CASE 40
1. What should be included in the differential diagnosis? (Choose all that apply.)
B. Cryptogenic organizing pneumonia
D. Acute respiratory distress syndrome
2. What is the predominant distribution of the lung opacity?
A. Basilar
B. Upper lobe
C. Peripheral
3. What is the most likely diagnosis?
B. Cryptogenic organizing pneumonia
D. Acute respiratory distress syndrome
4. What is the most likely etiology?
A. Cardiogenic
B. Neurogenic
ANSWERS
Reference
Eisenhuber E, Schaefer-Prokop CM, Prosch H, et al. Bedside chest radiography. Respir Care. 2012;57(3):427–443.
Cross-Reference
Cardiac Imaging: The REQUISITES, ed 3, p 18.
Comment
Pathophysiology and Etiology
Congestive heart failure can lead to pulmonary edema and pleural effusions. Pulmonary edema is related to both blood flow and blood pressure or to blood pressure alone. Elevation of pulmonary venous pressure can be secondary to left ventricular failure, mitral stenosis, and other causes of vascular obstruction distal to the pulmonary arterial bed.
Imaging Findings
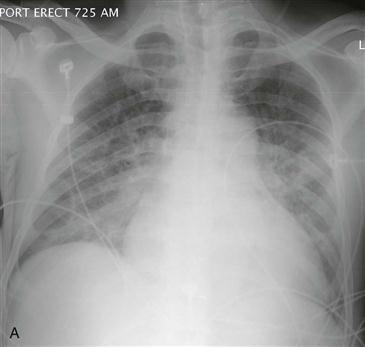
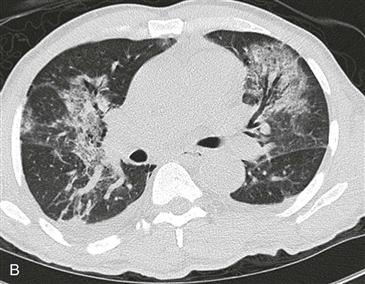
Patients with congestive heart failure typically have pulmonary edema, as evidenced by diffuse lung disease (Fig. A) or Kerley B lines on radiography. Early signs of pulmonary edema include subpleural thickening, best visualized along pulmonary fissures, and indistinct vessel margins. CT scan can show ground-glass opacity (Fig. B), interlobular septal thickening, and frank consolidation. The lung opacity is often perihilar or basilar predominant (or both). In patients with alveolar edema, there may be central opacities with sparing of the lung periphery—so-called bat-wing pulmonary edema. If the pulmonary edema is related to congestive heart failure, the cardiac silhouette is enlarged, and pleural effusions are often seen on chest radiography. The radiographic findings of pulmonary edema often persist for hours to days after symptom resolution.
Cephalization
Acute pulmonary edema rarely causes redistribution of blood flow to the lung apices—so-called cephalization. Cephalization is usually seen in patients with long-standing pulmonary venous hypertension and occurs most commonly in patients with chronic mitral stenosis or long-standing left heart failure.