Procedure 44 Dorsal Metacarpal Artery Perforator Flap
![]() See Video 36: Dorsal Metacarpal Artery Perforator Flap
See Video 36: Dorsal Metacarpal Artery Perforator Flap
Indications
 Dorsal and lateral finger soft tissue defect proximal to the distal interphalangeal (DIP) joint (Fig. 44-1)
Dorsal and lateral finger soft tissue defect proximal to the distal interphalangeal (DIP) joint (Fig. 44-1)
 Palmar finger soft tissue defect proximal to the DIP joint in patients with injuries to multiple fingers that make it difficult to use local flaps from adjacent digits
Palmar finger soft tissue defect proximal to the DIP joint in patients with injuries to multiple fingers that make it difficult to use local flaps from adjacent digits
 Palmar or dorsal soft tissue defects proximal to the DIP joint in more than one finger
Palmar or dorsal soft tissue defects proximal to the DIP joint in more than one finger
Examination/Imaging
Clinical Examination
 Defect: The flap should be used for defects that are free of infection. This is determined by looking at the wound bed and the surrounding skin for edema and erythema. This is a low-flow flap that is easily compromised by any residual infection.
Defect: The flap should be used for defects that are free of infection. This is determined by looking at the wound bed and the surrounding skin for edema and erythema. This is a low-flow flap that is easily compromised by any residual infection.
 Perforator: There should be no injury in the vicinity of the selected perforator. Injuries that may disturb the perforator include metacarpal neck fractures, lacerations extending into the web space, contusion on the dorsum of the hand, and previous injection of local anesthetic agent. The perforator artery may be intact, but the tenuous venae comitantes are easily injured and can result in flap failure owing to venous congestion.
Perforator: There should be no injury in the vicinity of the selected perforator. Injuries that may disturb the perforator include metacarpal neck fractures, lacerations extending into the web space, contusion on the dorsum of the hand, and previous injection of local anesthetic agent. The perforator artery may be intact, but the tenuous venae comitantes are easily injured and can result in flap failure owing to venous congestion.
 Morbidity: This flap requires division of some dorsal sensory branches during flap elevation. This will result in loss of sensation in the territory of the nerve and, rarely, a painful neuroma. Closure of the flap donor site will result in a visible scar on the dorsum of the hand. Patients should be informed about these problems preoperatively.
Morbidity: This flap requires division of some dorsal sensory branches during flap elevation. This will result in loss of sensation in the territory of the nerve and, rarely, a painful neuroma. Closure of the flap donor site will result in a visible scar on the dorsum of the hand. Patients should be informed about these problems preoperatively.
Imaging
 A radiograph of the hand is useful in patients with a posttraumatic defect to rule out any associated metacarpal neck fractures.
A radiograph of the hand is useful in patients with a posttraumatic defect to rule out any associated metacarpal neck fractures.
 A preoperative Doppler assessment of the perforator is not required. It is difficult to separate the Doppler signals of the perforator from the dorsal metacarpal artery (DMA). In our experience, the perforator is always present, and, if the DMA is absent, the perforator should arise directly from one of the branches of the deep palmar arch.
A preoperative Doppler assessment of the perforator is not required. It is difficult to separate the Doppler signals of the perforator from the dorsal metacarpal artery (DMA). In our experience, the perforator is always present, and, if the DMA is absent, the perforator should arise directly from one of the branches of the deep palmar arch.
