CASE 44
FG, a 42-year-old patient with fulminant cardiac failure secondary to acute viral myocarditis, receives a heart (via UNOS) from a trauma victim. You are aware incidentally that the lungs, liver, and kidneys of the same donor have been used in other transplants around the globe.
QUESTIONS FOR GROUP DISCUSSION
RECOMMENDED APPROACH
Implications/Analysis of Family History
We are not provided with any family history for the patient.
Implications/Analysis of Clinical History
Acute and Chronic Rejection
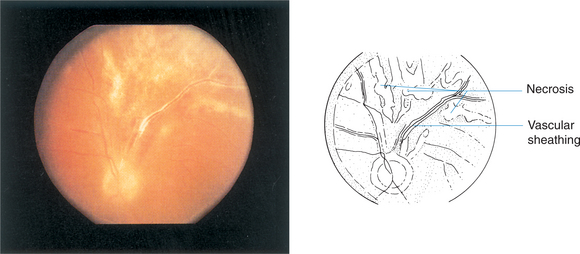
Chronic rejection occurs with release of a variety of mediators, including fibroblast growth factor and endothelial growth factor, which can cause an insidious fibrosing/proliferative reaction relatively refractory to immunosuppressive treatment. This could affect the heart, causing secondary lung failure (and the respiratory distress). However, the kinetic picture (<4 weeks after transplant) does not suggest this as a likely explanation.
Implications/Analysis of Laboratory Investigation
Side Effects of Drug Therapy
Could this disorder represent one of a possible number of side effects of the treatment he received for the transplant? In general, we know that chronically immunosuppressed populations show an increased frequency of malignancy, drug toxicity, and infections (Fig. 44-1).
Additional Laboratory Tests
The chest radiograph was consistent with an infiltrate, but biopsy showed no signs of malignancy.
Drug toxicity (or idiosyncratic drug effects) remains a possible explanation of this patient’s clinical presentation. Tacrolimus has been associated with fibrotic reactions, but this is very early for such an effect. Moreover, checking his file, you find he is not on tacrolimus as immunosuppressant!
There is no eosinophilia, which is often seen in the case of hypersensitivity reactions.
Aldallal N. Inflammatory response in airway epithelial cells isolated from patients with cystic fibrosis. Am J Respir Crit Care Med. 2002;166:1248.
Araujo MB, et al. Development of donor specific microchimerism in liver transplant recipient with HLA-DRB1 and -DQB1 mismatch related to rejection episodes. Transplant Proc. 2004;36:953.
Arul A, Murday AJ, Jackson R. Natural killer-like T cell lymphoma, CD56+, following cardiac transplantation. J Heart Lung Transplant. 2004;23:783.
Blusch JH, et al. Infection of nonhuman primate cells by pig endogenous retrovirus. J Virol. 2000;74:7687.
Chalasani G, et al. The allograft defines the type of rejection (acute versus chronic) in the face of an established effector immune response. J Immunol. 2004;172:7813.
Chantranuwat C, et al. Sudden unexpected death in cardiac transplant recipients: An autopsy study. J Heart Lung Transplant. 2004;23:683.
Chen HL, et al. Pediatric fulminant hepatic failure in endemic areas of hepatitis B infection: 15 years after universal hepatitis B vaccination. Hepatology. 2004;39:58.
Cho JH. Advances in the genetics of inflammatory bowel disease. Curr Gastroenterol Rep. 2004;6:467.
Conese M, et al. Neutrophil recruitment and airway epithelial cell involvement in chronic cystic fibrosis lung disease. J Cyst Fibros. 2003;2:129.
Corvol H, et al. Distinct cytokine production by lung and blood neutrophils from children with cystic fibrosis. Am J Physiol Lung Cell Mol Physiol. 2003;284:L997.
D’Haens G, Hlavaty T. Advances in medical therapy for Crohn’s disease. Curr Gastroenterol Rep. 2004;6:496.
De Hertogh G, Geboes K. Crohn’s disease and infections: A complex relationship. MedGenMed. 2004;10:14.
Dransfield MT, Garver RI, Weill D. Standardized guidelines for surveillance bronchoscopy reduce complications in lung transplant recipients. J Heart Lung Transplant. 2004;23:110.
Fateh-Moghadam S. Cytomegalovirus infection status predicts progression of heart-transplant vasculopathy. Transplantation. 2003;76:1470.
Galili U. Interaction of the natural anti-Gal antibody with α-galactosyl epitopes: A major obstacle for xenotransplantation in humans. Immunol Today. 1993;14:480.
Gardner R, et al. Gamma/delta T-cell lymphoma as a recurrent complication after transplantation. Leuk Lymphoma. 2004;45:2355.
Grazia et al Grazia TJ, et al: A two-step model of acute CD4 T-cell mediated cardiac allograft rejection. J Immunol 172:7451.
Halloran PF. Immunosuppressive drugs for kidney transplantation. N Engl J Med. 2004;26:2715.
