CASE 44 Crush Stent or Provisional Stenting for Bifurcation Lesion?
Case presentation
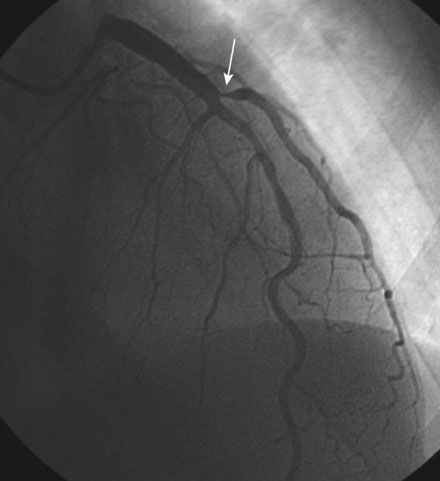
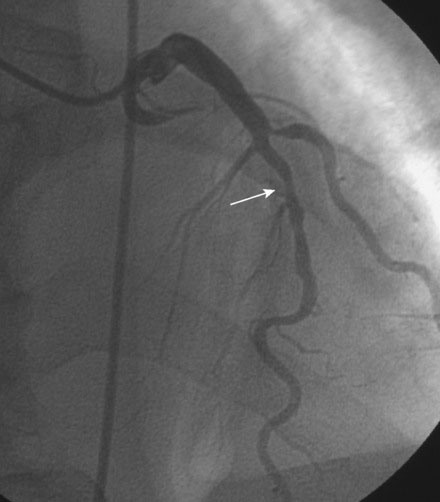
A 52-year-old man with end-stage renal disease, on dialysis for 5 months, developed ventricular tachycardia during vascular access surgery for dialysis. Past history was notable for longstanding and poorly controlled hypertension leading to end-stage kidney disease and a history of systolic heart failure, with an echocardiogram showing global left ventricular dysfunction and ejection fraction of 35% to 40%. He underwent cardiac catheterization 5 months earlier when he first presented with heart failure in the setting of renal failure, and was found to have a normal right coronary artery (Figure 44-1), a normal circumflex system, and moderate disease in the left anterior descending (LAD) artery just after the first septal perforator, but he also had a severe stenosis of the ostium of a large diagonal branch (Figures 44-2 through 44-4 and Video 44-1). Based on this evaluation, his heart failure and systolic dysfunction were thought to be secondary to the renal failure and hypertensive heart disease, with coexisting coronary artery disease. He was treated medically with lisinopril, metoprolol, aspirin, and amlodipine and did well until he developed sustained polymorphic ventricular tachycardia and chest pain during AV fistula graft placement for dialysis. This episode required resuscitation with cardioversion and intubation. Sinus rhythm was restored and subsequent electrocardiograms showed no acute changes but serial troponin I assays were elevated, consistent with a non-ST segment elevation myocardial infarction. He was loaded with clopidogrel and referred for repeat coronary angiography with the plan to treat the diagonal lesion previously observed.