Surgical Anatomy
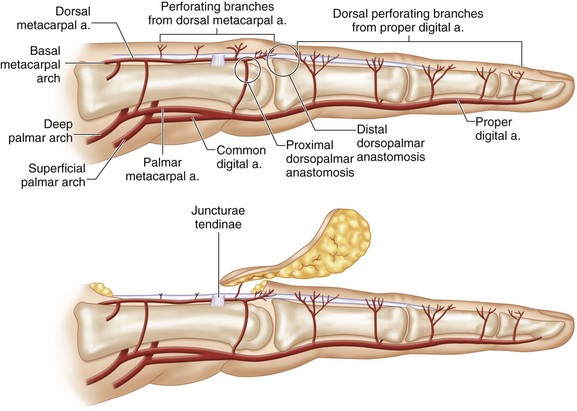
 Vascular basis: The flap is based on the distal cutaneous perforator of the DMA that arises at the level of the metacarpal neck in the second to fourth intermetacarpal spaces. In addition to the DMA, this flap is also nourished by the palmar arterial system through a dorsopalmar anastomosis. This anastomosis is formed by the dorsal perforating branch of the palmar metacarpal artery (arising from the deep palmar arch) and the DMA at the neck of the metacarpal (Fig. 44-2).
Vascular basis: The flap is based on the distal cutaneous perforator of the DMA that arises at the level of the metacarpal neck in the second to fourth intermetacarpal spaces. In addition to the DMA, this flap is also nourished by the palmar arterial system through a dorsopalmar anastomosis. This anastomosis is formed by the dorsal perforating branch of the palmar metacarpal artery (arising from the deep palmar arch) and the DMA at the neck of the metacarpal (Fig. 44-2).
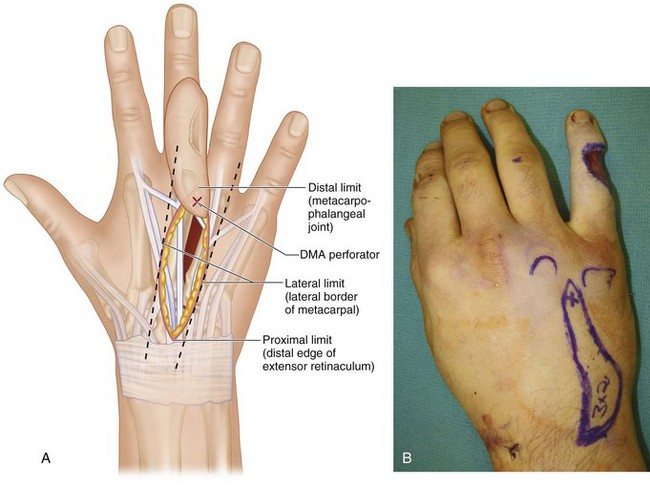
 Limits of the flap: We limit our flaps between the distal edge of the extensor retinaculum, the metacarpophalangeal (MCP) joint, and the outer borders of the adjoining metacarpals (Fig. 44-3A and B).
Limits of the flap: We limit our flaps between the distal edge of the extensor retinaculum, the metacarpophalangeal (MCP) joint, and the outer borders of the adjoining metacarpals (Fig. 44-3A and B).
Exposures
 Flap design: The DMA perforator closest to the defect is marked at the level of the metacarpal neck in the intermetacarpal space. The location of the perforator represents the pivot point of the flap. The distance between the perforator and the proximal edge of the defect represents the bridge segment of the flap. Based on the size of the soft tissue defect, a flap is designed proximal to the perforator at a distance that equals the bridge segment.
Flap design: The DMA perforator closest to the defect is marked at the level of the metacarpal neck in the intermetacarpal space. The location of the perforator represents the pivot point of the flap. The distance between the perforator and the proximal edge of the defect represents the bridge segment of the flap. Based on the size of the soft tissue defect, a flap is designed proximal to the perforator at a distance that equals the bridge segment.
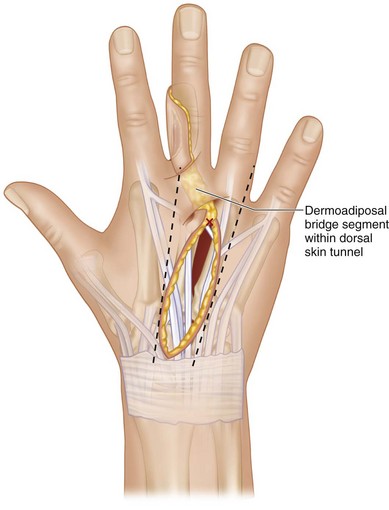
 The flap may be designed as wholly cutaneous, cutaneous with a dermoadiposal bridge segment, or wholly adiposal.
