Procedure 41 Centralization for Radial Longitudinal Deficiency
![]() See Video 34: Centralization for Radial Deficiency
See Video 34: Centralization for Radial Deficiency
Indications
 Radial longitudinal deficiency (RLD) has been classified into four grades depending on the degree of hypoplasia of the radius (Table 41-1). Centralization is usually performed at 9 to 12 months of age because anesthesia is safer, preliminary soft tissue distraction can be carried out, and subsequent thumb reconstruction can be done before the child develops a maladaptive pattern.
Radial longitudinal deficiency (RLD) has been classified into four grades depending on the degree of hypoplasia of the radius (Table 41-1). Centralization is usually performed at 9 to 12 months of age because anesthesia is safer, preliminary soft tissue distraction can be carried out, and subsequent thumb reconstruction can be done before the child develops a maladaptive pattern.
 This procedure may be done first for children with type 0 or 1 deficiencies.
This procedure may be done first for children with type 0 or 1 deficiencies.
 Children with type 2 or greater deficiencies may need preliminary serial casting or soft tissue distraction using an external fixator.
Children with type 2 or greater deficiencies may need preliminary serial casting or soft tissue distraction using an external fixator.
| Type | Distal Radius | Proximal Radius |
|---|---|---|
| N | Normal | Normal |
| 0 | Normal | Normal, radioulnar synostosis, congenital radial head dislocation |
| 1 | >2 mm shorter than ulna | Normal, radioulnar synostosis, congenital radial head dislocation |
| 2 | Hypoplasia | Hypoplasia |
| 3 | Physis absent | Variable hypoplasia |
| 4 | Absent | Absent |
Examination/Imaging
Clinical Examination
 Sixty percent to 70% of children with RLD have an associated systemic or musculoskeletal abnormality, the most common being scoliosis. Therefore, before surgery, all children with RLD should undergo a thorough musculoskeletal and systemic examination, including spinal radiographs, cardiac echocardiographic evaluation, renal ultrasound, and a complete blood count.
Sixty percent to 70% of children with RLD have an associated systemic or musculoskeletal abnormality, the most common being scoliosis. Therefore, before surgery, all children with RLD should undergo a thorough musculoskeletal and systemic examination, including spinal radiographs, cardiac echocardiographic evaluation, renal ultrasound, and a complete blood count.
 It is important to assess elbow function. Some children are unable to flex the elbow, and the radial deviation deformity allows them to get the hand to the mouth. Correction of the radial deformity may improve the appearance but will limit function.
It is important to assess elbow function. Some children are unable to flex the elbow, and the radial deviation deformity allows them to get the hand to the mouth. Correction of the radial deformity may improve the appearance but will limit function.
Surgical Anatomy
 Children with RLD have anomalies involving the muscular, vascular, and nervous systems in addition to the obvious skeletal deformity.
Children with RLD have anomalies involving the muscular, vascular, and nervous systems in addition to the obvious skeletal deformity.
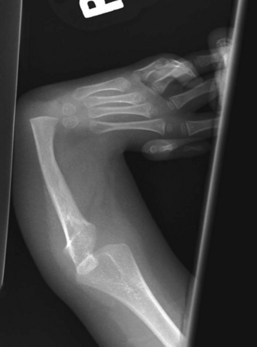
 Skeletal anomalies: The radius is either absent or partially developed, and the ulna is bowed posteriorly and shortened to two thirds its normal length. The articulation between the carpus and ulna does not form a normal joint. It is usually fibrous but can be lined by hyaline cartilage.
Skeletal anomalies: The radius is either absent or partially developed, and the ulna is bowed posteriorly and shortened to two thirds its normal length. The articulation between the carpus and ulna does not form a normal joint. It is usually fibrous but can be lined by hyaline cartilage.
 Muscle anomalies: The extensor carpi radialis longus and brevis may be absent or fused to the extensor digitorum communis (EDC). The extensor pollicis longus (EPL), extensor pollicis brevis (EPB), and abductor pollicis longus (APL) are present if the thumb metacarpal is present, or they may be fused to the surrounding tissues. The supinator is generally absent, as is the pronator quadratus. The pronator teres is absent if the radius is absent. The flexor carpi radialis longus and brevis are often absent. The flexor carpi ulnaris is usually present and normal, as is the flexor digitorum superficialis. The palmaris longus is often absent. The flexor pollicis longus is present only if the thumb metacarpal is present. If the thumb is present, the thenar muscles are usually present. The hypothenar, interosseous, and lumbrical muscles are usually normal.
