CHAPTER 4. The person with type 2 diabetes
Derek Gordon
The metabolic syndrome 68
Why treat type 2 diabetes?68
Self-monitoring in type 2 diabetes 71
Non-drug treatment of type 2 diabetes 71
Pharmacological treatment of type 2 diabetes 74
Insulin therapy 84
Drugs of the future 88
Medications altering glucose tolerance and drug interactions 90
Conclusion 92
References 93
A WORLDWIDE EPIDEMIC
Type 2 diabetes has reached epidemic proportions both in developing countries and in the developed world. It is estimated that throughout the world there are currently 150 million people with diabetes, and that number will double by 2025. Globally, 97% of these people will have type 2 diabetes, although in the industrialised countries this figure falls to 90%.
In the UK, it is estimated there will be 2.88 million people with type 2 diabetes by 2010. Data from eight European countries indicate that the mean cost per patient with diabetes is US$2928 annually (1999 values), and the proportion of healthcare spending on diabetes ranges from 1.6% to 6.6%, depending on the country.
Changes in human lifestyle over the past century have precipitated this dramatic increase in the incidence of diabetes. Increasing prosperity, ready access to food – much of which is now ready-made, convenience food – and a more sedentary way of life have resulted in an explosion in the incidence of obesity. The Nurses’ Health Study found that in 91% of people with type 2 diabetes the condition could be attributed to a body mass index (BMI) > 23, lack of exercise, unhealthy diet, smoking and abstinence from alcohol (Hu et al 2001).
Obesity is associated with increased resistance to insulin action and the development of type 2 diabetes. Insulin resistance also increases with age and an ageing population has also contributed to the numbers of people with diabetes.
It is now recognised that insulin resistance is associated with a cluster of factors known as the ‘metabolic syndrome’. Overall obesity, and in particular central obesity, dyslipidaemia [characterised by elevated levels of triglycerides and low levels of high-density lipoprotein (HDL) cholesterol], hyperglycaemia and hypertension are common traits that, when they occur together, constitute the metabolic syndrome. The metabolic syndrome is very common, affecting about 24% of US adults between the ages of 20 and 70 years. People with the syndrome are about twice as likely to develop coronary heart disease as people without it.
It should, therefore, be recognised that type 2 diabetes is usually part of a more complex metabolic disorder and that treatment of the blood glucose levels should not be undertaken in isolation. It is important to tackle all aspects of the metabolic syndrome, that is, obesity, dyslipidaemia and hypertension. This chapter deals with the management of diabetes control; Chapter 8 covers the management of other cardiovascular risk factors.
THE PREDIABETIC STATE
The development of diabetes takes many years. The earliest feature in most people is the development of insulin resistance. The pancreas can initially compensate by producing more insulin and blood glucose levels can be maintained within normal limits. Eventually, however, the pancreas can no longer produce sufficient insulin to overcome the worsening insulin resistance and blood glucose levels begin to rise. At this stage people will have impaired glucose tolerance. Eventually the pancreatic beta cells begin to fail and insulin levels fall. This results in higher blood glucose concentrations and the development of diabetes.
THE SPECTRUM OF TYPE 2 DIABETES
Type 2 diabetes is therefore the result of both insulin resistance and insulin lack, hence people with type 2 diabetes form a classic spectrum of disease. At one end of the spectrum are obese people who have predominantly insulin resistance, at the opposite end are non-obese individuals with predominant insulin insufficiency.
WHY TREAT TYPE 2 DIABETES?
There are several reasons for treating the blood glucose concentrations in diabetes. Hyperglycaemia is associated with symptoms of lethargy, thirst and frequency of urination, including nocturia. Poorly controlled diabetes can lead to vaginal or penile thrush. Treatment of diabetes can relieve the symptoms of hyperglycaemia.
It had also been assumed for many years that control of blood glucose levels would prevent some of the complications of diabetes. This was demonstrated, for people with type 2 diabetes, when the results of the UK Prospective Diabetes Study (UK Prospective Diabetes Study (UKPDS) Group, 1998a and UK Prospective Diabetes Study (UKPDS) Group, 1998b) were published.
UK PROSPECTIVE DIABETES STUDY
The UK Prospective Diabetes Study (UKPDS) was a large, multicentre, clinical trial that started in 1977 and reported its final results in 1998. The aims of the study were to identify whether, in people with type 2 diabetes, tight metabolic control reduced the macrovascular and microvascular complications and whether any particular form of therapy was best in achieving tight control. In addition, the study aimed to demonstrate whether tight control of blood pressure prevented macro- and microvascular complications. The blood pressure control part of the study will not be discussed in this chapter.
During the course of the study, several UKPDS reports were published that revealed aspects of the epidemiology and natural history of type 2 diabetes. The study followed 3867 people with newly diagnosed type 2 diabetes. Individuals were randomly assigned to conventional treatment (the aim of which was to maintain fasting blood glucose at < 15 mmol/L) or intensive treatment (the aim of which was to achieve fasting blood glucose levels < 6 mmol/L).
People were allocated to treatment by diet, a sulphonylurea or insulin therapy. In addition, a small subgroup of obese individuals was allocated to initial treatment with metformin.
Results of the UKPDS
The study demonstrated that in both the conventional and intensive treatment groups, there was a steady increase in fasting blood glucose and glycated haemoglobin (HbA1c) over the period of the study. Type 2 diabetes is therefore a progressive disease associated with worsening metabolic control over a number of years (Fig. 4.1). This implies that metabolic control can be maintained in type 2 diabetes only by progressive increases in doses of medications and the utilisation of multiple therapies, including insulin. The different treatment modalities showed little difference on their effect on fasting blood glucose or HbA1c. Only people treated with chlorpropamide had significantly improved metabolic control when compared with other sulphonylureas or insulin.
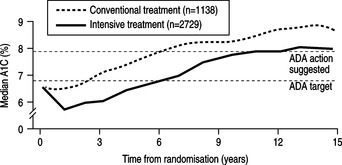 |
| Fig. 4.1HbA1c rises with time in both the conventional and the intensively treated groups of patients with type 2 diabetes.Reprinted from UKPDS (1998a), with permission from Elsevier. |
The intensively treated group showed an 11% reduction in HbA1c when compared to the conventional group (HbA1c 7.0% compared to 7.9%). For every 1% increment in HbA1c the study demonstrated a:
▪ 21% increased risk of any diabetes-related endpoint
▪ 21% increased risk of any diabetes-related death
▪ 14% increased risk of a myocardial infarction (MI)
▪ 37% increased risk of any microvascular complication.
Furthermore, the UKPDS (1998a) demonstrated that benefits could be achieved by reducing HbA1c results no matter how low they were to start with; in other words the lower the HbA1c the better. Microvascular risk became low when HbA1c reached levels of 7–8% whereas macrovascular risk continued to fall, down to HbA1c levels of 6–7%.
The difference in HbA1c results between the conventional and intensive treatment groups was associated with a significantly reduced frequency of microvascular endpoints; the reduction in diabetes-related mortality or macrovascular endpoints did not quite reach statistical significance. However, the group of obese people who were treated intensively with metformin showed a significant reduction in cardiovascular risk.
Metformin was the only treatment that was not associated with weight gain and raised circulating concentrations of plasma insulin. Sulphonylureas and insulin treatments were associated with increased plasma insulin concentrations and insulin resistance, and this might therefore have accounted for their poorer influence on long-term cardiovascular morbidity.
SELF-MONITORING IN TYPE 2 DIABETES
There is no evidence that blood or urine testing improves HbA1c, body weight or the incidence of hypoglycaemic events in people with type 2 diabetes. The National Institute for Health and Clinical Excellence (NICE) does not recommend the use of self-monitoring as a stand-alone intervention in people with type 2 diabetes (NICE 2004). Rather, it recommends that self-monitoring be taught only if the purpose or need for it is clear and agreed with the individual with diabetes.
Self-monitoring can be useful in the period immediately after diagnosis, when people can learn the effects of various foodstuffs on their blood or urine glucose levels. This can sometimes be effective in encouraging alterations to diet. It can be useful to teach self-monitoring to people in whom oral hypoglycaemic agents are failing; this can act as an incentive to improve control. Also, if they subsequently require insulin treatment they will already have mastered the technique prior to starting insulin. No doubt there are other situations when self-monitoring can be useful. However, prolonged self-monitoring with no clear purpose is an expensive practice that may not be beneficial. See Chapter 7 for further elaboration.
NON-DRUG TREATMENT OF TYPE 2 DIABETES
DIET
Dietary review is fundamental to the management of the person with type 2 diabetes. The basic tenets of dietary management should therefore be known to the primary healthcare team so that preliminary advice can be given in the community at the time of diagnosis (see Chapter 6). However, few doctors or nurses have adequate training to provide complete dietary advice and all newly diagnosed people should receive advice from a dietician.
