CHAPTER 43 Perioperative Hepatic Dysfunction
7 What is hepatorenal syndrome? How does it differ from acute renal failure in patients with end-stage liver disease?
13 How can laboratory results be used to stratify perioperative risk in patients with cirrhosis?
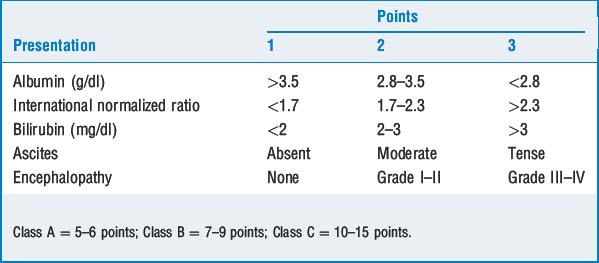
Liver function tests have also been used to predict outcome following surgery in patients with chronic hepatic impairment. Child’s scoring system (Table 43-1) was originally used to stratify risk in patients undergoing portosystemic shunting procedures. Using this method, 30-day mortality rates of 10%, 14% to 31%, and 51% to 80% were identified in Child’s class A, B, and C patients, respectively, when undergoing noncardiac surgery. More recently the Model for End-Stage Liver Disease (MELD) scoring system was created as a more objective method for assessing mortality in cirrhotic patients (Table 43-2). When compared to the Child’s scoring system, the MELD is a superior predictor of perioperative risk in patients with cirrhosis. MELD scores of <10, 10 to 14, and <14 correlate well with the Child’s A, B, and C classifications.
| MELD Score = 3.8 × log (e) (bilirubin mg/dl) + 11.2 × log (e) (INR) + 9.6 log (e) (creatinine mg/dl) |
| MELD <10 = Low perioperative mortality |
| MELD 10–14 = Moderate perioperative mortality |
| MELD >14 = Severe perioperative mortality |
INR, International normalized ratio; MELD, Model for End-Stage Liver Disease.
14 What risk factors for liver disease can be identified by history and physical examination?
Table 43-3 lists risk factors for liver disease easily obtained in a brief medical history. Physical examination may yield stigmata of chronic liver disease, including ascites, hepatosplenomegaly, spider angiomata, caput medusae, and gynecomastia. Patients with these signs or a prior history of jaundice or liver disease should have liver function tests evaluated before surgery.
| Risk Factor | Example |
|---|---|
| Viral hepatitis | Intravenous drug abuse, transfusion, tattoos, contact with infected person |
| Drugs | Alcohol, prescription medications (e.g., acetaminophen, haloperidol, tetracycline, isoniazid, hydralazine, captopril, and amiodarone) |
| Autoimmune disease | Systemic lupus erythematosus, sarcoidosis, mixed connective tissue disorder |
| Metabolic disease | Hemochromatosis, Wilson’s disease, cystic fibrosis, α1-antitrypsin deficiency, and glycogen storage disease |
| Inflammatory bowel disease | Crohn’s disease and ulcerative colitis/primary sclerosing cholangitis |
17 List the common causes of unconjugated and conjugated hyperbilirubinemia
Unconjugated hyperbilirubinemia is defined as an elevation of the total serum bilirubin of which the conjugated fraction does not exceed 15%. The causes are listed in Table 43-4.
| Cause | Example |
|---|---|
| Hemolysis | Incompatible blood transfusion, arterial/venous bypass circuit, congenital or acquired defects (e.g., autoimmune and drug-induced hemolytic anemia, glucose-6-phosphatase deficiency) |
| Hematoma resorption | Retroperitoneal or pelvic hematoma |
| Enzymatic deficiencies | Congenital deficiency (Gilbert syndrome) to complete absence (Crigler-Najjar syndrome) of hepatic uridine diphosphoglucuronyl transferase |
Elevations of conjugated bilirubin are caused by hepatocyte dysfunction and/or intrahepatic or extrahepatic stasis. A differential diagnosis of biliary stasis is listed in Table 43-5.
TABLE 43-5 Causes of Biliary Obstruction/Stasis
| Extrahepatic Obstruction | Intrahepatic Obstruction |
|---|---|
| Tumor (bile duct, pancreas, and duodenum) | Primary biliary cirrhosis |
| Cholecystitis | Drugs (estrogens, anabolic steroids, tetracycline, and valproic acid) |
| Biliary stricture | Total parenteral nutrition |
| Ascending cholangitis | Pregnancy |
| Sclerosing cholangitis |
18 What are the main causes of hepatocyte injury?
| Cause | Example |
|---|---|
| Infection | Hepatitis A, B, and C; cytomegalovirus; Epstein-Barr virus |
| Drugs | Acetaminophen, isoniazid, phenytoin, hydralazine, α-methyldopa, sulfasalazine |
| Sepsis | Pneumonia |
| Total parenteral nutrition (TPN) | Abnormal liver function tests in 68%–93% of patients given TPN for longer than 2 weeks |
| Hypoxemia | Lower arterial oxygen or interference with peripheral use as in cyanide and carbon monoxide poisoning |
| Ischemia | Increased venous pressure (e.g., congestive heart failure, pulmonary embolus, and positive-pressure ventilation) Decreased arterial pressure (e.g., hypovolemia, vasopressors, and aortic cross-clamp) |
20 How do inhalational agents alter hepatic blood flow?
Key Points: Perioperative Hepatic Dysfunction
1. Befeler A., Palmer D. The safety of intra-abdominal surgery in patients with cirrhosis. Arch Surg. 2005;140:650-654.
2. Millwala F., Nguyen G.C. Outcomes of patients with cirrhosis undergoing non-hepatic surgery: risk assessment and management. World J Gastroenterol. 2007;13:4056-4063.
3. Mushlin P., Gelman. Hepatic physiology and pathophysiology. In: Miller R., editor. Miller’s anesthesia. ed 6. Philadelphia: Elsevier Churchill Livingstone; 2005:743-775.