Section 4 Orthopaedic Emergencies
4.1 Injuries of the shoulder
Fractures of the clavicle
Fractures of the clavicle account for 2.6–5% of all fractures and usually result from a direct blow on the point of the shoulder, but may also be due to a fall on the outstretched hand. The most common site of fracture is the middle third of the clavicle, which accounts for 69–82% of clavicular fractures. There are varying degrees of displacement of the fracture ends, with overlapping fragments and shortening being common. Owing to the strategic location of the clavicle, injury to the pleura, axillary vessels and/or brachial plexus is possible, but fortunately these complications are rare.
Midshaft fractures with complete displacement, comminution or fractures in the elderly or women with osteoporosis, have a higher rate of non-union and poorer functional outcome. Recent evidence suggests that this group may benefit from surgical stabilization with either plate-and-screw fixation or intramedullary devices. Fractures of the outer third of the clavicle may involve the coracoclavicular ligaments. If so, surgical management should be considered. This may be performed by open or arthroscopic techniques.
Rotator cuff injuries
Treatment of rotator cuff strains is conservative, usually including analgesia and physiotherapy. Local injection of hydrocortisone may be useful if symptoms persist. Treatment of rotator cuff tears is controversial, with no clear evidence guiding the choice of operative versus non-operative therapy or the components or duration of non-operative treatments. Most experts would still recommend a trial of non-operative therapy before considering surgery. An exception to this may be the patient with a previously asymptomatic shoulder who sustains trauma with resultant weakness (after the pain from the injury subsides) in whom imaging studies indicate an acute full-thickness tear.
Dislocation of the shoulder
Anterior dislocation
Bicos J, Nicholson GP. Treatment and results of sternoclavicular injuries. Clinical Journal of Sport Medicine. 2003;22:359-370.
Canadian Orthopaedic Trauma Society. Non-operative treatment compared with plate fixation of displaced midshaft clavicular fractures. A multi-center randomized clinical trail. Journal of Bone and Joint Surgery. 2007;89A:1-10.
Kuhn JE. Treating the initial anterior shoulder dislocation – an evidence-based medicine approach. Sports Medicine and Arthroscopy Review. 2006;14:192-198.
Miljesic S, Kelly AM. Reduction of anterior dislocation of the shoulder: the Spaso technique. Emergency Medicine. 1998;10:173-175.
Oh LS, Wolf BR, Hall MP, et al. Indications for rotator cuff repair: a systematic review. Clinical Orthopaedics and Related Research. 2007;455:52-63.
Zlowodzki M, Bhandari M, Zelle BA, et al. Treatment of scapula fractures: systematic review of 520 fractures in 22 case series. Journal of Orthopaedic Trauma. 2006;20:230-233.
4.2 Fractures of the humerus
Fractures of the proximal humerus
Patterns of injury
Fractures of the proximal humerus represent 5% of all fractures presenting to emergency departments (ED) and 25% of all humeral fractures. The fracture typically occurs as a result of an indirect mechanism in elderly, osteoporotic patients who fall on their outstretched hand with an extended elbow. These injuries are important to understand, as the majority do not require surgical intervention and may initially be treated in the ED. A subset with non-viable humeral head requires early surgical intervention, and it is therefore important to identify this group. Fractures of the humerus may also occur in patients with multiple injuries or in the elderly with associated fractures of the neck of femur.1
Clinical assessment
History and examination
A neurovascular examination is essential as the axillary nerve, brachial plexus and/or axillary artery may be damaged. The axillary nerve is the most commonly injured, and presents with altered sensation over the badge area (insertion of the deltoid) and reduced deltoid muscle contraction (which may be hard to assess because of pain). The axillary artery is the commonest vessel to be injured and may present with any combination of limb pain, pallor, paraesthesia, pulselessness, poor limb perfusion and paralysis.
Fracture classification
Neer classification system
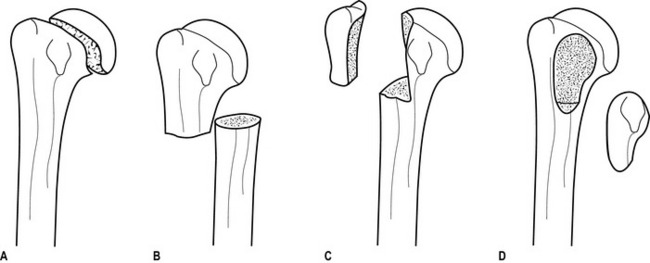
In this system, fractures are classified first according to four anatomical sites (anatomical and surgical necks, greater and lesser tuberosities); second, according to the number of fragments (one to four parts); and third, according to the degree of fracture displacement, defined as 1 cm separation or >45° angulation (Figs 4.2.1 and 4.2.2).