Well over 50% of all newly diagnosed people with type 2 diabetes are overweight (BMI 25–30 kg/m2) or obese (BMI > 30 kg/m2). The cornerstone to their diet is an individualised reduced-calorie diet (see Chapter 6). Eating less reduces energy intake and allows weight reduction. Weight reduction will improve insulin resistance and allow the person to utilise his or her own insulin production more effectively.
When diet succeeds, the benefits are evident. Blood glucose, lipids and blood pressure fall. However, the response to diet is often disappointing. Most diabetic clinics in general practice or hospital lack the resources required to allow frequent dietary review and people often lack motivation or find it impossible to alter deeply ingrained eating habits. The UKPDS found that only 16% of newly diagnosed people with type 2 diabetes achieved near-normal fasting blood glucose concentrations after 3 months of dieting. Those people with the highest fasting blood glucose levels at the time of diagnosis were least likely to achieve good diabetic control by diet alone (UKPDS 1990).
EXERCISE
Several studies have demonstrated the benefit of lifestyle intervention on the development and management of diabetes. Modest weight loss and increased physical activity have been shown to cause substantial reduction in the risk of developing type 2 diabetes (Helmrich et al 1991, Manson et al 1991). For each 500-kcal increment in weekly energy expenditure, the risk of developing type 2 diabetes can be reduced by 6%.
Decreased cardiac risk
Exercise confers the well-established benefit of improved insulin sensitivity for people with or without diabetes. As with weight loss, improved insulin sensitivity is associated with reduction in blood pressure and improvement in lipid profiles, thus reducing cardiovascular risk. Improved fitness and exercise are associated with a reduction in coronary disease in the general population, but evidence for such a decrease among people with diabetes has not appeared.
Weight loss
The addition of exercise training to a conventional diet has been shown to be beneficial (Blonk 1994) with people showing greater weight loss and improved HbA1c. However, weight loss tends to be modest in most people and only a minority maintain their weight loss over a 3-year period (Stevens et al 2001).
Improved glucose utilisation
Increased insulin sensitivity allows glucose to enter muscle cells more efficiently both acutely and chronically with exercise. Improvements in glucose tolerance testing have been shown in type 2 diabetes after as little as 1 week of aerobic training. Increased insulin sensitivity begins to decline however, in as little as 1 or 2 days without exercise.
Exercise can therefore improve diabetic control and allow lower doses of oral hypoglycaemic drugs or insulin. However, the exercise must be maintained and this requires both self-motivation by the individuals and continuing encouragement by their families, friends and health carers. The optimal methods for maintaining motivation are still to be identified.
Bernard is a 52-year-old taxi driver who was recently diagnosed as having type 2 diabetes when he attended his GP complaining of tiredness and thirst. A random blood glucose was found to be 23 mmol/L. He has been overweight for many years and currently weighs 107 kg (BMI 34 kg/m2). When working, he eats erratically from cheap hot-food stalls. He smokes 30 cigarettes per day and never takes any exercise. His GP estimates his weekly alcohol intake at approximately 28 units. His mother and two brothers have type 2 diabetes.
Despite adherence to a restricted-calorie diet for 6 months and some increase in his exercise activities, Bernard continues to complain of thirst and frequency of urination during the night. His weight has fallen by 4 kg but his HbA1c remains elevated at 9.2%. His GP decides to start him on metformin.
The finding of a random blood glucose above 11.1 mmol/L in a person with osmotic symptoms confirms diabetes. Bernard’s elevated blood glucose might be the cause of his lethargy. In addition to his diabetes, his unhealthy lifestyle will further increase his risk of vascular catastrophe in the future unless he makes major alterations to the way he lives.
Bernard’s case history is fairly typical of the person with type 2 diabetes. There is a strong family history of diabetes and he has the associated risk factor of being overweight. He is likely to have other features of the metabolic syndrome; namely hypertension and hyperlipidaemia. His initial management will involve appropriate changes to his lifestyle including diet and exercise.
As Bernard has a sedentary lifestyle, he should be encouraged to increase his exercise activity. It is recommended that all individuals (including those with diabetes) undertake aerobic physical activity on a minimum of 3 days per week with sessions lasting 20–60 minutes. However, our 52-year-old taxi driver might have to start with low intensity exercise for shorter periods of time. In some areas of the UK, general practitioners can prescribe an exercise programme at a local gym. It is important to undertake a pre-exercise assessment of people with diabetes prior to entry into any such programme. Watch for signs and symptoms of peripheral vascular disease, such as intermittent claudication, cold feet, decreased or absent peripheral pulses. Diminished light touch, pin-prick or vibration sense might signal a peripheral neuropathy. Such people might be at risk of foot ulceration if asked to undertake exercise. Eyes should be examined to identify new vessel formation (see Chapter 9).
A history of postural hypotension, hypoglycaemia unawareness, gustatory sweating or impotence might signal the presence of autonomic neuropathy which, if present, could make exercise dangerous because of risks to the heart.
An exercise stress test is recommended for people at risk of heart disease who anticipate engaging in moderate to intense exercise. Among people with diabetes who are considered at risk are those who are older than 35 years, who have had type 2 diabetes for longer than 10 years and those who have had type 1 diabetes for longer than 15 years.
PHARMACOLOGICAL TREATMENT OF TYPE 2 DIABETES
METFORMIN: A BIGUANIDE
In medieval times, the plant, Galega officialis, (goat’s rue or French lilac) was used as a traditional remedy for diabetes in Southern and Eastern Europe. The plant was subsequently shown to be rich in guanidine and in 1918 guanidine was shown to have mild hypoglycaemic effects. However, guanidine was too toxic for clinical use and in the 1950s the biguanide, metformin, was derived and introduced into clinical practice.
Metformin lowers blood glucose concentrations by several mechanisms. Its most important effect is to enhance insulin sensitivity in peripheral tissues, in particular the liver and skeletal muscles. By improving insulin action on the liver, metformin inhibits glucose production and release. It also stimulates insulin uptake by skeletal muscle. It might have direct or indirect effects on reducing appetite (Bailey 1992).
The UKPDS included a subgroup of overweight people who were allocated to treatment with metformin, sulphonylureas (chlorpropamide or glibenclamide) or insulin therapy. Only metformin therapy was associated with improved insulin sensitivity and reduced circulating concentrations of insulin.
Reduced insulin resistance would be expected to improve cardiovascular risk and, indeed, the UKPDS showed that metformin had the greatest effects on any diabetes-related end point, on overall mortality due to any cause and also on the incidence of stroke. The UKPDS also reported that, in overweight people, metformin was not associated with weight gain and produced fewer hypoglycaemic attacks than sulphonylureas or insulin therapy (UKPDS 1998b). It is therefore recommended that metformin is used as first-line treatment in overweight people if lifestyle changes fail to improve diabetic control.
Metformin is likely to reduce blood glucose concentrations by 2–3 mmol/L when prescribed for people in whom diet has failed. This is a comparable blood glucose lowering effect to sulphonylureas. About 30% of people so treated will achieve good diabetic control. However, in a further 5–10% of people per year, metformin treatment will fail to achieve adequate control.
Prescribing metformin
Metformin is available in the UK as 500- and 850-mg tablets. The drug should be taken with meals and the dose increased gradually to lessen side effects. A typical starting dose would be 850 mg once daily or 500 mg once or twice daily. The dosage can be increased in a stepwise fashion over a period of several weeks to prevent adverse drug effects. Garber et al (1997) showed that metformin lowered HbA1c and fasting blood glucose in a dose-related manner, up to 2000 mg per day. Beyond this dosage there is little therapeutic gain but a much higher incidence of side effects.
Side effects of metformin
The most common side effects of metformin are gastrointestinal in origin. About 20% of people experience diarrhoea, flatulence or abdominal pain, whereas others complain of a metallic taste, nausea or anorexia. Although a reduction in appetite might be desirable in the overweight person, for the sake of compliance any nausea or anorexia must be considered seriously. These disturbances are generally transient and can be minimised by starting treatment at a low dosage and taking the drug with food.
Metformin can cause the blood lactate levels to rise. However, if it is prescribed taking into account recognised contraindications, there is no increased risk of serious lactic acidosis or increased levels of lactate compared to other antihyperglycaemic agents (Aguilar et al 1992). Metformin is normally excreted through the kidneys and is contraindicated in people with impaired renal function (e.g. serum creatinine > 130 micromol/L) as this can result in accumulation of the drug in the body, enhancing its effect on lactate production. Liver disease is also a contraindication, because adequate hepatic function is required to metabolise the increased lactic acid. People with cardiac failure perfuse their tissues poorly and the resulting tissue hypoxia causes lactic acid production. It is therefore unwise to prescribe metformin for such individuals. Metformin should be temporarily withdrawn in people undergoing surgery or radiology procedures requiring injection of contrast.
