CHAPTER 40 Chronic Obstructive Pulmonary Disease
3 Describe chronic bronchitis and emphysema
 Chronic bronchitis: Characterized by cough, sputum production, recurrent infection, and airway obstruction for many months to several years. Patients with chronic bronchitis have mucous gland hyperplasia, mucus plugging, inflammation and edema, peribronchiolar fibrosis, airway narrowing, and bronchoconstriction. Decreased airway lumina caused by mucus and inflammation increase resistance to flow of gases.
Chronic bronchitis: Characterized by cough, sputum production, recurrent infection, and airway obstruction for many months to several years. Patients with chronic bronchitis have mucous gland hyperplasia, mucus plugging, inflammation and edema, peribronchiolar fibrosis, airway narrowing, and bronchoconstriction. Decreased airway lumina caused by mucus and inflammation increase resistance to flow of gases. Emphysema: Characterized by progressive dyspnea and variable cough. Destruction of the elastic and collagen network of alveolar walls without resultant fibrosis leads to abnormal enlargement of air spaces. In addition, the loss of airway support leads to airway narrowing and collapse during expiration (air trapping).
Emphysema: Characterized by progressive dyspnea and variable cough. Destruction of the elastic and collagen network of alveolar walls without resultant fibrosis leads to abnormal enlargement of air spaces. In addition, the loss of airway support leads to airway narrowing and collapse during expiration (air trapping).4 List contributory factors associated with the development of chronic obstructive pulmonary disease
 Smoking: Smoking impairs ciliary function, depresses alveolar macrophages; leads to increased mucous gland proliferation and mucus production; increases the inflammatory response in the lung; leading to increased proteolytic enzyme release; reduces surfactant integrity; and causes increased airway reactivity.
Smoking: Smoking impairs ciliary function, depresses alveolar macrophages; leads to increased mucous gland proliferation and mucus production; increases the inflammatory response in the lung; leading to increased proteolytic enzyme release; reduces surfactant integrity; and causes increased airway reactivity. Occupational and environmental exposure: Animal dander, toluene and other chemicals, various grains, cotton, and sulfur dioxide and nitrogen dioxide in air pollution.
Occupational and environmental exposure: Animal dander, toluene and other chemicals, various grains, cotton, and sulfur dioxide and nitrogen dioxide in air pollution. Recurrent infection: Bacterial, atypical organisms (mycoplasma), and viral (including human immunodeficiency virus, which can produce an emphysema-like picture).
Recurrent infection: Bacterial, atypical organisms (mycoplasma), and viral (including human immunodeficiency virus, which can produce an emphysema-like picture). Familial and genetic factors: A predisposition to COPD exists and is more common in men than women. α1-antitrypsin deficiency is a genetic disorder resulting in autodigestion of pulmonary tissue by proteases and should be suspected in younger patients with basilar bullae on chest x-ray film. Smoking accelerates its presentation and progression.
Familial and genetic factors: A predisposition to COPD exists and is more common in men than women. α1-antitrypsin deficiency is a genetic disorder resulting in autodigestion of pulmonary tissue by proteases and should be suspected in younger patients with basilar bullae on chest x-ray film. Smoking accelerates its presentation and progression.6 What features distinguish pink puffers from blue bloaters?
| Pink puffers (emphysema) | Blue bloaters (chronic bronchitis) |
| Usually older (>60 years) | Relatively young |
| Pink in color | Cyanotic |
| Thin | Heavier in weight |
| Minimal cough | Chronic productive cough; frequent wheeze |
8 What laboratory examinations are useful?
 Electrolytes: Bicarbonate levels are elevated to buffer a chronic respiratory acidosis if the patient retains carbon dioxide. Hypokalemia can occur with repeated use of β-adrenergic agonists.
Electrolytes: Bicarbonate levels are elevated to buffer a chronic respiratory acidosis if the patient retains carbon dioxide. Hypokalemia can occur with repeated use of β-adrenergic agonists. Chest x-ray film: Look for lung hyperinflation, bullae or blebs, flattened diaphragm, increased retrosternal air space, atelectasis, cardiac enlargement, infiltrate, effusion, masses, or pneumothorax.
Chest x-ray film: Look for lung hyperinflation, bullae or blebs, flattened diaphragm, increased retrosternal air space, atelectasis, cardiac enlargement, infiltrate, effusion, masses, or pneumothorax. Electrocardiogram: Look for decreased amplitude, signs of right atrial (peaked P waves in leads II and V1) or ventricular enlargement (right axis deviation, R/S ratio in V6 ≤1, increased R wave in V1 and V2, right bundle-branch block), and arrhythmias. Atrial arrhythmias are common, especially multifocal atrial tachycardia and atrial fibrillation.