Two-part fracture
Two-part fractures account for 10% of proximal humeral fractures, and usually one fragment is significantly displaced. Two-part fractures of the humerus may involve the anatomical neck (Fig. 4.2.1a), the surgical neck (Fig. 4.2.1b), the greater tuberosity (Fig. 4.2.1c) or the lesser tuberosity (Fig. 4.2.1d).
Management
For undisplaced three- and four-part fractures, the consensus is for open reduction and internal fixation. However, recent reviews suggest that there is little evidence that surgery is superior to the non-operative approach.2
For displaced proximal humeral fractures, surgical management remains varied and controversial.3 Small randomized controlled trials suggest that external fixation may confer some benefit over closed manipulation,4 and that conservative treatment is better than tension band osteosynthesis.5 A recent study shows that the decision should be made according to the viability of the humeral head. Locking plate technology may also provide better outcomes in patients with unstable displaced humeral fractures having a viable humeral head.6 Other small-scale studies suggest that some bandaging styles may be better than others,7 that early physiotherapy may improve functional outcome, but that pulsed high-frequency electromagnetic energy gives no additional benefit.8
Special cases
Fracture dislocations
Fractures of the greater tuberosity accompany 15% anterior glenohumeral dislocations and may be associated with rotator cuff tears. Although the fracture may be grossly displaced, reduction of the dislocated shoulder usually also reduces the fracture. In patients who require the full range of movement of their shoulders, surgical repair of the cuff may be required.
Fractures of the lesser tuberosity are associated with posterior glenohumeral dislocations.
Fractures of the shaft of humerus
Patterns of injury
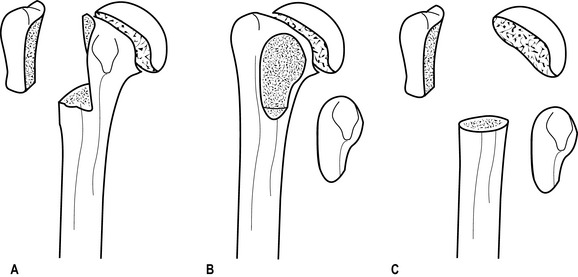
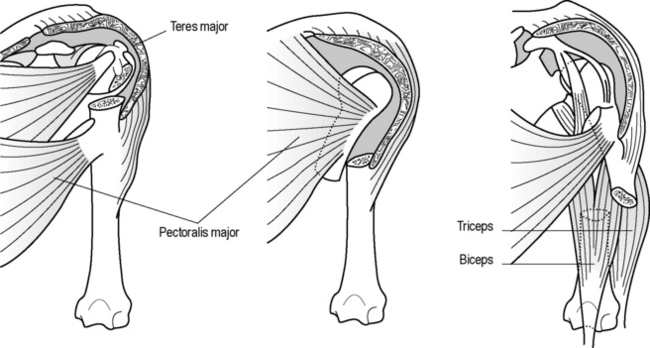
The angle and degree of displacement of the fracture depends on the site of injury and its relationship to the action and attachment of muscles on either side of the injury (Fig. 4.2.3).
Clinical assessment
History and examination
The commonest complication is radial nerve injury resulting either from injury or reduction of the fracture, and evidenced by wrist drop and altered sensation in the first dorsal web space. A recent systemic review reported that radial nerve injury occurs in 11% of mid-shaft humerus fractures.9
Fracture management and disposition
Uncomplicated, closed fractures account for the majority of injuries and may be treated by immobilization, analgesia, a functional brace such as a hanging or U-shaped cast (Fig. 4.2.3), and a broad arm or collar and cuff sling. The acceptable deformity is 20° anterior/posterior angulation, and 30° valus/valgus deformity.10 The union rate is usually higher than 90%. Early specialist follow-up is recommended.
Some departments may prefer a humeral brace rather than U-shaped plaster for immobilization, as the former may permit greater functional use without affecting healing or fracture alignment.11 For oblique/spiral fractures some orthopaedic surgeons prefer an operative approach for a better functional outcome.12
Open fractures and complications affecting the vessels require surgical repair. Although the majority of radial nerve injuries are neuropraxia and recover without surgical intervention, each case should be considered individually by an orthopaedic surgeon with a view to possible operative exploration.