Annie is a 62-year-old housewife who has had type 2 diabetes for 10 years and was initially managed on diet alone. After 3 years her metabolic control deteriorated and as she was obese (BMI 31 kg/m2), metformin was started at an initial dose of 500 mg daily. Gradually, over a number of years, the dose was increased to 1 g twice daily. Over the past 3 months Annie has developed thirst and she has begun to monitor her urine for glycosuria. This has shown persistently elevated results. She denies any recent change to her diet. A clinic HbA1c result is 9.5%, confirming recent poor control.
Before making additions to Annie’s current therapy, it is important to determine if she is actually taking her current prescribed medication. Further dietary assessment should also be undertaken to determine her understanding, identify any necessary changes to be made and to assess her motivation and adherence.
One of the most important findings of the UKPDS was the demonstration that type 2 diabetes is a progressive condition. All modalities of therapy were associated with a relentless rise in HbA1c with duration of disease (see Fig. 4.1). This results in the need for increasing doses of medication and the introduction of multiple therapies to maintain diabetic control. UKPDS (1990) suggested that 3 years after diagnosis approximately half of people controlled on diet alone were failing in their control and required more than one glucose-lowering drug. After 9 years this increased to 75% of people requiring multiple therapies to achieve HbA1c levels averaging 7.0%. Following the failure of metformin to control Annie’s diabetes, the introduction of an insulin secretogogue is recommended (NICE 2004).
INSULIN SECRETOGOGUES
The sulphonylureas
Sulphonylureas have been used to treat type 2 diabetes for more than 50 years. In recent years, understanding of their mode of action has developed. Sulphonylureas bind to cell membrane receptors on the beta cell. This causes the potassium channel across the membrane to close and the membrane to depolarise. In turn, this causes calcium influx and insulin granule release into the extracellular medium. Therefore the effect of sulphonylureas is limited to people with preserved pancreatic cell function. The pancreas can only be squeezed to produce more insulin if there are functioning beta cells there to be squeezed!
It is generally recommended that sulphonylureas are ingested about 30 minutes before meals as this will stimulate insulin production to coincide with the time of eating. This in turn has been shown to reduce the postprandial rise in blood glucose (Melander et al 1989). Most drugs in this group are given twice daily when used at higher doses. The maximum therapeutic effect of most sulphonylureas is achieved at relatively low doses. This is likely to be due to cell receptors for the drug becoming saturated at low doses and further increases in drug dose have no additional effects. A person who shows poor glycaemic control on a dose of gliclazide 160 mg daily or glibenclamide or glipizide 10 mg daily is unlikely to respond optimally to higher doses and a decision to start additional therapy should not be delayed unnecessarily.
Which agent to use?
There are very few studies of the older sulphonylureas such as tolbutamide. For the more recently introduced sulphonylureas there is little evidence that one compound is more effective than another and little to be gained by changing from one agent to another (Gordon 1996).
Nevertheless, there are important differences between the sulphonylureas, in particular their duration of effect (Table 4.1). The shorter-acting sulphonylureas require more frequent dosing, with consequent influence on concordance with treatment (see below). The longer-acting sulphonylureas – glibenclamide and chlorpropamide – are associated with a higher incidence of severe hypoglycaemic attacks (Gordon 1996).
| Drug | Effect duration (hours) | Daily dose (mg) |
|---|---|---|
| tolbutamide | 6–10 | 500–2000 |
| gliquidone | 6–18 | 15–180 |
| gliclazide | 12–20 | 40–320 |
| glipizide | 6–16 | 2.5–20 |
| glimepiride | 12– > 24 | 1–6 |
| glibenclamide | 12– > 24 | 2.5–20 |
| chlorpropamide | 24–72 | 100–500 |
Glimepiride is the most recently introduced sulphonylurea and can be prescribed as a once-daily preparation even at higher dosage (Sonnenberg et al 1997). The starting dose is usually 1 mg daily and this can be increased in 1-mg steps every 1–2 weeks to the usual maximum dose of 6 mg. Glimepiride has been shown to be less likely to cause symptomatic hypoglycaemia than glibenclamide (Dills & Schneider 1996).
These agents tend to cause weight gain and should only be used in obese patients when dietary restriction and metformin therapy have proved inadequate in controlling blood glucose levels.
The most important side effect with sulphonylureas is the development of serious and prolonged hypoglycaemia. For this reason, any person who becomes hypoglycaemic due to a sulphonylurea should be admitted to hospital for at least 24 hours for observation. The elderly are most at risk, probably because of coexisting vascular disease of the brain and heart. Almost all causes of prolonged hypoglycaemia have involved people over the age of 70 years (Ferner & Neil 1988). Of those admitted to hospital, 10% will die and 3% will be left with permanent brain damage. The longer-acting sulphonylureas should be avoided in the elderly.
The short-acting tolbutamide can be used in renal impairment, as can gliquidone and gliclazide, which are mainly metabolised and inactivated by the liver. However, care should be taken to monitor blood glucose levels regularly in order to avoid hypoglycaemia.
Sulphonylurea failure
As type 2 diabetes progresses, beta-cell function deteriorates further and the ability of the sulphonylureas to stimulate insulin secretion also deteriorates. Indeed, by ‘flogging a dying horse’ it is possible that the sulphonylureas might actually hasten the demise of the beta cell. Harrower and Wong (1990) reported 5-year failure rates for gliclazide at 7%, glibenclamide 17.9% and glipizide 25.6%.
SHORT-ACTING INSULIN SECRETOGOGUES
The glinides (meglitinides and D-phenylalanine derivatives)
Glinides, such as repaglinide and nateglinide, are recently introduced insulin secretogogues. Like the sulphonylureas, they bind to the sulphonylurea receptor on the surface of the beta cell. The binding, however, occurs at a different position on the sulphonylurea receptor. Nevertheless, their action is similar to that of the sulphonylureas, causing closure of the transmembrane, potassium channel and subsequent release of insulin from the beta cell.
These drugs are short acting and should be taken before main meals. Their function is mainly to reduce postprandial rises in blood glucose. There is some evidence to support the hypothesis that rapid rises in blood glucose levels are particularly important in the development of diabetic complications. Therefore, drugs that can reduce postprandial glucose excursions might be important in reducing the morbidity and mortality associated with diabetes. However, this theory is at present unproven and controversial.
Repaglinide
Repaglinide is the first meglitinide to become available for clinical use. It is taken before meals at doses of 0.5–4 mg. Studies have shown that repaglinide as monotherapy or in combination with other hypoglycaemic agents such as metformin or rosiglitazone (see below) achieves good metabolic control similar to that achieved by glibenclamide regimens. Repaglinide is associated with less severe and less frequent hypoglycaemic events than sulphonylureas. There is some evidence that repaglinide is less likely to cause weight gain than various sulphonylureas.
Nateglinide
Nateglinide is a d-phenylalanine derivative and is taken before meals at a dose of 60–120 mg. It is not licensed as monotherapy and should be used in combination with metformin. Studies with nateglinide have shown that, compared with glibenclamide, the hypoglycaemic effects of nateglinide are more rapid and greater, while producing less prolonged insulin exposure and less risk of hypoglycaemia. When nateglinide was compared to glipizide, a shorter-acting sulphonylurea, both agents showed similar postprandial glucose excursions. Glipizide produced lower blood glucose levels 4 hours after meals with therefore an increased risk of late hypoglycaemia.
The glinides need to be taken three times a day and therefore compliance with therapy can be reduced. Their exact place in the management of type 2 diabetes remains to be established. They can be particularly suitable for people with erratic lifestyles for whom mealtimes are unpredictable. They might be suitable hypoglycaemic agents for elderly people in whom hypoglycaemia is a concern and for those individuals with renal or mild hepatic failure.
THE THIAZOLIDINEDIONES (ALSO KNOWN AS GLITAZONES)
The mode of action of the thiazolidinediones is complex and not fully understood. They bind to a nuclear protein called peroxisome proliferator-activated receptor-γ (PPARγ), a nuclear receptor found mainly in fat cells but also in muscle and liver. Binding of thiazolidinediones to this receptor protein switches on several genes that are involved mainly with lipid metabolism (Tontonoz et al 1994, Vidal-Puig et al 1997). The net effect of the stimulation of these genes is to reduce circulating levels of fatty acids that are known to be responsible for causing insulin resistance. Also, binding to the PPARγ receptor decreases production of tumour necrosis factor α (TNFα) and of resistin, both of which are involved in causing insulin resistance. The main effect of the thiazolidinediones is therefore to reduce peripheral insulin resistance.