Muscle anomalies: The extensor carpi radialis longus and brevis may be absent or fused to the extensor digitorum communis (EDC). The extensor pollicis longus (EPL), extensor pollicis brevis (EPB), and abductor pollicis longus (APL) are present if the thumb metacarpal is present, or they may be fused to the surrounding tissues. The supinator is generally absent, as is the pronator quadratus. The pronator teres is absent if the radius is absent. The flexor carpi radialis longus and brevis are often absent. The flexor carpi ulnaris is usually present and normal, as is the flexor digitorum superficialis. The palmaris longus is often absent. The flexor pollicis longus is present only if the thumb metacarpal is present. If the thumb is present, the thenar muscles are usually present. The hypothenar, interosseous, and lumbrical muscles are usually normal.
 Vascular anomalies: The brachial and ulnar artery are usually present and normal, but the radial artery is absent or attenuated. The interosseous arteries are usually well developed.
Vascular anomalies: The brachial and ulnar artery are usually present and normal, but the radial artery is absent or attenuated. The interosseous arteries are usually well developed.
 Nerve anomalies: The median and ulnar nerves are present, but the median nerve is the most superficial structure on the radial side of the arm and may be confused during surgical dissection with a tendinous structure. The median nerve must be identified first during the exposure. The radial nerve frequently ends at the elbow; thus, the median nerve supplies sensation to the radial side of the arm.
Nerve anomalies: The median and ulnar nerves are present, but the median nerve is the most superficial structure on the radial side of the arm and may be confused during surgical dissection with a tendinous structure. The median nerve must be identified first during the exposure. The radial nerve frequently ends at the elbow; thus, the median nerve supplies sensation to the radial side of the arm.
Exposures
 The four key steps of centralization are the following:
The four key steps of centralization are the following:
Procedure
Step 1: Preliminary Soft Tissue Distraction
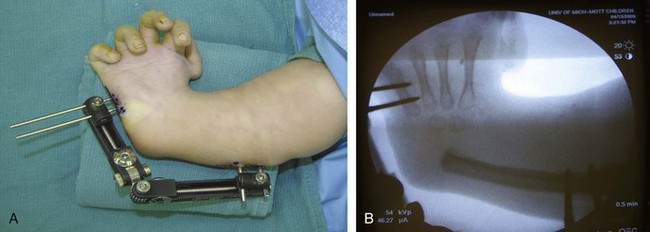
 A uniplanar external fixator device is applied on the ulnar side of the affected limb (the metacarpal of small finger and ulna of patient shown in Figure 41-4). This is best done at 6 to 9 months of age.
A uniplanar external fixator device is applied on the ulnar side of the affected limb (the metacarpal of small finger and ulna of patient shown in Figure 41-4). This is best done at 6 to 9 months of age.
 The parents begin distraction at a rate of 1 mm/day about 4 to 5 days after placement of the device. The patient is observed with a weekly clinic visit and radiograph.
The parents begin distraction at a rate of 1 mm/day about 4 to 5 days after placement of the device. The patient is observed with a weekly clinic visit and radiograph.
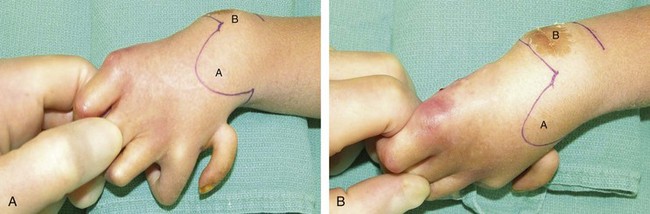
 Distraction is continued until the hand is about in a neutral position. Normally, it takes about 2 months of distraction to achieve this position (Fig. 41-5).
Distraction is continued until the hand is about in a neutral position. Normally, it takes about 2 months of distraction to achieve this position (Fig. 41-5).
 The external fixator device can be removed at the same time as surgery for centralization.
The external fixator device can be removed at the same time as surgery for centralization.
Step 2: Elevation of Bilobed Flap
 The skin is incised along the previously marked bilobed flap.
The skin is incised along the previously marked bilobed flap.
 The flap is raised in a plane superficial to the extensor retinaculum.
The flap is raised in a plane superficial to the extensor retinaculum.
Step 2 Pitfalls
Care should be taken to preserve the superficial cutaneous nerves and longitudinal veins.
Flaps should be kept as thick as possible to avoid devascularizing the wound edges.
Beware of the large dorsal branch of the median nerve, which replaces the absent superficial radial nerve that supplies sensation to the radial aspect of the hand. This branch is positioned in the subcutaneous fold between the wrist and forearm.
Step 3: Dissection of Nerve and Tendons
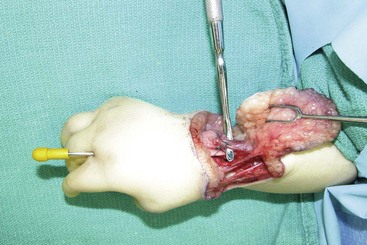
 The median nerve must be identified first during the exposure. It is the most superficial structure on the radial side of the distal forearm and can easily be confused with a tendinous structure (Fig. 41-6).