Fractures of the distal humerus
Classification and patterns of injury
Unlike in children, fractures of the distal humerus in adults are very uncommon and patterns of injury tend to reflect the anatomical two-column construction (condyles) of the humerus. Several classification methods have been used, such as the Riseborough and Radin, Mehne and Matta classifications, but the simplest and most commonly used are the AO/ASIF classifications.13 These classify injuries into three categories: type A are extra-articular fractures, type B are partial articular, and type C are complete articular fractures. Practically, distal humeral fractures may be classified into supracondylar, intercondylar and other types. Supracondylar fractures lie transversely, whereas intercondylar T or Y fractures include an additional vertical extension between the condyles.
Clinical assessment
History and examination
Patients typically present with a swollen, tender, deformed elbow. As very little subcutaneous or other tissue separates the bone from skin, any disruption of the skin should be carefully examined for the possibility of a compound fracture. Distal neurological and vascular injury must be assessed carefully, as the possibility of nerve injury has been reported to be as high as 12–20%.14
Investigations
Two radiographic views – anteroposterior and lateral – should be obtained. Some authors suggest that an internal oblique view may improve the diagnostic accuracy.15 Pain and inability to extend the elbow often result in poor-quality radiographs. Although high-quality radiographs are essential for operative planning, repeat films should not be attempted in the ED as they rarely provide the desired result. When there is any suspicion of severe injury, either from the history or from gross soft tissue swelling, early CT scanning should be considered to give better detail, especially of intra-articular fractures.
Fracture management and disposition
Guidance for management is based primarily on experience rather than rigorous research evidence.
1 Mulhall KJ, Ahmed A, Khan Y, Masterson E. Simultaneous hip and upper limb fracture in the elderly: incidence, features and management considerations. Injury. 2002;33:29-31.
2 Handol HHG, Madhok R. Interventions for treating proximal humeral fractures in adults. Cochrane Database Systematic Review. (4):2003. CD000434. DOI: 0.1002/14651858.CD000434
3 Weber E, Matter P. Surgical treatment of proximal humerus fractures – an international multicenter study [In German]. Swiss Surgery. 1998;4:95-100.
4 Kristiansen B, Kofoed H. Transcutaneous reduction and external fixation of displaced fractures of the proximal humerus. A controlled clinical trial. Journal of Bone and Joint Surgery. 1988;70:821-824.
5 Zyto K, Ahrengart L, Sperber A, Tornkvist H. Treatment of displaced proximal humeral fractures in elderly patients. Journal of Bone and Joint Surgery. 1999;79:412-417.
6 Vallier HA. Treatment of proximal humerus fractures. Journal of the Orthopaedic Trauma. 2008;21(7):469-476.
7 Rommens PM, Heyvaert G. Conservative treatment of subcapital humerus fractures. comparative study of the classical Desault bandage and the new Gilchrist bandage. Unfallchirurgie. 1993;19:114-118.
8 Livesley PJ, Mugglestone A, Whitton J. Electrotherapy and the management of minimally displaced fracture of the neck of the humerus. Injury. 1992;23:323-327.
9 Shao YC, Harwood P, Grotz MRW, et al. Radial nerve palsy associated with fractures of the shaft of the humerus: A systematic review. Journal of Bone and Joint Surgery. 2005;87-B:1647-1652.
10 Klenerman L. Fractures of the shaft of the humerus. Journal of Bone and Joint Surgery. 1966;48B:105-111.
11 Camden P, Nade S. Fracture bracing the humerus. Injury. 1992;23:245-248.
12 Ring D, Chin K, Taghinia AH, Jupiter JB. Nonunion after functional brace treatment of diaphyseal humerus fractures. Journal of Trauma. 2007;62:1157-1158.
13 Diana JN, Ramsey ML. Decision making in complex fractures of the distal humerus: current concepts and potential pitfalls. Orthopaedic Journal. 1998;11:12-18.
14 Ramachandran M, Birch R, Eastwood DM. Clinical outcome of nerve injuries associated with supracondylar fractures of the humerus in children, the experience of a specialist referral centre. Journal of Bone and Joint Surgery. 2006;88B:90-94.