Two glitazones are currently available: rosiglitazone and pioglitazone. Rosiglitazone is available in two doses, 4 and 8 mg, whereas pioglitazone is available in doses of 15, 30 and 45 mg. They have been used as monotherapy in the USA for several years and recently gained licences for monotherapy in the UK. Because these drugs work by switching on genes, their full effect is not felt for 6–10 weeks. Doses should therefore be increased after intervals of 6–8 weeks.
Thiazolidinediones are associated with weight gain. There is evidence, however, that the weight is redistributed so that there is less central obesity; a situation that is associated with improved insulin sensitivity. Their use is also associated with fluid retention and they are therefore contraindicated in people with cardiac failure or severe renal impairment.
Thiazolidinediones have been shown to sustain glycaemic control over a 2-year period (Jariwala et al 2003). A comparison of pioglitazone with gliclazide demonstrated that the time to failure of glycaemic control was significantly longer with pioglitazone. The thiazolidinediones have a greater effect on peripheral insulin resistance than metformin (Mathews et al 1999, Rosenstock 2000) and the hope is that they will prove to be better drugs for preventing the long-term macrovascular complications of type 2 diabetes. Several studies of morbidity and mortality outcomes are currently underway and will report in the next few years. If these studies confirm beneficial cardiovascular effects for this group of drugs then they are likely to become more widely used.
Eithne is a 48-year-old social worker who has had type 2 diabetes for 7 years. Her BMI at diagnosis was 28 kg/m2 and she was initially started on metformin therapy. However, she was able to tolerate only the lowest dose of metformin 500 mg daily. Doses greater than this caused unacceptable symptoms of abdominal pain and diarrhoea. As her metabolic control remained poor, a sulphonylurea, glipizide was added to her oral regimen. In recent years, her diabetic control has deteriorated and her dose of glipizide has gradually increased to maximum. Despite this, her most recent HbA1c is 10.3%. Her consultant decides that she requires further oral therapy in the form of rosiglitazone at an initial dose of 4 mg daily. Her metformin is withdrawn while the glipizide is continued.
The thiazolidinediones are often used in the UK in circumstances where metformin is contraindicated or poorly tolerated. In Eithne’s situation, metformin has caused unacceptable side effects at increased dosage. The addition of a thiazolidenedione to a sulphonylurea has been shown to improve metabolic control and prolong the time until insulin therapy is required. Withdrawal of metformin might result in an initial worsening of metabolic control because the therapeutic effect of rosiglitazone may take several weeks to develop. Eithne would be advised of this at the time of the medication change over and would require close monitoring.
ALPHA-GLUCOSIDASE INHIBITORS
Acarbose is the only drug of this class available in the UK. Alpha-glucosidases are enzymes that line the gut wall and are required for the absorption of various carbohydrates. Inhibition of these enzymes by acarbose results in delayed absorption of carbohydrate.
Acarbose should be prescribed at an initial dose of 50 mg daily to minimise side effects (see below). The dose can be increased to 50 mg three times daily, then increased if necessary after 6–8 weeks to 100 mg three times per day. The maximum dose is 200 mg thrice daily. The tablets should be chewed with the first mouthful of food or swallowed immediately before food.
Acarbose does not cause hypoglycaemia itself but, when used in combination with insulin or insulin secretogogues, hypoglycaemia can occur. People should be warned that they need to carry glucose and not sucrose with them to treat hypoglycaemic episodes. This is because acarbose interferes with sucrose absorption from the gut.
Several studies have shown that acarbose can reduce postprandial hyperglycaemia (Lindstrom et al 2000, Scorpiglione et al 1999) as well as HbA1c levels by generally small amounts (Chan et al 1998, Holman et al 1999, Scott et al 1999).
However, acarbose is poorly tolerated and there is a high incidence of gastrointestinal side effects, mainly flatulence, abdominal pain and diarrhoea. Several studies have demonstrated high drop-out rates because of side effects (Chan et al 1998, Holman et al 1999) and these findings have led NICE (2004) to recommend that acarbose should probably only be considered for people who cannot tolerate other oral glucose-lowering therapies.
CONCORDANCE
NICE (2004) defines concordance as being:
… concerned with the extent to which an individual’s behaviour, in terms of lifestyle practices and medication taking, coincides with medical or health advice.
In the management of diabetes, the emphasis is on individual empowerment and partnership between people and healthcare professionals. The term ‘concordance’ recognises this more equitable relationship and is now the preferred expression, as opposed to either compliance or adherence.
The Diabetes Audit and Research Tayside Study
The Diabetes Audit and Research in Tayside Scotland (DARTS) programme has added substantially to our understanding of concordance with drug therapy for people with type 2 diabetes. Using information obtained from dispensed prescription data from community pharmacies, Donnan and colleagues (2002) were able to derive adherence indices for individuals taking sulphonylureas or metformin as monotherapy. Adequate adherence was defined as the amount of drug dispensed being ≥ 90% of individuals’ requirements. The authors were able to show that adequate adherence was found in only one in three people with type 2 diabetes receiving a single oral hypoglycaemic agent. Adherence was poorer with an increasing daily number of tablets for both sulphonylurea and metformin, with only one in four people remaining adherent when treatment involved more than once daily dosing. Adherence also fell as the number of co-medications rose. Poorer adherence was also associated with more socially deprived groups.
The data from the DARTS project (Donnan et al 2002) have encouraged pharmaceutical companies to develop long-standing, once-a-day preparations and combination drugs to improve concordance by individuals with diabetes.
MODIFIED-RELEASE MEDICATIONS
Diamicron MR is a slow-release preparation of gliclazide. It is prescribed as a once-daily medication and it is hoped that this will improve concordance. Preliminary studies with Diamicron MR have shown that HbA1c can be improved following conversion from conventional gliclazide to the long-acting preparation. Diamicron MR is also associated with a decreased incidence of hypoglycaemic events.
A slow-release preparation of metformin, Glucophage SR is available and may be associated with fewer gastorintestinal side effects.
COMBINATION DRUGS
Avandamet is currently available in the UK. This drug is a combination of metformin and rosiglitazone and is available in a number of dose variations. Combination treatments are expected to improve concordance for people with type 2 diabetes who are on multiple drug regimens.
Similarly Competact is a combination of metformin and pioglitazone which has recently gained marketing authorisation in Europe.
ANTI-OBESITY DRUGS
Anti-obesity drugs should be used only as part of a comprehensive weight-management programme, with frequently reinforced guidance on diet, exercise and healthy living. These agents should only be considered when people have a BMI > 30 kg/m2 and when at least 3 months of lifestyle intervention has failed to induce weight loss. In the presence of comorbidity such as diabetes, coronary heart disease, hypertension or obstructive sleep apnoea, anti-obesity drugs can be used for individuals with BMI > 28 kg/m2. Drug treatment should be withdrawn if weight loss is insignificant (< 5% initial body weight after 3 months) or if there is weight gain at any time while receiving drug treatment.
Orlistat
Orlistat is a pancreatic lipase inhibitor. Lipases are required to break down fats before they can be absorbed from the gastrointestinal tract. Weight loss therefore occurs by reducing the absorption of fat from the diet by about 30%. Orlistat is licensed for use in the UK in conjunction with a mildly hypocaloric diet in those with BMI of > 30 kg/m2. It can also be used in those with a BMI of 28 kg/m2 or greater and associated risk factors such as diabetes. Treatment should only be started if a low-fat diet has previously produced a weight loss of 2.5 kg over a period of four consecutive weeks. Orlistat is prescribed at a dose of 120 mg before, during or up to 1 hour after main meals.
Several studies have shown that orlistat in conjunction with a hypocalorific diet causes increased weight loss, when compared with placebo, in obese people with type 2 diabetes treated by diet alone, metformin, sulphonylureas or insulin. This effect is seen in studies lasting as long as 1 year (Greenway 1999, Halpern et al 2003Hanefeld & Sachse 2002). Similarly, these studies have demonstrated that people treated with orlistat have significant improvements in HbA1c, fasting glucose and postprandial glucose levels.
Orlistat and dyslipidaemia
There is now a significant body of evidence that demonstrates the effect of orlistat on lipid profiles. Orlistat has been shown to cause significant reductions in total cholesterol, low-density lipoprotein (LDL) cholesterol and fasting free fatty acids. The reduction in circulating free fatty acids was associated with a reduction in insulin resistance (Kelley et al., 2002 and Kelley et al., 2004).
Orlistat and blood pressure
Orlistat has also been shown to produce modest reductions in systolic blood pressure in people with type 2 diabetes when compared to placebo (Miles et al 2002, Tong et al 2002). This contrasts with sibutramine (see below) and might prove to be of clinical significance.
Orlistat and the prevention of diabetes
The XENDOS study (Torgeson et al 2004) has reported results that show that the modest weight loss achieved with orlistat in people with impaired glucose tolerance can delay the development of diabetes over a 4-year period.
