CHAPTER 42
Thoracic Compression Fracture
Definition
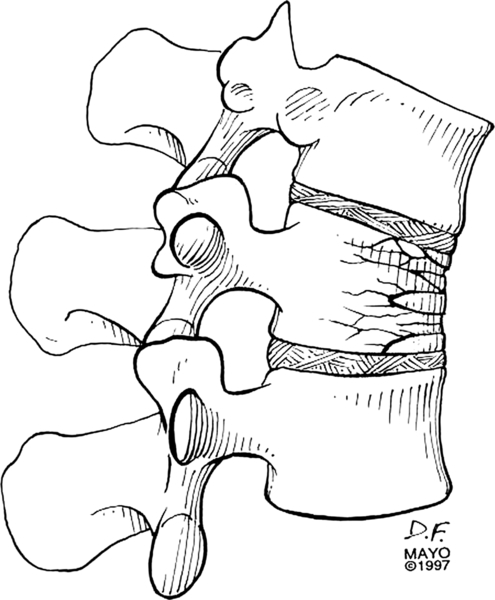
A compression fracture is caused by forces transmitted along the vertebral body. The ligaments are intact, and compression fractures are usually stable [1] (Fig. 42.1). Compression fractures in the thoracic vertebrae are commonly seen in osteoporosis with decreased bone mineral density. They may be asymptomatic and diagnosed incidentally on radiography. Such fractures may occur with trivial trauma and are usually stable [2,3]. Pathologic vertebral fractures may occur with metastatic cancer (commonly from lung, breast, or prostate) as well as with other processes affecting vertebrae. Trauma, such as a fall from a height or a motor vehicle accident, can also result in thoracic compression fracture. Considerable force is required to fracture healthy vertebrae, which are resistant to compression. In such cases, the force required to produce a fracture may cause extension of fracture components into the spinal canal with neurologic findings. There may be evidence of additional trauma, such as calcaneal fractures from a fall. Multiple thoracic compression fractures, as seen with osteoporosis, can produce a kyphotic deformity [4–6]. An estimated 1.5 million vertebral compression fractures occur annually in the United States, with 25% of postmenopausal women affected in their lifetime. Estimates indicate that there are 44 million persons with osteoporosis and 34 million with low bone mass in the United States [7]. Existence of vertebral compression fracture increases the risk of future vertebral compression fractures (with 1 fracture, there is a 5-fold increase; with 2 or more fractures, there is a 12-fold increase) [8].
Symptoms
Pain in the thoracic spine over the affected vertebrae is the usual hallmark of the presentation. It may be severe, sharp, exacerbated with movement, and decreased with rest. Severe pain may last 2 to 3 weeks and then decrease during 6 to 8 weeks, but pain may persist for months. Acute fractures in osteoporosis, however, may result in little discomfort or poor localization [9]. In osteoporotic fractures, the mid and lower thoracic vertebrae are typically affected. A good history and physical examination are essential as there may be indicators of a more ominous underlying pathologic process [10,11].
Physical Examination
Tenderness with palpation or percussion over the affected region of the thoracic vertebrae is the primary finding on physical examination. Spinal movements also produce pain. Kyphotic deformity, loss of height, and impingement of the lower ribs on the superior iliac crest may be present in the patient who has had multiple prior compression fractures. Neurologic examination below the level of the fracture is recommended to assess for presence of reflex changes, pathologic reflexes such as Babinski sign, and sensory alterations. Sacral segments can be assessed through evaluation of rectal tone, volitional sphincter control, anal wink, and pinprick if there is concern about bowel and bladder function [12]. It is also important to assess the patient’s gait for stability. Comorbid neurologic and orthopedic conditions may contribute to gait dysfunction and fall risk [13,14].
Functional Limitations
Functional limitations in a patient with an acute painful thoracic compression fracture can be significant. The patient may experience loss of mobility and independence in activities of daily living and household activities, and there may be an impact on social, avocational, vocational, and psychological functioning. In patients with severe symptoms, hospitalization may be necessary [15].