15 Song KS, Kang CH, Min BW, et al. Internal oblique radiographs for diagnosis of nondisplaced or minimally displaced lateral condylar fractures of the humerus in children. Journal of Bone and Joint Surgery. 2007;89A:58-63.
16 Nolte PA, van der Krans A, Patka P, et al. Low-intensity pulsed ultrasound in the treatment of nonunions. Journal of Trauma. 2001;51:693-702.
McRae R, editor. Practical fracture treatment. Churchill Livingstone, Edinburgh, 1994, 99-127.
Uehara DT, Rudzinski JP. Injuries to the shoulder complex and humerus. In: Tintinalli JE, Kelen GD, Stapczynski JS, editors. Emergency medicine. A comprehensive study guide. New York: McGraw-Hill; 2000:1783-1791.
Willet K. Upper limb injuries. In: Skinner D, Swain A, Peyton R, Robertson C, editors. Cambridge textbook of accident and emergency medicine. Cambridge: Cambridge University Press; 1997:601-617.
4.3 Dislocations of the elbow
Introduction
Elbow dislocation, along with glenohumeral and patellofemoral joint dislocations, is one of the three most common large joint dislocations.1 The elbow joint is a hinge-like articulation involving the distal humerus and proximal radius and ulna. Owing to its strong muscular and ligamentous supports, the joint is normally quite stable and rarely requires operative intervention, even for acute instability after dislocation.
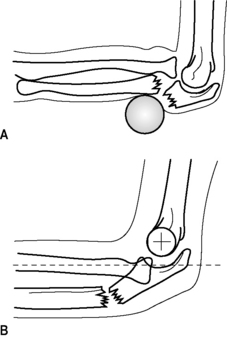
Uncommonly, the radius or ulna alone may dislocate at the elbow. In such cases there is always a fracture of the other bone. One common example is in Monteggia fractures, where anterior or posterior radiohumeral dislocation occurs alongside a fracture of the ulna shaft (Fig. 4.3.1). A rarer example is a posterior ulna–humeral dislocation with fracture of the radial shaft. So, although elbow dislocations may appear to be isolated, it is essential to look for associated intra-articular or shaft fractures.
Clinical assessment
History and examination
Patients typically present holding the lower arm at 45° to the upper arm and with swelling, tenderness and deformity of the elbow joint. The three-point anatomical triangle of olecranon, medial and lateral epicondyles should be assessed for abnormal alignment, as this strongly suggests dislocation.
The commonest neurovascular injury involves the ulnar nerve, reported in 10–15% of elbow dislocations,2 but the median and radial nerves, and the brachial artery may also be affected.
Investigations
Magnetic resonance imaging (MRI) characterizes bony injury more accurately than radiography in children with elbow injuries, but its potential role for diagnosis and guiding management in adults has not been well evaluated.3 Duplex Doppler ultrasound can be use to identify early brachial artery injury.4
Management
There is little evidence that surgical intervention improves outcome in patients with medial or lateral elbow instability after dislocation. One small randomized controlled trial showed no evidence that surgical ligamentous repair produced better results than conservative management.5 Another small study, a case series of patients with humeral medial condyle fracture, suggested good results after surgical management using absorbable implants compared to removal of the bony fragment.6 Current practice is to treat all Monteggia fractures by early reduction and stabilization of the ulnar facture. The majority could be treated very well with close reduction and percutaneous intramedullary K-wire fixation of the ulnar fracture.7 All late cases require open reduction and internal fixation; 45% of these cases are associated with complications and poor long-term functional outcome.8
Compound fracture dislocation should be reduced by the open method.
Disposition
Current practice is that most patients may be discharged from the emergency department (ED) with analgesia, plaster slab support and a broad arm sling with appropriate follow-up. A recent prospective, randomized French study9 suggested that early mobilization is superior to plaster immobilization in terms of functional recovery, without any increased instability or a recurrence of dislocation for patients with uncomplicated posterior dislocations, so the duration of immobilization is controversial. Patients with irreducible dislocations, neurovascular complications, associated fractures or open dislocations require admission.
1 Uehara DT, Chin HW. Injuries to the elbow and forearm. In: Tintinalli JE, Kelen GD, Stapczynski JS, editors. Emergency medicine. A comprehensive study guide. New York: McGraw-Hill; 2000:1763-1772.
2 Robert S, David R. Current concepts review: the ulnar nerve in elbow trauma. Journal of Bone and Joint Surgery. 2007;89A:1108-1116.