Sibutramine
Sibutramine is a centrally acting drug that prolongs the action of the neurotransmitters serotonin and noradrenaline by blocking their reuptake at nerve endings. This results in the induction of premature satiety and the maintenance of thermogenic energy expenditure. Sibutramine therefore helps to prevent the reduction in energy expenditure that normally occurs during dieting.
Several studies have demonstrated the ability of sibutramine to improve both weight loss and diabetic control in overweight and obese people with type 2 diabetes (Finer et al 2000, Fujioka et al 2000, Serrano-Rios et al 2002). The improvement in glycaemic control was generally commensurate with the amount of weight loss. In general, reductions in HbA1c were < 0.5% but could be > 1% for people achieving substantial weight loss.
The ability of sibutramine to maintain weight loss has been demonstrated in several trials. For example, a multicentre French trial started individuals on a very low calorie diet for 1 month before randomising people to sibutramine or placebo. After 12 months the sibutramine group had lost a further 5 kg whereas the placebo group had regained 0.5 kg (Apfelbaum et al 1999).
Sibutramine and dyslipidaemia
Sibutramine treatment has been shown to improve the typical pattern of dyslipidaemia seen in obese people or those with diabetes (i.e. raised triglycerides and low HDL cholesterol). The reduction in triglycerides and the increase in HDL cholesterol achieved by sibutramine is in excess of that seen by equivalent weight reduction by diet alone (Dujovne et al 2001).
Sibutramine and blood pressure
Sibutramine can cause small increases in blood pressure and heart rate, probably by means of its central, inhibitory action on noradrenaline reuptake. This drug is therefore contraindicated in people with uncontrolled hypertension. However, if blood pressure is well controlled, studies have shown no detrimental cardiovascular effects (Faria et al 2002, Hazenburg 2000, McMahon et al 2000, Sharma 2001). However, NICE guidelines (2004) suggest that the detrimental effect of sibutramine on blood pressure negates the beneficial effects of weight loss on cardiovascular outcomes.
Rimonabant is a selective cannabinoid type 1 receptor blocker which has recently been introduced. In combination with an energy-restricted diet and exercise this can reduce bodyweight and HbA1c in obese persons with type 2 diabetes inadequately controlled on metformin or sulphonylurea (Scheen et al 2006).
LONG-TERM SAFETY
Dexfenfluramine (a stimulator of serotonin release) and phentermine (a stimulator of noradrenaline release) have been withdrawn from clinical use because of serious side effects; in particular cardiac valve disease and pulmonary hypertension. These complications have not been identified in people on sibutramine treatment.
INSULIN THERAPY
Margaret is a 68-year-old woman who has had type 2 diabetes for 5 years. She was treated initially by diet alone and subsequently with a sulphonylurea. Her control has never been good and 6 months ago metformin was introduced. She has never been overweight and she has lost 4 kg in weight over the past 6 months. She is symptomatic, with polydipsia and nocturia. The need for insulin therapy has been discussed with her on several occasions but she is reluctant to consider this option.
Many people have a deep-seated fear of self-injection and are understandably reluctant to consider insulin treatment. It can be explained that insulin will be given for a trial period and can subsequently be withdrawn if the person so wishes. This often reassures the individual, who feels that the introduction of insulin treatment is a ‘life sentence’. Most people requiring insulin therapy are tired and lethargic, although they might not appreciate the significance of these symptoms, attributing them to old age. It is important to point out to the doubting person that insulin therapy can give them a new lease of life. Most people started on insulin treatment feel a lot better: their symptoms of polydipsia and polyuria recede, they regain lost weight and they generally feel more energetic. Most people ‘never look back’ after starting insulin therapy and do not contemplate reverting to oral treatments.
INSULIN TREATMENT IN THE ELDERLY
It should be remembered that starting elderly people on insulin treatment can have far-reaching consequences. Many elderly people are unable to learn the technique of self-injection. There can be several reasons for this: failing eyesight, poor muscle coordination due to cerebrovascular disease or degenerative diseases, arthritis or the inability to grasp new concepts may limit the ability of the individual to undertake self injection. Under these circumstances, the person becomes dependent on a relative or healthcare worker for insulin treatment. A previously independent person can therefore be rendered dependent on others. This loss of independence can be associated with a reduction in self-esteem and the development of depression.
Jean, who is also 68 years old, has had type 2 diabetes for 6 years. She weighs 117 kg and has been unable to lose weight on diet or metformin treatment. Gliclazide was introduced about 1 year ago. This improved metabolic control initially but resulted in weight gain of nearly 6.5 kg over a 6-month period. The dose of gliclazide has been increased to maximum without further benefit and Jean’s blood glucose levels at the clinic are usually greater than 17 mmol/L. Jean is troubled by recurrent carbuncles and recurrent vaginal thrush.
Jean is markedly obese and likely to be insulin resistant. Attempts to achieve control of blood glucose can result in massive doses of insulin being prescribed. This in turn can result in further weight gain. However, the UKPDS has demonstrated the benefit of insulin therapy in preventing long-term complications, despite weight gain. Every effort should be made to encourage weight loss by dieting and exercise, and the use of an anti-obesity drug may be justified. Improved metabolic control in Jean’s situation will reduce the incidence of repeated skin and vaginal infections.
INSULIN PROTOCOLS
Until recently, most general practitioners in the UK referred individuals requiring insulin therapy to the local hospital diabetic clinic. Increasingly, however, insulin therapy is being instigated in the community. The principles of insulin therapy in type 2 diabetes will be briefly described here and the reader is referred to Chapter 5, where the subject is dealt with in greater depth.
The UKPDS used once-daily ultralente insulin or isophane insulin, which reflected common practice during the 1970s and 1980s. During that era, oral hypoglycaemic agents were withdrawn and replaced by insulin treatment. Once-daily insulin injections would be particularly suitable for elderly people who might require community nursing assistance with injections. However, for the majority of individuals the aim is to achieve optimum metabolic control, and such regimens are rarely adequate. An early study suggested that if once-daily isophane insulin was used, there was some evidence that better overall control of the diabetes could be achieved if the insulin was given at bedtime rather than before breakfast (Seigler et al 1992). However, as bedtime insulin can be associated with nocturnal hypoglycaemia, this form of therapy has been discouraged. When once-daily insulin injections failed to adequately control hyperglycaemia, the person was normally switched to twice-daily or multiple injection regimens. New insulin analogues available nowadays mean that night-time injections are again feasible (see Chapter 5).
INSULIN AND ORAL HYPOGLYCAEMIC AGENT COMBINATIONS
Sulphonylurea plus insulin
Increasingly, the trend in recent years has been to continue sulphonylurea and/or metformin treatment while introducing insulin therapy. The launch of insulin glargine has encouraged this trend and studies have shown that bedtime insulin glargine in combination with oral therapy can achieve tight diabetic control while causing significantly less nocturnal hypoglycaemia than isophane insulins (Riddle et al 2003).
Combination sulphonylurea and insulin therapy can be effective in people with a partial beta-cell response to sulphonylureas. As the sulphonylureas stimulate endogenous insulin secretion, lower insulin doses might be expected to be effective. The combination of an oral agent with a single daily insulin injection can make the introduction of insulin more acceptable to the individual person.
This combination has been the subject of several studies and a meta-analysis of 16 studies has shown that the combination of sulphonylurea plus insulin improves glycaemic control with reduced insulin requirements and with no adverse effect on weight (Johnson et al 1996). Combination therapy was associated with a 1.1% reduction in HbA1c as compared to 0.25% reduction with insulin monotherapy.
Metformin plus insulin
For the obese person with insulin resistance, a combination of metformin and insulin seems logical. Metformin improves the action of insulin on peripheral tissues and one would expect it to reduce the requirement for high doses of insulin in this type of individual. The addition of metformin to insulin therapy might also be expected to reduce or prevent the inevitable weight gain which occurs in obese people with type 2 diabetes following the introduction of insulin therapy.
Metformin plus insulin therapy has been associated with an insulin sparing effect of between 15–32% in people with type 2 diabetes (Buse 2000). This combination has been shown to reduce HbA1c to a greater extent than insulin alone, while using a lower dose of insulin.
If combination treatment with oral agents and insulin fails to control blood glucose levels, people can be changed onto twice-daily insulin regimens. Fixed mixtures of short-acting and isophane insulins are probably the simplest insulins to use in this group of people.
Thiazolidinedione therapy is contraindicated for people on insulin treatment. Thiazolidinediones should therefore be withdrawn before the introduction of insulin treatment.