Diagnostic Testing
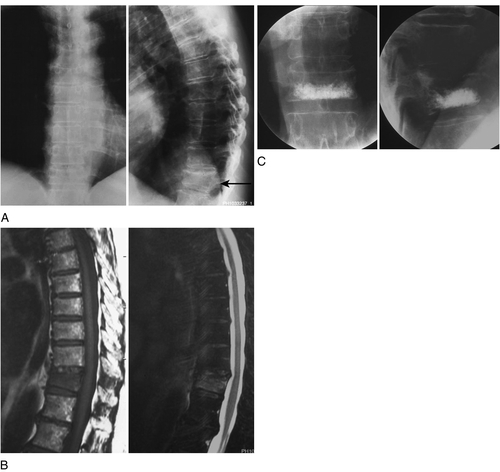
Anteroposterior and lateral radiographs of the thoracic spine can confirm the clinical impression of a thoracic compression fracture. On radiographic examination in a thoracic compression fracture, the height of the affected vertebrae is reduced, generally in a wedge-shaped fashion, with anterior height less than posterior vertebral height. In osteoporosis, biconcave deformities can also be noted on spinal radiographs (Fig. 42.2A). A bone scan may help localize (but not necessarily determine the etiology of) processes such as metastatic cancer, occult fracture, and infection. Spinal imaging, such as computed tomography or magnetic resonance imaging, may also elucidate further detail [16] (Fig. 42.2B). Percutaneous needle biopsy of the affected vertebral body can be helpful diagnostically in selected cases. Laboratory tests are obtained as appropriate. These include a complete blood count and sedimentation rate or C-reactive protein level (which are nonspecific but sensitive indicators of an occult infection or inflammatory disease). Serum alkaline phosphatase, serum and urine protein electrophoresis, and other laboratory tests are beneficial when a malignant neoplasm is suspected. Diagnostic testing is directed, as appropriate, on the basis of the entire clinical presentation, including secondary causes of osteoporosis. Bone densitometry can be performed when the patient is improved clinically.
Treatment
Initial
Initial treatment consists of activity modification, including limited bed rest. Cushioning with use of a mattress overlay (such as an egg crate) can also be helpful. Pharmacologic agents, including oral analgesics, muscle relaxants, and anti-inflammatory medications, as appropriate to the patient, are helpful. Agents such as tramadol 50 mg (one or two every 4 to 6 hours, not exceeding eight per day), acetaminophen 300 mg/codeine 30 mg (one or two every 4 to 6 hours), and controlled-release oxycodone CR (10 mg or 20 mg every 12 hours) may be considered. Acetaminophen dose should not exceed 3 g/day. Muscle relaxants such as cyclobenzaprine, 10 mg three times daily, may be helpful initially with muscle spasm. A variety of nonsteroidal anti-inflammatory drugs, including celecoxib (Celebrex, a cyclooxygenase 2 inhibitor), can be considered, depending on the patient. Calcitonin (one spray daily, alternating nostrils, providing 200IU per spray) has also been used for painful osteoporotic fractures [19]. Stool softeners and laxatives may be necessary to reduce strain with bowel movements and constipation, particularly with narcotic analgesics. Selection of pharmacologic agents must factor in the age, comorbidities, and clinical status of the patient. Avoidance of spinal motion, especially flexion, by appropriate body mechanics (such as log rolling in bed) and spinal bracing is helpful. There are a variety of spinal orthoses that reduce spinal flexion (Fig. 42.3). They must be properly fitted [20,21]. A lumbosacral orthosis may be sufficient for a low thoracic fracture. A thoracolumbosacral orthosis is used frequently (Fig. 42.3A-D). If a greater degree of fracture immobilization is required, an off-the-shelf orthosis (Fig. 42.3E) or a custom-molded body jacket may be fitted by an orthotist. Proper diagnosis and treatment of underlying contributors to the thoracic compression fracture are necessary [22,23]. Most thoracic compression fractures will heal with symptomatic improvement in 4 to 6 weeks [24,25].