3 Griffiths JF, Roebuck DJ, Cheng JCY, et al. Comparison of radiography and magnetic resonance imaging in the detection of injuries after paediatric elbow trauma. American Journal of Roentgenology. 2001;176:53-60.
4 Ergunes K, Yilik L, Ozsoyler I, et al. Traumatic brachial artery injuries. Texas Heart Institute Journal. 2006;33:31-34.
5 Josefsson PO, Gentz CF, Johnell O, Wendeberg B. Surgical versus non-surgical treatment of ligamentous injuries following dislocation of the elbow joint. A prospective randomized study. Journal of Bone and Joint Surgery. 1987;69:605-608.
6 Partio EK, Hirvensalo E, Bostman O, Rokkanen P. A prospective controlled trial of the fracture of the humeral medial epicondyle – how to treat? Annales Chirurgiae Gynaecologiae. 1996;85:67-71.
7 Lam TP, Ng BKW, Ma RF, Cheng JCY. Monteggia fractures in children a review of 30 cases. Journal of the Japanese Pediatric Orthopedic Association. 2004;13:193-195.
8 Reynders P, De Groote W, Rondia J, et al. Monteggia lesions in adults. A multi-centre Bota study. Acta Orthopaedica Belgica. 1996;62:78-83.
9 Rafai M, Largab A, Cohen D, Trafeh M. Pure posterior luxation of the elbow in adults: immobilization or early mobilization. A randomized prospective study of 50 cases. Chirurgie de la Main. 1999;18:272-278.
4.4 Fractures of the forearm and carpal bones
Radial head fractures
Classification
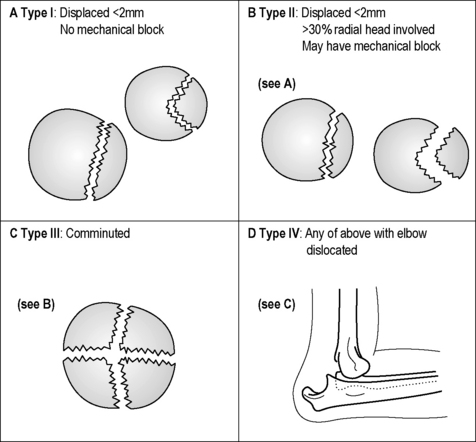
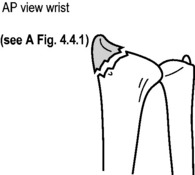
Radial head fractures may be described as hairline, marginal (displaced and undisplaced), segmental (displaced and undisplaced) or comminuted. They may also be classified into four types (Fig. 4.4.1). Fractures of the radial neck may be undisplaced or have various degrees of lateral tilting.
Management
Type I and minor type II radial head fractures without mechanical block may be managed with a bandage and sling. If there is severe pain, aspiration of the fracture haematoma, intra-articular bupivacaine or a back slab may be useful. Mobilization can occur after 1–2 days depending on symptoms. Prognosis is good, but full extension may not be possible for many months.
Shaft fractures
Isolated fracture of the ulnar shaft
Fractures displaced less than 50% of the ulna width heal well with a non-union rate of 0–4%. Traditional treatment involves fixing the forearm in mid-pronation with a plaster cast, extended above elbow if the middle or proximal thirds of the ulna are fractured. The cast is removed once union occurs, usually in 6–8 weeks. Other proven options include a below-elbow plaster (BEPOP) for proximal fractures, early mobilization with bandage after 1–2 weeks in BEPOP, or functional bracing after 3–5 days, which allows movement at wrist and elbow.
Fractures of the distal radius and ulna
Management
Prompt attention to analgesia, splinting and elevation is essential while awaiting X-rays.
Reduction is indicated in the following circumstances to improve long-term function:
Greater deformity can be accepted in low-demand, elderly patients.
Stable, undisplaced, extra-articular fractures can be managed more conservatively with splinting and referral to a family doctor for early mobilization after 4 weeks.