Beatrice is a 67-year-old woman who was admitted to hospital 7 months ago having sustained a dense right hemiplegia and aphasia. On admission to hospital a random blood glucose was measured at 17 mmol/L and, in accordance with the protocol for acute treatment of stroke, she was started on an insulin infusion to control her hyperglycaemia. Initially, Beatrice required nasogastric feeding and intravenous insulin was continued. When she was again able to swallow and eat, the insulin was changed to twice-daily injections of a fixed insulin mixture. She had a prolonged period of rehabilitation but remained chair-bound and profoundly dysphasic.
On discharge from hospital, Beatrice’s insulin requirements were 28 units per day. However, over the next few weeks, she had several hypoglycaemic episodes and the insulin was gradually reduced to 12 units per day. It was therefore decided to stop insulin treatment and she was converted to gliclazide 80 mg twice daily. The dose of gliclazide was, however, reduced first to 80 mg once daily and then 40 mg daily. Diabetic control remained tight and the oral agent was also stopped. Months later, Beatrice’s blood glucose remains in the range 4.0–8.0 mmol/L on diet alone.
Similarly, the introduction of medications such as steroids can result in deterioration in glycaemic control and the need to increase glucose lowering therapy. On cessation of steroid treatment, the insulin or oral agent might need to be reduced in dosage or withdrawn.
DRUGS OF THE FUTURE
DUAL PPARα AND PPARγ RECEPTOR AGONISTS
Current PPARγ receptor agonists exhibit only mild lipid-lowering effects in addition to their insulin-sensitising action. Fibrates are PPARα receptor agonists and have been used for many years as lipid-lowering agents. They reduce plasma triglycerides and raise HDL cholesterol while reducing LDL cholesterol. By combining the therapeutic effects of PPARα and γ receptor agonists, the major metabolic disorders of type 2 diabetes, hyperglycaemia, insulin resistance and dyslipidaemia can be addressed simultaneously.
Aside from improving dyslipidaemia, cardiovascular risks can be further modified by dual activation of PPARα and γ receptors, as this has been shown to exert direct antiatherogenic effects (Jackson et al 1999, Marx et al 1999). In addition, this dual activation has been shown in animal models to reduce the undesirable weight gain associated with TZD therapy (Chaput et al 2000, Guerre-Millo et al 2000). By simultaneously stimulating both PPARα and γ, the propensity for adipogenesis resulting from PPARγ activation might be offset by the propensity of PPARα activation to stimulate lipid catabolism.
Muraglitazar
Muraglitazar is a novel non-TZD dual PPARα and γ agonist. This drug, along with other dual PPARα and γ agonists is currently under development.
The amylin story
Amylin is a pancreatic hormone that is co-localised with insulin in the beta cells and co-secreted with insulin in response to meals. Postprandial insulin and amylin responses become markedly reduced as beta-cell function deteriorates with advancing type 2 diabetes.
Modes of action
Following its release from the pancreas, amylin acts on the brain. It binds to specific sites, including the area postrema. Signals sent via the vagus nerve then result in the slowing of gastric emptying. Amylin also acts centrally as an appetite suppressant (Young et al 2000). In addition, amylin suppresses nutrient-stimulated secretion of glucagon (Gedulin et al 1997). This hormone is responsible for stimulating postprandial release of glucose from the liver.
Thus amylin contributes to normal glucose homeostasis through actions that limit nutrient influx during the postprandial period.
Pramlintide
Pramlintide is a synthetic analogue of human amylin and has similar biological actions. Studies with pramlintide are now well advanced. Current regimens of insulin therapy in type 2 diabetes are associated with excessive weight gain, failure to adequately control postprandial glycaemic excursions and an increased risk of hypoglycaemia. Studies of pramlintide in both type 1 and type 2 diabetes have shown beneficial effects when it is co-injected with insulin (Thomson et al., 1997 and Thomson et al., 1998). These studies have demonstrated that the addition of pramlintide to insulin can result in improved glycaemic control without the need to increase insulin doses and in association with significant weight loss. The improvement in glycaemic control with pramlintide was not associated with an increased incidence of severe hypoglycaemia. Pramlintide therefore appears to go some way to counter the detrimental effects of insulin treatment in type 2 diabetes. It is likely that this compound will come to the market in the near future.
The incretin story
It has long been recognised that orally administered glucose provokes greater stimulation of insulin release than similar amounts infused intravenously. Hence, it has been postulated that oral nutrient ingestion must stimulate gut-derived signals that are potent stimulators of insulin release (incretins). The neurotransmitter substances glucagon-like peptide-1 (GLP-1) and glucose-dependent insulinotropic peptide (GIP) have been identified as the most important peptides for the majority of nutrient-stimulated insulin secretion.
Unlike the potent glucose-lowering actions of GIP in normal rodents, exogenous administration of GIP is less effective in diabetic rodents. It is, therefore, unlikely to be of clinical benefit for people with type 2 diabetes. However, GLP-1 appears to be equipotent in diabetic and non-diabetic animals. GLP-1 has been shown to have additional glucose-lowering properties. These include inhibition of glucagon secretion, inhibition of gastric emptying and reduction of food intake.
GLP-1 is metabolised very rapidly by the enzyme dipeptidyl peptidase IV (DPP-IV). Because of this, the effects of a single injection of GLP-1 are short-lasting and continuous intravenous infusions are required for sustained effects. In order to overcome this problem, degradation-resistant GLP-1 analogues with longer duration of action have been developed.
Exendin-4 (exenatide)
Exendin-4 is a naturally occurring GLP-1 receptor agonist isolated from the salivary gland venom of the lizard Heloderma suspectum. Exendin-4 is highly resistant to the proteolytic activity of DPP IV and exhibits a longer duration of action. Exendin-4, now renamed exenatide, must be given by twice-daily subcutaneous injections. It is currently being evaluated for treatment of type 2 diabetes in combination with metformin, sulphonylureas or both (Fineman et al 2003).
Liraglutide is a fatty-acid-linked DPP-IV-resistant GLP-1 analogue that is given once daily and is also undergoing clinical trials for treatment of type 2 diabetes. A further GLP-1 analogue currently named CJC-1131 and with a half-life of 10 days is undergoing preliminary studies in humans (Baggio & Drucker 2004).
DPP IV inhibitors
An alternative therapeutic approach to prolong the action of GLP-1 is to inhibit the enzyme DDP IV. Several DDP IV inhibitors (LAF-237, MK-0431 and P93/01) are currently undergoing clinical trials. These drugs have the advantage over GLP-1 analogues that they can be administered orally.
MEDICATIONS ALTERING GLUCOSE TOLERANCE AND DRUG INTERACTIONS
Individuals with type 2 diabetes are likely to be middle aged or elderly and might have other medical conditions that need to be treated simultaneously. As stated elsewhere, type 2 diabetes is associated with hypertension, hyperlipidaemia and vascular disease. Polypharmacy is the norm for these people, who may often be taking medications that interfere with their diabetes (Table 4.2).
| Hypoglycaemic effects | hyperglycaemic effects |
|---|---|
| alcohol | corticosteroids |
| monoamine oxidase inhibitors | thiazide and loop diuretics |
| fibrates | chlorpromazine |
| miconazole | chronic alcohol |
| salicylates | oral contraceptives |
| cimetidine, ranitidine | anabolic steroids |
HYPERGLYCAEMIC EFFECTS
Diuretics
Thiazide diuretics such as bendroflumethiazide are known to increase blood glucose levels by causing increased resistance to the action of insulin on peripheral tissues. Thiazides are often included in ‘combination pills’ such as Tenoretic and Capozide. The loop diuretics, furosemide and bumetanide, also have mild effects on glucose tolerance.
The beta-blockers are now less commonly used as first-line therapy for hypertension. They remain useful drugs, however, in people who also have angina. These drugs also impair glucose tolerance and might worsen diabetic control.
Oestrogen
Oestrogen-containing preparations or drugs with oestrogen-like actions can increase blood glucose levels. Although oral contraceptive agents are not often used in this age group, hormone replacement therapy is used and must be introduced with care in the older female with type 2 diabetes lest diabetic control deteriorates. The anti-oestrogen, tamoxifen, has oestrogenic effects and can worsen glucose tolerance. This medication is commonly used in older persons with breast malignancy.
Steroids
Corticosteroids antagonise the action of insulin and therefore medications, such as prednisolone, used for the treatment of asthma or for immunosuppression will result in raising blood glucose concentrations. Anabolic steroids are used in some people with malignancy and are also used illegally for body building. They will also cause blood glucose levels to rise.
Adrenaline
Adrenaline is another hormone that can counter the action of insulin and it is important to remember that adrenaline or adrenaline-like compounds (phenylpropanolamine and ephedrine) are frequently found in decongestants and cold remedies.
Atypical antipsychotics
Over the past 10 years, the atypical (also known as novel or second-generation) antipsychotic drugs have increasingly been used to treat schizophrenia and related disorders in which psychosis is a prominent feature. The British National Formulary currently lists amisulpride, clozapine, olanzapine, quetiapine, risperidone, aripiprazole, sertindole and zotepine as atypical antipsychotics.