The flap may be designed as wholly cutaneous, cutaneous with a dermoadiposal bridge segment, or wholly adiposal.
 Flaps with a dermoadiposal bridge segment can reach the defect by passing the bridge under a skin tunnel or by laying open the intervening skin segment (Fig. 44-4).
Flaps with a dermoadiposal bridge segment can reach the defect by passing the bridge under a skin tunnel or by laying open the intervening skin segment (Fig. 44-4).
Pearls
We design the skin island in an oblique fashion when a wider flap is required to accommodate a defect that involves two surfaces (palmar + lateral or dorsal + lateral).
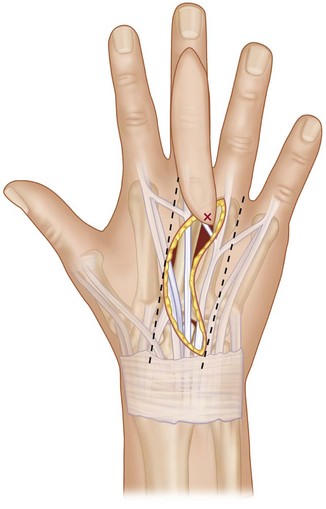
If the flap design extends proximal to the distal edge of the extensor retinaculum, we design the flap as a curved ellipse instead of a straight ellipse. Once the flap is raised, the curved ellipse is straightened out and inset as a straight ellipse. This results in an additional 8 to 10 mm while maintaining the design within the previously mentioned limits (Fig. 44-5).
Procedure
Step 1
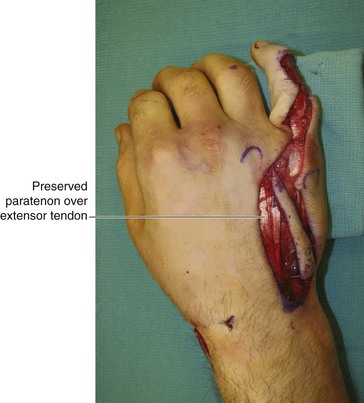
 The skin and subcutaneous tissue on one lateral border of the flap are incised until the underlying extensor tendon is seen (Fig. 44-6).
The skin and subcutaneous tissue on one lateral border of the flap are incised until the underlying extensor tendon is seen (Fig. 44-6).
Step 3
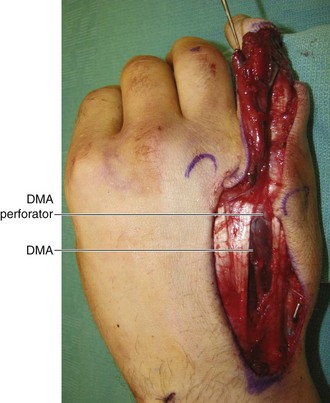
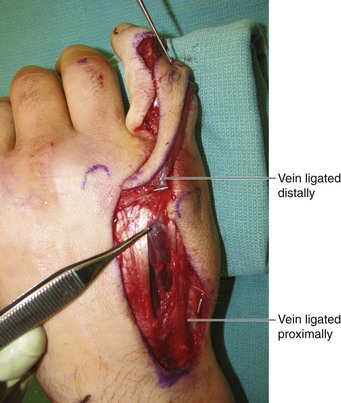
 The remaining lateral border of the flap is incised, and the flap is elevated from proximal to distal (Fig. 44-7).
The remaining lateral border of the flap is incised, and the flap is elevated from proximal to distal (Fig. 44-7).
Step 4
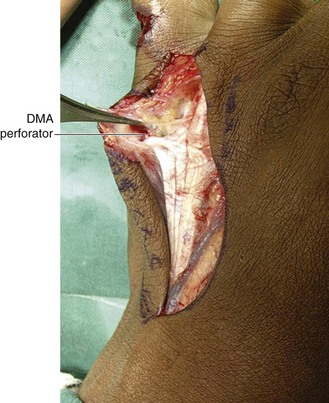
 The DMA perforator is identified, and the flap is incised into an island distal to the perforator (Fig. 44-8).