Indications for operative management are debated, but should be considered for:
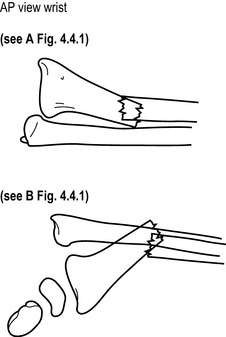
Colles’ fracture
First described in 1814, the Colles’ fracture is a metaphyseal bending fracture. The wrist has a classic ‘dinner-fork’ appearance, often with significant swelling of the soft tissues.This appearance is reflected in the radiographs (Fig. 4.4.3). There is often associated damage to the radioulnar fibrocartilage. There may be comminution, commonly dorsally, which can extend into the radiocarpal or radioulnar joints.
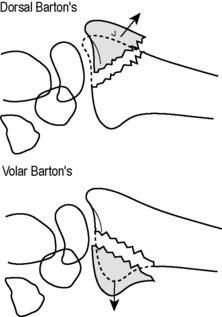
Barton’s fracture
Barton’s fractures are dorsal or volar intra-articular fractures of the distal radial rim (Fig. 4.4.4). The mechanisms of injury are similar to those seen with Colles’ and Smith’s fractures, respectively. There is often significant soft-tissue injury and the carpus is usually dislocated or subluxed along with the distal fragment. These fractures are complicated by arthritis of the radiocarpal joints and carpal instability.
Minimally displaced fractures involving less than 50% of the joint surface and without carpal displacement may be reduced along the lines of a Colles’ or Smith’s fracture. Immobilization should occur with wrist flexed for dorsal Barton’s and extended for volar Barton’s. However, most fractures are unstable and potentially disabling, requiring early operative management, especially in younger patients. Early orthopaedic follow-up is mandatory.
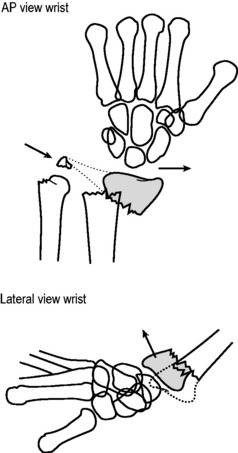
Radial styloid (Hutchison or chauffeur’s) fracture
This oblique intra-articular fracture of the radial styloid is caused by a direct blow or fall onto the hand. Displacement is associated with carpal instability and long-term arthritis. The fracture is seen best on AP X-rays of the wrist (Fig. 4.4.5). Undisplaced fractures can be treated with a cast for 4–6 weeks. Displaced fractures should be referred to an orthopaedic surgeon for anatomical reduction and fixation.
Carpal fractures and dislocations
Dislocations of the wrist
Radiographic features include:
Barton’s fracture/dorsal shearing fracture. Wheeless CRIII, editor. Wheeless’ textbook of orthopaedics, 2008. Accessed Jan http://www.wheelessonline.com/ortho/dorsal_bartons_fracture_dorsal_shearing_frx
Connolly JF. Nonoperative fracture treatment. In Bucholz RW, Heckman JD, Court-Brown C, et al, editors: Rockwood and Green’s fractures in adults, 6th edn, Baltimore: Lippincott Williams & Wilkins, 2005.
Geiderman JM, Magnusson AR. Humerus and elbow. Rosen P, Barker. Emergency medicine, 4th edn, St. Louis: Mosby-Year Book, 1998.
Closed reduction of distal radius fractures. Wheeless CRIII, editor. Wheeless’ textbook of orthopaedics, 2008. Accessed Jan http://www.wheelessonline.com/ortho/closed_reduction_of_distal_radius_fractures
Cruikshank J, Meakin A, Braedmore R, et al. Early computerized tomography accurately determines the presence or absence of scaphoid and other fractures. Emergency Medicine of Australasia. 2007;19:223-228.
de Beaux AC, Beattie T, Gilbert F. Elbow fat-pad sign: implications for clinical management. Journal of the Royal College of Surgeons of Edinburgh. 1992;37:205-206.
Distal Radial Frx: position of immobilization. Wheeless CRIII, editor. Wheeless’ textbook of orthopaedics, 2008. Accessed Jan http://www.wheelessonline.com/ortho/distal_radius_frx_position_of_immobilization
Eisenhauer MA. Wrist and forearm. In Rosen P, Barker R, editors: Emergency medicine, 4th edn, St. Louis: Mosby-Year Book, 1998.
Ferris BD, Thomas NP, Dewar ME, Simpson MA. Brace treatment of Colles’ fracture. Acta Orthopaedica Scandinavica. 1989;60:63-65.
Hanel DP, Jones MD, Trumble TE. Wrist fractures. Orthopaedic Clinics of North America. 2002;33:35-57.