Recently, evidence has been mounting to suggest that atypical antipsychotic drugs are associated with adverse metabolic effects, including weight gain, new-onset diabetes (both type 2 and diabetic ketoacidosis) and hypertriglyceridaemia. (Koller et al 2001, Newcomer et al 2002). These drugs have also been noted to exacerbate pre-existing diabetes.
The mechanism by which atypical antipsychotic drugs affect glucose metabolism remains unclear but it is likely that multiple factors are involved. These drugs can cause weight gain, with an associated increase in insulin resistance. However, it is likely that these drugs have an adverse effect on insulin sensitivity independent of their tendency to cause weight gain. It is therefore recommended that fasting glucose, HbA1c and lipids are monitored at least 6-monthly in people taking atypical antipsychotics, and more often in those at greater risk of diabetes.
A variety of drugs can have hypoglycaemic effects (Table 4.3). Aspirin and other non-steroidal anti-inflammatory agents have a mild blood-glucose-lowering effect. Similarly, alcohol can cause hypoglycaemia, particularly if a person is taking insulin or on sulphonylurea treatment. Alcohol acts on the liver and reduces the ability of the liver to produce glucose. Hence alcohol will enhance the hypoglycaemic effects of insulin or oral hypoglycaemic agents.
| *Enhance action of drug. |
|||
| **Antagonise action of drug. |
|||
| Sulphonylureas | meglitinides | metformin | glitizones |
|---|---|---|---|
| sulphonamides* | gemfibrozil* | cimetidine* | unusual |
| trimethoprim* | clarithromycin* | ||
| chloramphenicol* | |||
| ciprofloxacin* | |||
| itraconazole, fluconazole* | |||
| rifampicin** | |||
Drug interactions with sulphonylureas
Drugs that bind to proteins in the blood can displace the sulphonylureas from their binding sites and release the more active drug into the circulation, thus causing hypoglycaemia. The sulphonamide antibiotics and trimethoprim are examples of drugs that compete with the sulphonylureas for their protein binding sites. Other antibiotics, such as chloramphenicol and the 4-quinolones, can also enhance the hypoglycaemic action of the sulphonylureas. Rifampicin, however, is an antibiotic that accelerates the metabolism of the sulphonylureas and therefore reduces their therapeutic effect.
Drug interactions with meglitinides
A potentially dangerous interaction between repaglinide and gemfibrozil has been identified. Gemfibrozil markedly increases the systemic exposure to repaglinide and this combination of drugs should be avoided. A similar interaction occurs between repaglinide and clarithromycin and this may require a reduction in the dose of repaglinide.
Table 4.3 also lists medications that alter the hypoglycaemic effects of the above agents. The reader is also referred to the British National Formulary for a more extensive list of interactions.
Cimetidine increases the serum levels of metformin by competing with metformin for transport across the renal tubules.
Dietary management is fundamental to the care of all people with type 2 diabetes. However, a substantial number of people will fail to control their diabetes with diet alone and will require oral hypoglycaemic agents. Exercise and other lifestyle changes are also required to improve metabolic status and reduce long-term cardiovascular disease. Type 2 diabetes is a progressive disease requiring increasing doses of hypoglycaemic agents and additional therapies to maintain glycaemic control.
Tight metabolic control is associated with significant reductions in the incidence of microvascular complications. There is also a reduction in macrovascular disease with reducing HbA1c results. Metformin treatment in obese people with diabetes has been shown to significantly reduce these macrovascular events.
Metformin is the drug of first choice for the obese person with diabetes, and indeed metformin should probably also be used first in non-obese people. Thiazolidinediones are currently not recommended as first-line treatment in the UK unless other medications are contraindicated or not tolerated. This situation might change if these drugs are shown to have beneficial effects on cardiovascular outcomes.
As metabolic control deteriorates, combination therapy using different classes of oral hypoglycaemics will be required. Increasingly, insulin therapy is used to prolong glycaemic control. Insulin is often introduced as a single injection while people are maintained on an oral agent, and only when this combination regimen fails are multiple insulin injections introduced.
REFERENCES
C Aguilar, A Reza, JE Garcia, JA Rull, Biguanide related lactic acidosis: incidence and risk factors, Archives of Medical Research 23 (1992) 19–24.
M Apfelbaum, P Vague, O Ziegler, et al., Long-term maintenance of weight loss after a very-low-calorie diet: a randomised blinded trial of the efficacy and tolerability of sibutramine, American Journal of Medicine 106 (1999) 179–184.
LL Baggio, DJ Drucker, Incretin hormones and the treatment of type 2 diabetes Online, Available: www.medscape.com/viewarticle/482591 (2004).
CJ Bailey, Biguanides and NIDDM, Diabetes Care 15 (1992) 755–772.
MC Blonk, MAJM Jacobs, EHE Biesheuvel, et al., Influences on Weight Loss in Type 2 Diabetic Patients: Little Long-term Benefit from Group Behaviour and Exercise Training, Diabetic Medicine 11 (1994) 449–457.
J Buse, Combining insulin and oral agents, American Journal of Medicine 108 (6 suppl 1) (2000) 23–32 .
JCN Chan, K-WA Chan, LLT Ho, et al., An Asian multicenter clinical trial to assess the efficacy and tolerability of acarbose compared with placebo in Type 2 diabetic patients previously treated with diet, Diabetes Care 21 (1998) 1058–1061.
E Chaput, R Saladin, M Silvestre, AD Edgar, Fenofibrate and rosiglitazone lower serum triglycerides with opposing effects on body weight, Biochemistry and Biophysics Research Communications 271 (2000) 445–450.
DG Dills, J Schneider, Clinical evaluation of glimepiride versus glyburide in NIDDM in a double-blind comparative study. Glimepiride/Glyburide Research Group, Hormones and Metabolic Research 28 (9) (1996) 426–429.
PJ Donnan, TM MacDonald, AD Morris, Adherence to prescribed oral hypoglycaemic medication in a population of patients with type 2 diabetes: a retrospective cohort study, Diabetic Medicine 19 (2002) 279–284.
CA Dujovne, JH Zavirak, E Rowe, et al., Effects of sibutramine on both body weight and serum lipids; a double blind, randomised, placebo-controlled study in 322 overweight and obese patients with dyslipidaemia, American Heart Journal 142 (2001) 489–497.
AN Faria, FF Ribeiro Filho, DD Lerarlo, et al., Effects of sibutramine on the treatment of obesity in patients with arterial hypertension, Arquivos Brasileiros de Cardiologia 78 (2002) 172–180.
RE Ferner, HAW Neil, Sulphonylurea and hypoglycaemia [editorial], British Medical Journal 296 (1988) 949–950.
MS Fineman, TA Bicsak, LZ Shen, et al., Effect on glycaemic control of synthetic exendin-4 (AC2993) additive to existing metformin and/or sulfonylurea treatment in patients with type 2 diabetes, Diabetes Care 26 (2003) 2370–2377.
N Finer, SR Bloom, GS Frost, et al., Sibutramine is effective for weight loss and diabetic control in obesity with type 2 diabetes: a randomised double-blinded, placebo-controlled study, Diabetes Obesity and Metabolism 2 (2000) 105–112.
K Fujioka, TB Seaton, E Rowe, et al., Weight loss with sibutramine improves glycaemic control and other metabolic parameters in obese patients with type 2 diabetes mellitus, Diabetes Obesity & Metabolism 2 (2000) 175–187.
AJ Garber, D Theodore, A Goodman, et al., Efficacy of metformin in type II diabetes: results of a double-blind, placebo-controlled, dose response trial, American Journal of Medicine 103 (1997) 491–497.
BR Gedulin, TJ Rink, AA Young, Dose-response for glucagonostatic effect of amylin in rats, Metabolism 46 (1997) 67–70.
D Gordon, Diabetes. The patient with non-insulin-dependent-diabetes mellitus, In: (Editors: J McDowell, D Gordon) Caring for patients in the community (1996) Churchill Livingstone, London.
F Greenway, Obesity medications and the treatment of type 2 diabetes, Diabetes Technology and Therapeutics 1 (1999) 277–287.
M Guerre-Millo, P Gervois, E Raspe, et al., Peroxisome proliferator-activated receptor a activators improve insulin sensitivity and reduce adiposity, Journal of Biological Chemistry 275 (2000) 16638–16642.
A Halpern, MC Mancini, H Suplicy, et al., Latin-American trial of orlistat for weight loss and improvement in glycaemic profile in obese diabetic patients, Diabetes Obesity and Metabolism 5 (2003) 180–188.
M Hanefeld, G Sachse, The effects of orlistat on body weight and glycaemic control in overweight patients with type 2 diabetes: a randomized, placebo-controlled trial, Diabetes Obesity and Metabolism 4 (2002) 415–423.