The median nerve must be identified first during the exposure. It is the most superficial structure on the radial side of the distal forearm and can easily be confused with a tendinous structure (Fig. 41-6).
 The extensor carpi ulnaris (ECU) is easier to find distal to the retinaculum. The ECU is shortened by imbrication after centralization, and the ECR is divided at its insertion to facilitate later transfer to the ECU (Fig. 41-7).
The extensor carpi ulnaris (ECU) is easier to find distal to the retinaculum. The ECU is shortened by imbrication after centralization, and the ECR is divided at its insertion to facilitate later transfer to the ECU (Fig. 41-7).
Step 4: Ulnocarpal Joint Reduction and Centralization
 The wrist capsule is opened distal to the ulnar physis, and a soft tissue release is carried out until the carpus can be brought over the distal ulna (Fig. 41-8).
The wrist capsule is opened distal to the ulnar physis, and a soft tissue release is carried out until the carpus can be brought over the distal ulna (Fig. 41-8).
 The carpus is mobilized off the palmar capsule until it can be reduced onto the distal ulna for centralization.
The carpus is mobilized off the palmar capsule until it can be reduced onto the distal ulna for centralization.
Step 4 Pearls
If the carpus cannot be reduced, the radial side of the wrist needs to be reexamined, and any radial fibrous bands should be divided to facilitate reduction of the carpus onto the ulna.
Occasionally, partial carpectomy or limited shaving of the carpus to create a notch in it for seating of the distal end of the ulna may be required to achieve reduction. However, it should be remembered that carpal bones are resected only if reduction is impossible, because excessive resection of the epiphysis will arrest growth. Rather than accepting this risk, preoperative soft tissue stretching using an external distractor is recommended in most cases.
Step 5: Fixation
Step 6: Wrist Stabilization
 The ECR tendon is transferred to the distal stump of the ECU passing below the EDC (see Fig. 41-3). The proximal end of the ECU is advanced and sutured to the dorsal wrist capsule. Tendon repairs are done using 2-0 Ethibond horizontal mattress sutures.
The ECR tendon is transferred to the distal stump of the ECU passing below the EDC (see Fig. 41-3). The proximal end of the ECU is advanced and sutured to the dorsal wrist capsule. Tendon repairs are done using 2-0 Ethibond horizontal mattress sutures.
 The extensor retinaculum is repaired using 4-0 Vicryl, and skin is closed with 4-0 chromic sutures (Fig. 41-10).
The extensor retinaculum is repaired using 4-0 Vicryl, and skin is closed with 4-0 chromic sutures (Fig. 41-10).
Postoperative Care and Expected Outcomes
 A long-arm cast with the elbow flexed to 90 degrees is provided. The extremity is immobilized for at least 8 weeks, and the pin is kept in place for as long as possible. A long-arm Orthoplast splint to maintain wrist position is worn full-time for 3 months and then at night until skeletal maturity. Prolonged pin fixation followed by long-term splinting is necessary to minimize recurrence.
A long-arm cast with the elbow flexed to 90 degrees is provided. The extremity is immobilized for at least 8 weeks, and the pin is kept in place for as long as possible. A long-arm Orthoplast splint to maintain wrist position is worn full-time for 3 months and then at night until skeletal maturity. Prolonged pin fixation followed by long-term splinting is necessary to minimize recurrence.
 Recurrence is the most common source of failure following centralization, and the cause appears to be multifactorial. Operative causes include the inability to obtain complete correction at surgery, inadequate radial soft tissue release, and failure to balance the radial force. Postoperative reasons consist of early pin removal, poor postoperative splint use, and the natural tendency for the shortened forearm and hand to deviate in a radial direction for hand-to-mouth use.
Recurrence is the most common source of failure following centralization, and the cause appears to be multifactorial. Operative causes include the inability to obtain complete correction at surgery, inadequate radial soft tissue release, and failure to balance the radial force. Postoperative reasons consist of early pin removal, poor postoperative splint use, and the natural tendency for the shortened forearm and hand to deviate in a radial direction for hand-to-mouth use.
 Even a successful centralization still results in a shortened forearm segment secondary to altered growth of the ulna (60% of normal). The short forearm is both a cosmetic and functional problem for the teenager with radial deficiency. Lengthening of the ulna can be accomplished using uniplanar or multiplanar shaft-distraction devices.
Even a successful centralization still results in a shortened forearm segment secondary to altered growth of the ulna (60% of normal). The short forearm is both a cosmetic and functional problem for the teenager with radial deficiency. Lengthening of the ulna can be accomplished using uniplanar or multiplanar shaft-distraction devices.