Cardiac catheterization
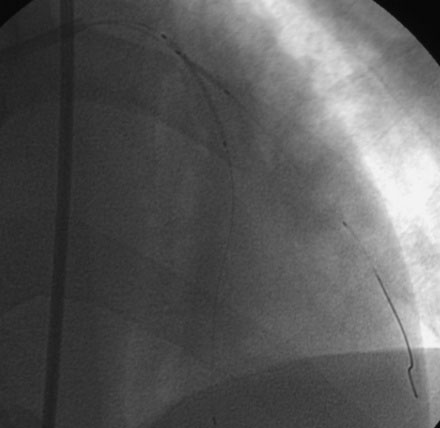
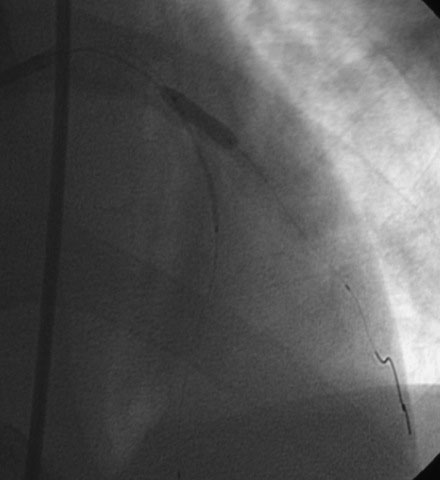
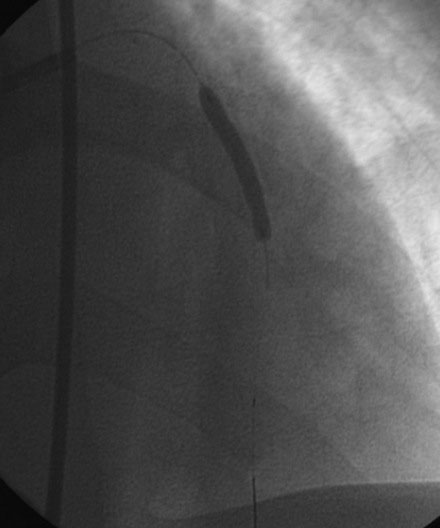
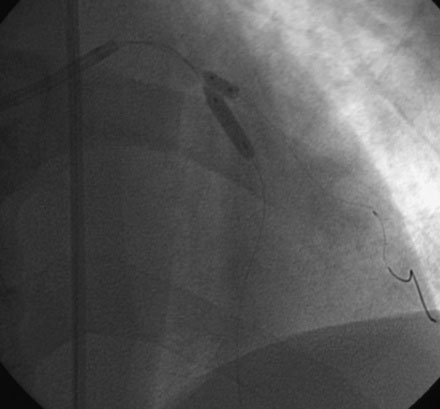
The angiographic appearance of the coronary arteries had not changed since the prior catheterization. Because the diagonal artery was very large in caliber and vascular distribution and the disease involved the ostium of this vessel, and because there was also disease involving the left anterior descending artery at the bifurcation, the operator planned to use a “crush” stent technique to treat the complex disease of the LAD/diagonal bifurcation. After achieving therapeutic anticoagulation with unfractionated heparin, an 8 French, “C” left 4.5 guide catheter was engaged in the left coronary artery and floppy-tipped guidewires were placed in the diagonal and the LAD. A 3.5 mm diameter by 12 mm long paclitaxel-eluting stent was positioned in the diagonal at the ostium and a 3.5 mm diameter by 28 mm long paclitaxel-eluting stent was positioned in the LAD with the LAD stent spanning the ostium of the diagonal artery (Figure 44-5). With the LAD stent in place, the operator first deployed the diagonal stent (Figure 44-6). The catheter and guidewire were removed from the diagonal branch and the LAD stent was deployed (Figure 44-7). A floppy guidewire was then passed into the diagonal through the side of the LAD stent struts and both the LAD and diagonal stents were postdilated using a “kissing” balloon strategy (3.5 mm diameter by 15 mm long noncompliant balloon in the LAD and 3.5 mm diameter by 6 mm long noncompliant balloon in the diagonal) (Figure 44-8). The final angiographic result is shown in Figure 44-9 and Video 44-2.
Discussion
Bifurcation lesions remain a significant challenge. Ischemic complications from loss or compromise of the side branch as well as high restenosis and stent thrombosis rates with complex stenting strategies limit the utility of percutaneous approaches.1,2 Bifurcation lesions vary depending on the size of the involved vessels, the location of the plaque relative to these branches, the angle at which the side branch originates from the parent vessel, and the area of myocardium supplied by the side branch. The heterogeneous nature of bifurcation lesions complicates their management since few studies control for these important factors, leaving the operator unsure as to the optimal strategy for any individual patient.