The DMA perforator is identified, and the flap is incised into an island distal to the perforator (Fig. 44-8).
Step 5
 Any intervening normal skin between the flap and defect can be laid open, or a wide tunnel can be made under it to enable the flap to reach the defect (see Fig. 44-7).
Any intervening normal skin between the flap and defect can be laid open, or a wide tunnel can be made under it to enable the flap to reach the defect (see Fig. 44-7).
Step 5 Pearls
We prefer a tunnel for dorsal defects because the lax dorsal skin permits creation of large tunnels. In addition, this preserves the pliable skin over the dorsum of the MCP joint. For palmar defects, we prefer to lay the tunnel open or use a cutaneous bridge segment because making a tunnel in the palmar skin is difficult, and the constrictive fibrous septae can compromise flap vascularity.
Step 6
 The tourniquet is released with the flap in its native position, and the flap is allowed to perfuse for 10 to 15 minutes. This time is used to achieve excellent hemostasis.
The tourniquet is released with the flap in its native position, and the flap is allowed to perfuse for 10 to 15 minutes. This time is used to achieve excellent hemostasis.
Step 6 Pearls
This flap is now dependent only on the perforating vessel for blood supply. Allowing it to perfuse for 10 to 15 minutes gives it time to get accustomed to the new vascular flow pattern.
The pedicle of the flap has to be twisted to allow the flap to reach the defect. This should be done after tourniquet release because an empty vessel is more likely to get kinked than a vessel with flow.
Step 7
 The flap is then rotated into the defect and loosely anchored to the edges of the defect using 5-0 nylon sutures (Fig. 44-10).
The flap is then rotated into the defect and loosely anchored to the edges of the defect using 5-0 nylon sutures (Fig. 44-10).
Step 7 Pearls
Keeping the proximal interphalangeal (PIP) and MCP joints in extension will decrease the stretch on the pedicle.
When the flap is used to cover lateral or palmar defects, a folded gauze placed between the fingers that is incorporated into the final dressing keeps the web open and prevents compression of the bridge segment.
Postoperative Care and Expected Outcomes
 A volar splint is used for 1 week to keep the fingers and the wrist in extension. Patients are discharged on the first postoperative day and advised to keep the limb elevated. They are started on range-of-motion exercises at 1 week, the sutures are removed at 2 weeks, and patients are then allowed to resume normal activities (Fig. 44-11).
A volar splint is used for 1 week to keep the fingers and the wrist in extension. Patients are discharged on the first postoperative day and advised to keep the limb elevated. They are started on range-of-motion exercises at 1 week, the sutures are removed at 2 weeks, and patients are then allowed to resume normal activities (Fig. 44-11).
 The DMA perforator flap is easy to raise and has minimal donor site morbidity. It is the ideal flap for resurfacing dorsal soft tissue defects because it provides single-stage “like-for-like” reconstruction (color match, skin thickness, and texture). It provides excellent coverage of defects in the web space and the lateral aspect of the fingers, although the color match is not ideal. It has a valuable role in resurfacing palmar defects, especially in cases when multiple fingers are injured, and it is risky to harvest homodigital/heterodigital vascular island flaps or a cross-finger flap. In addition, more than one flap can be raised at the same time, permitting coverage of multiple fingers simultaneously.
The DMA perforator flap is easy to raise and has minimal donor site morbidity. It is the ideal flap for resurfacing dorsal soft tissue defects because it provides single-stage “like-for-like” reconstruction (color match, skin thickness, and texture). It provides excellent coverage of defects in the web space and the lateral aspect of the fingers, although the color match is not ideal. It has a valuable role in resurfacing palmar defects, especially in cases when multiple fingers are injured, and it is risky to harvest homodigital/heterodigital vascular island flaps or a cross-finger flap. In addition, more than one flap can be raised at the same time, permitting coverage of multiple fingers simultaneously.