Irshad F, Shaw NJ, Gregory RJ. Reliability of fat-pad sign in radial head/neck fractures of the elbow. Injury. 1997;28:433-435.
Kouros GJ, Schenck RR, Theodorou SJV. Carpal fractures, 2008. Accessed Jan http://www.emedicine.com/orthoped/topic36.htm
Kuntz DGJr, Bararz ME. Fractures of the elbow. Orthopaedic Clinics of North America. 1999;30:37-61.
Mackay D, Wood L, Rangan A. The treatment of isolated ulnar fractures in adults: a systematic review. Injury. 2000;31:565-570.
McRae R, editor. Practical fracture treatment, 3rd edn, London: Churchill Livingstone, 1994.
Uehara DT, Chin HW. Injuries to the elbow and forearm. In Tintinalli JE, Kelen GD, Stapcznski JS, et al, editors: Emergency medicine, 5th edn, New York: McGraw Hill, 2000.
Radial inclination of distal radius frx. Wheeless’ Textbook of Orthopaedics, 2008. Accessed Jan http://www.wheelessonline.com/ortho/radial_inclination_of_distal_radius_frx
Ruch DS. Fractures of the distal radius and ulna. In Bucholz RW, Heckman JD, Court-Brown C, et al, editors: Rockwood and Green’s fractures in adults, 6th edn, Lippincott Williams & Wilkins: Baltimore, 2005.
Sarmiento A, Latta L. The evolution of functional bracing for fractures. Journal of Bone and Joint Surgery. 2006;88B:141-148.
Barton’s fracture/dorsal shearing fracture. Wheeless CRIII, Wheeless CRIII, editors. Wheeless’ textbook of orthopaedics, 2008. Accessed Jan http://www.wheelessonline.com/ortho/smiths_fracture
Szabo RM. Extra-articular fractures of the distal radius. Orthopaedic Clinics of North America. 1993;24:229-237.
Uehara DT, Chin HW. Wrist injuries. In Tintinalli JE, Kelen GD, Stapczynski JS, et al, editors: Emergency medicine, 5th edn, New York: McGraw Hill, 2000.
Van Glabbeek F, Van Riet R, Verstreken J. Current concepts in the treatment of radial head fractures in adults. A clinical and biomechanical approach. Acta Orthopaedica Belgica. 2001;67:430-441.
Villarin LAJr, Belk KE, Freid R. Emergency department evaluation and treatment of elbow and forearm injuries. Emergency Medicine Clinics of North America. 1999;17:843-858.
Volar Barton’s fracture. Wheeless CRIII, editor. Wheeless’ Textbook of Orthopaedics, 2008. Accessed Jan http://www.wheelessonline.com/ortho/volar_bartons_fractures
4.5 Hand injuries
Introduction
Five to 10% of emergency department (ED) attendances involve injury to the hand. Presentations may be due to wounds (∼35%), contusions (∼20%), fractures (∼20%), sprains (∼10%) or infections (∼5%).1 Males injure their hands more than females. The effect of hand injury on an individual cannot be overestimated. Apart from the initial pain and trauma, occupational and psychological concerns play a major role in the aftermath of these injuries. Even a relatively minor fingertip injury can result in an individual being away from work for several days, with consequent loss of earnings and concerns for long-term function and appearance. It is therefore essential that initial assessment and management are appropriate. Complications of traumatic wounds account for the highest number of medicolegal actions against emergency physicians in the United States.
Clinical features
Examination
The injured hand must be examined in a well-lit area. Temporary dressings may need to be soaked off if they have been allowed to dry out and become adherent. At triage an initial moist dressing is ideal, with firm pressure and elevation if there is significant haemorrhage.
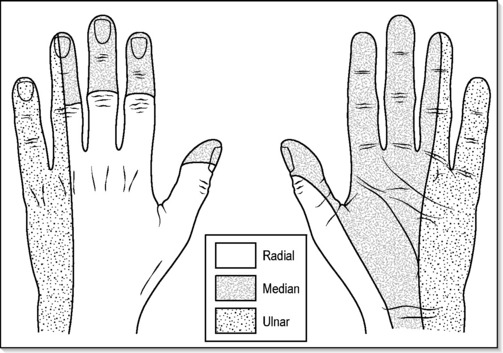
Hand and finger injuries are painful and suitable analgesia must be given to allow full examination. Local infiltration of lignocaine without epinephrine (adrenaline) around a wound or as a digital nerve block will allow examination of all aspects except sensation, which must be tested and recorded prior to anaesthesia. A wrist block is useful when some or all of the hand needs to be anaesthetized (Fig. 4.5.1), and longer-acting local anaesthetic is generally used to prolong the effect.