Helmi M, et al. Aspergillus infection in lung transplant recipients with cystic fibrosis: Risk factors and outcomes comparison to other types of transplant recipients. Chest. 2003;123:800-808.
Hoercher KJ, et al. Cardiac transplantation at the Cleveland Clinic. Clin Transpl. 2003;17:267.
Huo TI, et al. Long-term outcome of kidney transplantation in patients with hepatitis C virus infection. Hepatogastroenterology. 2001;48:169.
Kaufman DB, et al. Immunosuppression: Practice and trends. Am J Transpl. 2004;4:38.
Kaufman SS, et al. Discrimination between acute rejection and adenoviral enteritis in intestinal transplant recipients. Transplant Proc. 2002;34:943.
Lacouture ME, Hsieh FH. Skin rash in a transplant patient receiving multiple drugs. Cleve Clin J Med. 2003;70:1071.
Lin KW, Kirchner JT. Hepatitis B. Am Fam Physician. 2004;69:75.
Loinaz C, et al. Bacterial infections after intestine and multivisceral transplantation. Transplant Proc. 2003;35:1929.
Ludwiczek O, et al. Imbalance between interleukin-1 agonists and antagonists: Relationship to severity of inflammatory bowel disease. Clin Exp Immunol. 2004;138:323.
Magre S, et al. Reduced sensitivity to human serum inactivation of enveloped viruses produced by pig cells transgenic for human CD55 or deficient for galactosyl-α(1-3) galactosyl epitope. J Virol. 2004;78:5812.
Mahmond IM, et al. The impact of hepatitis C virus on renal graft and patient survival: A 9-year prospective study. Am J Kidney Dis. 2004;43:131.
Mazariegos GV, et al. Graft versus host disease in intestinal transplantation. Am J Transpl. 2004;4:1459.
Meloni F. Bronchoalveolar lavage cytokine profile in a cohort of lung transplant recipients: A predictive role of interleukin-12 with respect to onset of bronchiolitis obliterans syndrome. J Heart Lung Transplant. 2004;23:1053.
Neff GW, et al. Outcomes in liver transplant recipients with hepatitis B virus: Resistance and recurrence patterns from a large transplant center over the last decade. Liver Transplant. 2004;10:1372.
Nigen S, Knowles SR, Shear NH. Drug eruptions: Approaching the diagnosis of drug-induced skin diseases. J Drugs Dermatol. 2003;2:278.
Paul LC, et al. Antibodies and chronic organ graft rejection. Ann Transplant. 1997;2:46.
Piazza A, et al. Impact of donor-specific antibodies on chronic rejection occurrence and graft loss in renal transplantation: Post-transplant analysis using flow cytometric techniques. Transplantation. 2001;71:1106.
Quinn G, et al. Porcine endogenous retrovirus transmission characteristics of galactose α1-3 galactose deficient pig cells. J Virol. 2004;78:5805.
Rosen HR, et al. Cutting edge: Identification of hepatitis C virus-specific CD8+ T cells restricted by donor HLA alleles following liver transplantation. J Immunol. 2004;173:5355.
Schwartz KB, et al. Viral hepatitis. J Pediatr Gastroenterol Nutr. 2002;35:S29.
Schwartz KB. Pediatric issues in new therapies for hepatitis B and C. Curr Gastroenterol Rep. 2003;5:233.
Starzl TE, et al. Chimerism and tolerance in transplantation. Proc Natl Acad Sci U S A. 2004;101(Suppl 2):14607.
Starzl TE, Zinkernagel RM. Antigen localization and migration in immunity and tolerance. N Engl J Med. 339, 1905.
Thomas AR, et al. Hepatitis B vaccine coverage among the infants born to women without perinatal screening for hepatitis B virus infections: Effect of the joint statement of thimerosal in vaccines. Pediatr Infect Dis J. 2004;23:313.
Treem WR. Fulminant hepatic failure in children. J Pediatr Gastroenterol Nutr. 2002;35:S33.
Vanclaire J, Cornu Ch, Sokal EM. Fulminant hepatitis B in an infant born to a hepatitis Be antibody positive, DNA negative carrier. Arch Dis Child. 1991;66:983.
Verkman AS, Song Y, Thiagarajah JR. Role of airway surface liquid and submucosal glands in cystic fibrosis lung disease. Am J Physiol Lung Cell Mol Physiol. 2003;284:C2.
Weiner SM, et al. Impact of in vivo complement activation and cryoglobulins on graft. Clin Transpl. 2004;18:7.
Wy AU, et al. Graft versus-host disease after liver transplantation: Documentation by fluorescent in situ hybridization and human leucocyte antigen typing. Clin Transpl. 2000;14:174.
Zheng HX, et al. Interleukin 10 production genotype protects against acute persistent rejection after lung transplantation. J Heart Lung Transplant. 2004;23:541.
Zhong R, et al. Improvement in human decay accelerating factor transgenic porcine kidney xenograft rejection with intravenous administration of GAS914, a polymeric form of alpha GAL. Transplantation. 2003;75:10.