color match, skin thickness, and texture) for dorsal defects. (Figure 45-13 shows the late result of the patient in Figure 45-2.) It has a valuable role in resurfacing palmar defects, especially over the carpal tunnel, although the color match is not very good for palmar coverage. (Figure 45-14 shows the late result of the patient in Figure 45-1.)