Recent randomized controlled trials suggest that bifurcation lesions can initially be managed simply by stenting the main vessel with the use of provisional stenting of the side branch only if an inadequate result is obtained.3,4 When this strategy is adopted, a second stent is necessary in the side branch in only one third of cases.5 However, this strategy does not necessarily apply to all bifurcation lesions. For example, if the side branch is very large in caliber and vascular distribution, and if access to the side branch is not predictably achievable after a stent is placed in the main vessel, then the operator may chose a more complex stenting procedure that reliably provides an acceptable acute result. In the case presented here, the bifurcation was characterized by severe disease primarily of the ostium of a very large diagonal side branch. The disease of the main branch (the left anterior descending artery) appeared to be more modest in severity. However, stenting the diagonal branch alone might have shifted plaque into the LAD, potentially worsening the stenosis severity in that vessel or even closing it. Furthermore, if the operator chose to treat just the diagonal ostium, adequate treatment of this area would have required that the stent protrude into the LAD. This might have impaired future access to the LAD beyond the stent, and, in the event of luminal compromise of the LAD after diagonal stenting or if the LAD disease progressed and required intervention, the presence of a stent protruding out of the diagonal ostium might have made a percutaneous approach difficult or even impossible. With this in mind, the operator chose a more predictable strategy of using a crush stent technique to treat this bifurcation.
The crush stent technique remains a controversial management strategy for bifurcations. Although it leads to a highly predictable acute outcome, it has been associated with stent thrombosis rates of 2% to 4%.5,6 Furthermore, the best outcomes with this technique depend upon performance of final “kissing balloon” angioplasty. When final kissing-balloon angioplasty of the bifurcation is performed, the restenosis rates of the main branch and side branch are 6% and 10% respectively.6 If kissing-balloon angioplasty is not performed, the restenosis rates of the main branch and side branch are 12% and 41%, respectively.6 Clearly, novel techniques and, possibly, dedicated bifurcation stents are necessary to improve the outcomes in this complex lesion subset.
1. Al Suwaidi J., Yeh W., Cohen H.A., Detre K.M., Williams D.O., Holmes D.R.Jr. Immediate and one year outcome in patients with coronary bifurcation lesions in the modern era (NHLBI dynamic registry). Am J Cardiol. 2001;87:1139-1144.
2. Yamashita T., Nishida T., Adamian M.G., Briguori C., Vaghetti M., Corvaja N., Albiero R., Finci L., DiMario C., Tobis J.M., Colombo A. Bifurcation lesions: two stents versus one stent: immediate and follow-up results. J Am Coll Cardiol. 2000;35:1145-1151.
3. Steigen T.K., Maeng M., Wiseth R., et al. Nordic PCI Study Group Randomized study on simple versus complex stenting of coronary artery bifurcation lesions: the Nordic Bifurcation Study. Circulation. 2006;114:1955-1961.
4. Colombo A., Bramucci E., Sacca S., Violini R., Lettieri C., Zanini R., Sheiban I., Paloscia L., Grube E., Schofer J., Bolognese L., Orlandi M., Niccoli G., Latib A., Airoldi F. Randomized study of the crush technique versus provisional side-branch stenting in true coronary bifurcations. The CACTUS (Coronary Bifurcations: Application of the Crushing Technique Using Sirolimus Eluting Stents) Study. Circulation. 2009;119:71-78.
5. Moussa I., Costa R.A., Leon M.B., Lansky A.J., Lasic Z., Cristea E., Trubelja N., Carlier S.G., Mehran R., Dangas G.D., Weisz G., Kreps E.M., Collins M., Stone G.W., Moses J.W. A prospective registry to evaluate sirolimus eluting stents implanted at coronary bifurcation lesions using the “crush technique”. Am J Cardiol. 2006;97:1317-1321.
6. Hoye A., Iakovou I., Ge L., van Mieghem C.A.G., Ong A.T.L., Cosgrave J., Sangiorgi G.M., Airoldi F., Montorfano M., Michev I., Chieffo A., Carlino M., Corvaja N., Aoki J., Rodriguez Granillo G.A., Valgimigli M., Sianos G., van der Giessen W.J., de Feyter P.J., van Domburg R.T., Serruys P.W., Colombo A. Long-term outcomes after stenting of bifurcation lesions with the “crush” technique: Predictors of an adverse outcome. J Am Coll Cardiol. 2006;47:1949-1958.