A Harrower, C Wong, Comparison of secondary failure rate between three second generation sulphonylureas, Diabetes Research 13 (1990) 19–21 .
BP Hazenburg, Randomised, double-blind, placebo-controlled, multicenter study of sibutramine in obese hypertensive patients, Cardiology 94 (2000) 152–158.
JE Helmrich, DR Ragland, RW Leung, et al., Physical activity and reduced occurrence of non-insulin-dependent diabetes mellitus, New England Journal of Medicine 325 (1991) 147–152.
RR Holman, C Cull, R Turner, et al., (UKPDS 44) A randomized double-blind trial of acerbose in Type 2 diabetes shows improved glycaemic control over 3 years, Diabetes Care 22 (1999) 960–964.
FB Hu, JE Manson, MJ Stampfer, et al., Diet, lifestyle, and the risk of type 2 diabetes mellitus in women, New England Journal of Medicine 345 (2001) 790–797.
SM Jackson, F Parhami, XP Xi, et al., Peroxisome proliferator-activated receptor activators target human endothelial cells to inhibit leukocyte—endothelial cell interaction, Arteriosclerosis Thrombosis and Vascular Biology 19 (1999) 2094–2104.
S Jariwala, R Mather, L Walker, et al., Long-term glycaemic control with rosiglitazone in combination with metformin, Diabetic Medicine 20 (suppl 2) (2003); poster 277.
JL Johnson, SL Wolf, M Kabali, Efficacy of insulin and sulphonylurea combination therapy in type II diabetes. A meta-analysis of the randomized placebo-controlled trials, Archives of Internal Medicine 156 (3) (1996) 259–264.
DE Kelley, GA Bray, FX Pi-Sunyer, et al., Clinical efficacy of orlistat therapy in overweight and obese patients with insulin-treated type 2 diabetes: a 1-year randomized controlled trial, Diabetes Care 25 (2002) 1033–1041.
DE Kelley, LH Kuller, TM McKolanis, et al., Effects of moderate weight loss and orlistat on insulin resistance, regional adiposity and fatty acids in type 2 diabetes, Diabetes Care 27 (2004) 33–40.
E Koller, B Schneider, K Bennett, et al., Clozapine-associated diabetes, American Journal of Medicine 111 (2001) 716–723.
J Lindstrom, J Tuomilehto, M Spenglert, for the Finnish Acarbose Study Group, Acarbose treatment does not change the habitual diet of patients with type 2 diabetes mellitus, Diabetic Medicine 17 (2000) 20–25.
JE Manson, EB Rimm, MJ Stampfer, et al., Physical activity and incidence of non-insulin-dependent diabetes mellitus in women, Lancet 338 (1991) 774–778.
N Marx, GK Sukhova, T Collins, et al., PPAR alpha activators inhibit cytokine-induced vascular cell adhesion molecule-1 expression in human endothelial cells, Circulation 99 (1999) 3125–3131.
DR Mathews, A Bakst, WM Weston, et al., Rosiglitazone decreases insulin resistance and improves beta cell function in patients with type 2 diabetes, Diabetologia 42 (suppl 1) (1999) A228; abstract 858.
A Melander, P-O Bitzen, O Faber, L Groop, Sulphonylurea antidiabetic drugs: an update of their clinical pharmacology and rational therapeutic use, Drugs 37 (1989) 58–72.
FG McMahon, K Fujioka, BN Singh, et al., Efficacy and safety of sibutramine in obese white and African American patients with hypertension:a 1-year, double-blind, placebo-controlled, multicenter trial, Archives of Internal Medicine 160 (2000) 2185–2191.
JM Miles, L Leiter, P Hollander, et al., Effects of orlistat in overweight and obese patients with type 2 diabetes treated with metformin, Diabetes Care 25 (2002) 1123–1128.
National Institute for Health and Clinical Excellence (NICE), National clinical guidelines for type 2 diabetes. Online, Available: www.nice.org.uk/pdf/NICE_full_blood_glucose (2004); [accessed 18 September 2004].
JW Newcomer, DW Haupt, R Fucetola, et al., Abnormalities in glucose regulation during antipsychotic treatment of schizophrenia, Archives of General Psychiatry 59 (2002) 337–345.
MC Riddle, J Rosenstock, J Gerlich, The treat-to-target trial: randomized addition of glargine or human nph insulin to oral therapy of type 2 diabetes patients, Diabetes Care 26 (11) (2003) 3080–3086 .
J Rosenstock, Improved insulin sensitivity and beta cell responsivity suggested by HOMA analysis of pioglitazone therapy, Diabetologia 443 (suppl 1) (2000) A192.
AJ Scheen, N Finer, P Hollander, et al., for RIO-Diabetes Study Group. Efficacy and tolerability of rimonabant in overweight or obese patients with type 2 diabetes: a randomised controlled study, Lancet 368 (2006) 1660–1672.
N Scorpiglione, M Belfiglio, F Carinci, et al., The effectiveness, safety and epidemiology of the use of acarbose in the treatment of patients with type II diabetes mellitus. A model of medicine-based evidence, European Journal of Clinical Pharmacology 55 (1999) 239–249.
R Scott, CJ Lintott, P Zimmet, et al., Will acerbose improve the metabolic abnormalities of insulin-resistant type 2 diabetes mellitus, Diabetes Research and Clinical Practice 43 (1999) 179–185.
DE Seigler, GM Olsson, JS Skyler, Morning versus bedtime isophane insulin in type 2 (non-insulin dependent) diabetes mellitus, Diabetic Medicine 9 (1992) 826–833.
M Serrano-Rios, N Melchionda, E Moreno-Carretero, Role of sibutramine in the treatment of obese type 2 diabetic patients receiving sulphonylurea therapy, Diabetic Medicine 19 (2002) 119–124.
AM Sharma, Sibutramine in overweight/obese hypertensive patients, International Journal of Obesity 25 (suppl 4) (2001) S20–S23.
GE Sonnenberg, DC Carg, DJ Weilder, et al., Short term comparison of once-versus twice-daily administration of glimepiride in patients with non-insulin-dependent diabetes mellitus, The Annals of Pharmacotherapy 31 (1997) 671–676.
V Stevens, E Obarzanek, N Cook, et al., Long-term weight loss and changes in blood pressure: Results of the trial of hypertension prevention, phase II, Annals of Internal Medicine 134 (2001) 1–11.
RG Thomson, J Peterson, A Gottlieb, J Mullane, Effects of pramlintide, an analog of human amylin, on plasma glucose profiles in patients with insulin-dependent diabetes mellitus: results of a multicenter trial, Diabetes 46 (1997) 632–636.
RG Thomson, LRN Pearson, SL Schoenfeld, et al., Pramlintide, a synthetic analog of human amylin, improves the metabolic profile of patients with type 2 diabetes using insulin, Diabetes Care 21 (1998) 987–993.
PC Tong, ZS Lee, MM Sea, et al., The effect of orlistat-induced weight loss, without concomitant hypocaloric diet, on cardiovascular risk factors and insulin sensitivity in young obese Chinese subjects with or without type 2 diabetes, Archives of Internal Medicine 162 (2002) 2428–2435.
P Tontonoz, E Hu, RA Graves, et al., mPPARγ2: tissue-specific regulator of an adipocyte enhancer, Genes and Development 8 (1994) 1224–1234.
JS Torgeson, J Hauptman, MN Boldrin, et al., Xenical in the prevention of diabetes in obese subjects (XENDOS Study). A randomized study of orlistat as an adjunct to lifestyle changes for the prevention of type 2 diabetes in obese patients, Diabetes Care 27 (2004) 155–161.
UK Prospective Diabetes Study (UKPDS) Group, Response of fasting plasma glucose to diet therapy in newly presenting type II diabetic patients (UKPDS 7), Metabolism 39 (1990) 905–912.
UK Prospective Diabetes Study (UKPDS) Group, Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33), Lancet 352 (1998) 837–853.
UK Prospective Diabetes Study (UKPDS) Group, Effect of intensive blood-glucose control with metformin on complications in overweight patients with type 2 diabetes (UKPDS 34), Lancet 352 (1998) 854–865 .
AJ Vidal-Puig, PV Considine, M Jimenez-Linan, et al., Peroxisome proliferator-activated receptor gene expression in human tissues. Effects of obesity, weight loss, and regulation by insulin and glucocorticoids, Journal of Clinical Investigation 99 (1997) 2416–2422.
A Young, C Moore, J Herich, K Beaumont, In: (Editors: D Poyner, I Marshall, SD Brain) CGRP family: calcitonin gene-related peptide (CGRP), amylin, and adrenomedullin (2000) Landes Bioscience, Georgetown, TX, pp. 91–102.