Electrocardiogram: Look for decreased amplitude, signs of right atrial (peaked P waves in leads II and V1) or ventricular enlargement (right axis deviation, R/S ratio in V6 ≤1, increased R wave in V1 and V2, right bundle-branch block), and arrhythmias. Atrial arrhythmias are common, especially multifocal atrial tachycardia and atrial fibrillation.9 How does a chronically elevated arterial carbon dioxide partial pressure affect the respiratory drive in a person with chronic obstructive pulmonary disease?
12 What factors are associated with an increased perioperative morbidity or mortality?
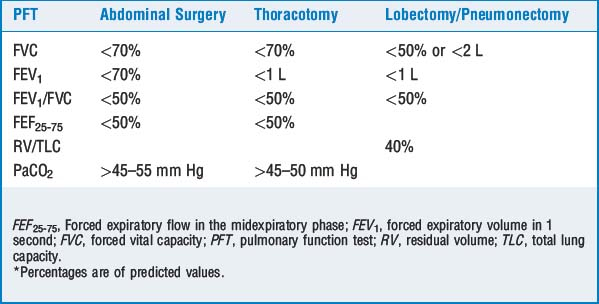
Patients presenting for lobectomy or pneumonectomy must have pulmonary function and arterial blood gas values that are superior to the values in Table 40-1. If any of the aforementioned criteria are not satisfied, further preoperative testing is indicated to determine the risk-benefit ratio for lung resection. Further tests include split-lung function, regional perfusion, regional ventilation, regional bronchial balloon occlusion, and pulmonary artery balloon occlusion studies. A forced expiratory volume in 1 second (FEV1) less than 800 ml in a 70-kg person is probably incompatible with life and is an absolute contraindication to lung resection because of the high incidence for extended mechanical ventilation.
13 List the common pharmacologic agents used to treat COPD and their mechanisms of action
TABLE 40-2 Agents used to Treat Chronic Obstructive Pulmonary Disease
| Class and Examples | Actions |
|---|---|
| β-Adrenergic agonists: albuterol, metaproterenol, fenoterol, terbutaline, epinephrine | Increases adenylate cyclase, increasing cAMP and decreasing smooth muscle tone (bronchodilation); short-acting β-adrenergic agonists (e.g., albuterol, terbutaline, and epinephrine) are the agents of choice for acute exacerbations |
| Methylxanthines: aminophylline, theophylline | Phosphodiesterase inhibition increases cAMP; potentiates endogenous catecholamines; improves diaphragmatic contractility; central respiratory stimulant |
| Corticosteroids: methylprednisolone, dexamethasone, prednisone, cortisol | Antiinflammatory and membrane stabilizing; inhibits histamine release; potentiates β-agonists |
| Anticholinergics: atropine, glycopyrrolate, ipratropium | Blocks acetylcholine at postganglionic receptors, decreasing cGMP, relaxing airway smooth muscle |
| Cromolyn sodium | Also a membrane stabilizer, preventing mast cell degranulation, but must be given prophylactically |
| Antileukotrienes: zileuton, montelukast | Inhibition of leukotriene production and/or zafirlukast, leukotriene antagonism; antiinflammatory; used in addition to corticosteroids; however, may be considered first-line antiinflammatory therapy for patients who cannot or will not use corticosteroids |
cAMP, Cyclic adenosine monophosphate; cGMP, cyclic guanosine monophosphate.
14 What therapies are available to reduce perioperative pulmonary risk?
 Stop smoking.
Stop smoking.
 Cessation for 48 hours before surgery decreases carboxyhemoglobin levels. The oxyhemoglobin dissociation curve shifts to the right, allowing increased tissue oxygen availability.
Cessation for 48 hours before surgery decreases carboxyhemoglobin levels. The oxyhemoglobin dissociation curve shifts to the right, allowing increased tissue oxygen availability.15 Do advantages exist with regional anesthesia techniques in patients with chronic obstructive pulmonary disease?
17 Discuss the particular concerns regarding muscle relaxation (and reversal) in patients with chronic obstructive pulmonary disease
19 Define auto-PEEP
KEY POINTS: Chronic Obstructive Pulmonary Disease 
21 How would you treat intraoperative bronchospasm?
 Administer 100% oxygen and manually ventilate, allowing sufficient expiratory time. Identify and correct the underlying condition as discussed in Question 20.
Administer 100% oxygen and manually ventilate, allowing sufficient expiratory time. Identify and correct the underlying condition as discussed in Question 20. Administer therapy:
Administer therapy:
 Increase the volatile anesthetic agents and/or administer intravenous lidocaine, ketamine, or propofol.
Increase the volatile anesthetic agents and/or administer intravenous lidocaine, ketamine, or propofol. Administer β-adrenergic agonists: aerosolized via the endotracheal tube (e.g., albuterol), subcutaneously (e.g., terbutaline), or intravenously (e.g., epinephrine or terbutaline).
Administer β-adrenergic agonists: aerosolized via the endotracheal tube (e.g., albuterol), subcutaneously (e.g., terbutaline), or intravenously (e.g., epinephrine or terbutaline).