Rehabilitation
Physical therapy is helpful to assist with gentle mobilization of the patient by employing proper body mechanics, optimizing transfer techniques, and training with gait aids (such as a wheeled walker) to reduce biomechanical stresses on the spine and to ensure gait safety [26]. Pain-relieving modalities, such as therapeutic heat or cold, and transcutaneous electrical stimulation may also be employed. Exercise should not increase spinal symptoms and should be implemented at the appropriate juncture. In addition to proper body mechanics and postural training emphasizing spinal extension and avoidance of flexion, spinal extensor muscle strengthening, limb muscle strengthening, stretching to muscle groups (such as the chest, hips, and lower extremity muscles), and deep breathing exercises may also be indicated. Weight-bearing exercises for bone health, balance, and fall prevention are also important [27]. Proper footwear, with cushioning inserts, can also be helpful. Occupational therapy can help the patient with activities of daily living, reinforce proper spinal ergonomics, address equipment needs, and prevent falls. Successful rehabilitation is targeted at increasing the patient’s comfort, decreasing deformity, and decreasing resultant disability and is individualized to address specific patient needs [28–30].
Procedures
Invasive procedures are generally not necessary. Percutaneous vertebroplasty or kyphoplasty with use of polymethyl methacrylate may be helpful to reduce fracture pain, to reinforce thoracic vertebral strength, and to improve function; with kyphoplasty, some potential restoration of vertebral height has been reported [26,31] (Fig. 42.2C). Patients with imaging evidence of an acute or a subacute thoracic fracture who have correlating pain, who fail to improve with conservative management, and who are without contraindications may be candidates for such interventional procedures [32,33]. In two randomized controlled trials, no beneficial effect was noted in vertebroplasty versus sham [32,34].
Surgery
Surgery is rarely necessary. Surgical stabilization can be considered in patients with continued severe pain after compression fracture as a result of nonunion of the fracture, in patients with spinal instability, or if neurologic complications occur. Referral to a spine surgeon is recommended in these cases for further assessment [35].
Potential Disease Complications
Neurologic complications, including nerve or spinal cord compromise, as well as orthopedic complications with continued pain, nonunion, and instability can occur. Underlying primary disease, for example, metastatic thoracic compression, needs to be addressed. Patients with severe kyphosis may experience cardiopulmonary dysfunction. Severe kyphosis may also result in rib impingement on the iliac bones, producing further symptoms. Severe pain accompanying a fracture may further limit deep breathing and increase the risk of pulmonary complications, such as pneumonia. Progressive spinal deformity may produce secondary pain generators. The patient may have progressive levels of dependency as a result.
Potential Treatment Complications
Side effects with medications, particularly nonsteroidal anti-inflammatory drugs as well as narcotic medications, can occur. It is important to select medications appropriate for individual patients. There may be difficulty with the use of spinal orthotics, such as intolerance in patients with gastroesophageal reflux disease. Kyphotic patients frequently do not tolerate orthoses and fitting is a problem. Complications of vertebroplasty or kyphoplasty can include infection, bleeding, fracture (in the treated or adjacent vertebrae), and systemic issues such as embolism. Cement leaks into surrounding tissues with spinal cord, spinal nerve, or vascular compression can occur [36]. Surgery can result in many complications, not only from general anesthesia risks but also from infection, bleeding, or thromboembolism. Poor mechanical strength of bone, as in osteoporosis with paucity of dense lamellar and cortical bone, may result in suboptimal surgical outcome.
Acknowledgments
The author thanks Dr. Kent Thielen for use of the case study; Sara Harstad for orthotic modeling; and Pamela Harders for secretarial support.







