CASE 43
Ms. Bell received cardiac transplantation approximately 6 years earlier for a cardiomyopathy that developed after she received chemotherapy (doxorubicin [Adriamycin]) for breast cancer. She has had routine endomyocardial biopsies each year, the last being 1 year ago. At that time the pathologist read the biopsy as normal, with no signs of rejection. The only change in her anti-rejection therapy over the past 2 years was a reduction in the prednisone dose (now 7.5 mg/day) and replacement of cyclosporine (which she had received for nearly 5 years since the time of transplantation) with tacrolimus. You (her son) were told that the advantage of tacrolimus was a slightly improved toxicity profile. You arrived home for a visit this afternoon to find your mother confused and with a droop on the left side of her face/mouth. You immediately call an ambulance and arrange transport to the local hospital.
QUESTIONS FOR GROUP DISCUSSION
RECOMMENDED APPROACH
Implications/Analysis of Clinical History
Ms. Bell received a cardiac transplant 6 years ago, and all the evidence we are provided with indicates that this was a successful graft in that the yearly endomyocardial biopsies have all been normal. In fact, the only change in her anti-rejection therapy has been a reduction in immunosuppressive therapy and change from cyclosporine to tacrolimus, which is slightly less toxic.
DIAGNOSIS
Prednisone has been shown to leave patients at increased risk of atherosclerotic disease, both within the vessels of the grafted organs (here, the heart) and elsewhere in the body (e.g., the brain). This narrowing of the blood vessels, in turn, results in increased risk of ischemic damage to the central organs (heart attack and, in the brain, a stroke). Most of the evidence points to prednisone toxicity as causing narrowing of the blood vessels, which, in turn, led to ischemic damage in the brain. This manifested as a stroke.
ETIOLOGY: TRANSPLANTATION COMPLICATIONS
Graft Rejection
Acute Rejection
ROLE OF SOLUBLE MEDIATORS AND NONSPECIFIC IMMUNE CELLS
Chemokines, produced by a number of cells in the inflammatory milieu (including fibroblasts/endothelial cells) attract other cells to the site of rejection, further propagating the process. Along with endothelial cell activation, engagement of the serum-derived plasminogen and thrombotic cascade occurs, as well as thrombosis mediated both by tissue factor and a novel prothrombinase discovered comparatively recently and referred to as fibroleukin. This procoagulant activity (a product of endothelial cells and macrophages) is distinct from previously described ones and occurs after immune-mediated activation of an inflammatory event.
Chronic Rejection
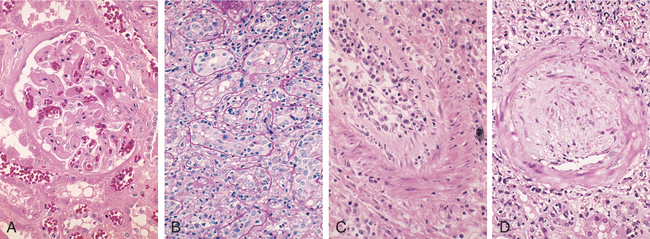
Chronic rejection may reflect the net outcome of numerous (even unidentified) minor acute rejection episodes and/or a chronic immunostimulation directed against minor incompatibilities (minor antigens) between graft and recipient. Like acute rejection, chronic rejection involves components of cell-mediated immunity; however, chronic rejection also involves the dramatic increase in non–T cell–derived growth factors (e.g., fibroblast growth factor), which leads to the production of fibrosed tissue that does not function well (Fig. 43-1). Note, too, that chronic rejection is generally not easily treated.
Infections
Complications of the immunosuppressive therapy used to ensure graft survival are unfortunately quite common. An increased incidence of (opportunistic) infection is observed in these patients. Recrudescence of earlier infections that were previously cleared can also cause problems.