CASE 42
History: A 37-year-old man has recurrent episodes of dysphagia.
1. Which of the following should be included in the differential diagnosis of the imaging finding shown in figure A? (Choose all that apply.)
E. Intramural pseudodiverticulosis
2. What structures are visible, filled by the barium?
B. Fibrosed traction diverticula
C. Scarred pulsion diverticula
D. Dilated excretory ducts of the esophageal mucous glands
3. What is the most common other esophageal abnormality seen with this condition?
4. What pathogen has been associated with this condition?
ANSWERS
CASE 42
Esophageal Intramural Pseudodiverticulosis
1. A, D, and E
2. D
3. B
4. C
Reference
Levine MS. Other esophagitides. In: Gore RM, Levine MS, eds. Textbook of Gastrointestinal Radiology. 2nd ed. Philadelphia: WB Saunders; 2000:381–384.
Cross-Reference
Gastrointestinal Imaging: THE REQUISITES, 3rd ed, p 30.
Comment
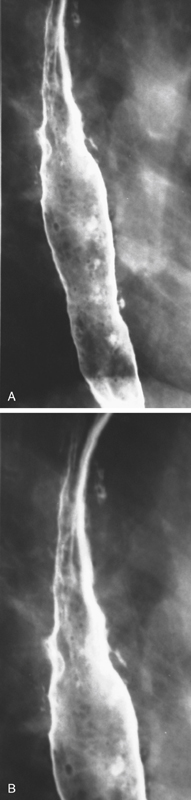
Intramural pseudodiverticulosis of the esophagus is a rare condition. Anatomically it represents barium filling the sparse adenomatous excretory ducts of the mucous glands of the esophagus. These mucous glands are normal anatomic structures of the esophagus but typically are not visible on radiologic studies. However, sometimes (thought to relate to chronic inflammation) these ducts become dilated, allowing barium to track into the ducts and glands.
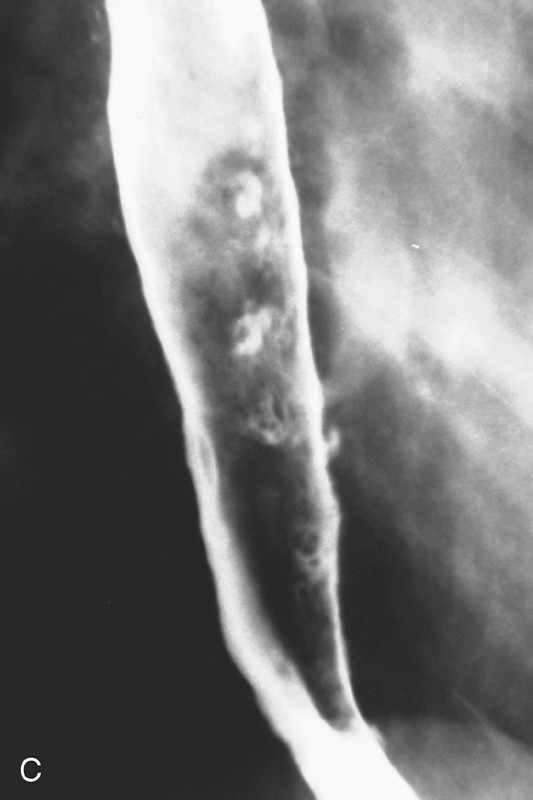
Some type of inflammation must be present for these pathologic changes to occur, and the large majority of these patients have evidence of esophageal inflammation. A large proportion of patients with intramural pseudodiverticulosis also have strictures. The strictures are typically benign, but intramural pseudodiverticulosis has been reported in association with malignant strictures. Candida organisms have been found in patients with this condition, but the exact causal relationship is uncertain. More than likely, this finding represents a secondary infection of the glands and not a predisposing condition. Rarely this condition is found in patients with an otherwise normal esophagus. However, the very presence of intramural pseudodiverticulosis is abnormal.
Radiologically the intramural pseudodiverticulosis appears as small outpouchings, often with a flask shape. These outpouchings are most commonly mistaken for ulcers by those who are unfamiliar with the condition. Intramural pseudodiverticulosis may be either segmental or diffuse. Even intramural tracking and deep penetration may be evident. On CT, the condition produces changes of esophageal wall thickening and irregularity of the lumen, mimicking esophageal carcinoma. Because it is primarily a radiologic oddity, the condition’s clinical course depends on treatment of the underlying condition.
Often, treatment of the stricture or inflammation results in a decrease or even disappearance of the pseudodiverticulosis. Slightly increased risks of adenocarcinoma of the esophagus have been associated with this condition.