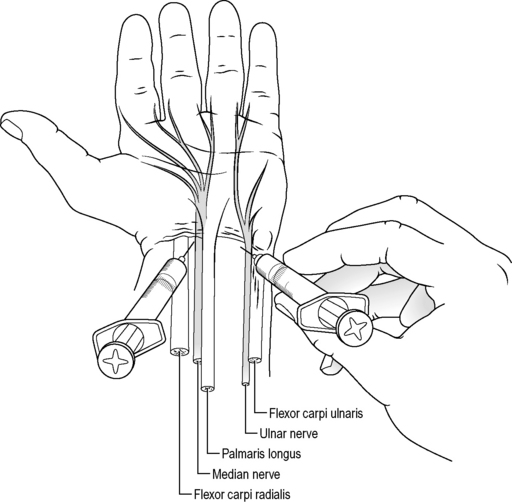
Fig. 4.5.1 Palmar wrist block.
(Reproduced with permission from American Society for the Surgery of the Hand. The hand, 2nd edn. Boston, MA: Churchill Livingstone, 1990.)
Testing sensation is achieved by light touch or two-point discrimination in the distribution of the three main nerves that supply the hand (Fig. 4.5.2). The median nerve supplies the palmar aspect of the thumb, index, middle and half of the ring finger, extending to supply the fingertip and nailbed. The ulnar nerve supplies both palmar and dorsal aspects of the other half of the ring finger and the little finger. The radial nerve supplies the radial dorsum of the hand, thumb, index, middle and radial aspects of the ring finger. If the patient is unable to describe sensation because they are too young or unconscious, it is useful to remember that the digital nerves also carry the sympathetic supply to the fingers, and that division will cause a dry finger in the distribution of the digital nerve.
The hand examination should be holistic and not just concentrate on the obvious injury. Inspection of the hand will provide information about the perfusion of the tissues, local swelling and position of wounds. The resting position of the hand may be a clue to tendon injury, as the normal uninjured position is held with the fingers in increasing flexion from the index to the little finger (Fig. 4.5.3a). A pointing finger may indicate a flexor tendon injury (Fig. 4.5.3b). Obvious bone or joint deformity should be recorded.
Investigations
Most information will be obtained from a full history and examination. Radiology of the hand and fingers will be necessary if bone/joint deformity or tenderness is elicited. Dislocations should always be X-rayed prior to manipulation, however trivial they may seem. Radiography can also reveal radio-opaque glass in a wound. Organic foreign bodies and infections can often be detected by ultrasound imaging using a small-parts soft tissue probe.
Blood investigations are rarely of use in the acutely injured hand.
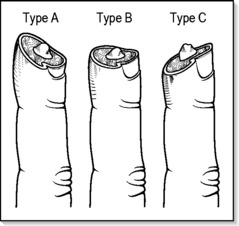
Fingertip injuries
The fingertips have an excellent blood supply and will usually heal if given the correct environment. Fingertip avulsions are classified as type A when the skin loss is oblique dorsal, type B when the loss is transverse, and type C when the loss is oblique volar (Fig. 4.5.4).
The most complex to manage is type C, as there is loss of palmar skin. When there is a type A or B injury involving less than 50% of the nailbed, conservative treatment is often the best option. Care of the fingertip initially is likely to require haemostasis followed by an occlusive dressing. There is good evidence that this kind of dressing promotes healing by being non-adherent and allowing fast re-epithelialization of the fingertip.2 The dressing is also quick to apply, easily removed, and comfortable for the patient. Most other dressings adhere to the wound and pull epithelial cells off when removed. Alternatives to conservative dressings include skin grafts to the fingertips, advancement flaps and cross-finger flaps. These should be performed by surgeons trained in the specialist techniques, and reserved for injuries involving large areas of skin loss.
Digital nerve injuries
Nerve repairs distal to the distal interphalangeal joint are rarely rewarding. More proximal injuries may be repaired under magnification by an experienced surgeon. Salvage of the digital nerve will depend on the extent of local tissue damage.3 Good results are achieved with early repair of digital nerves when the ends can be approximated without tension using a fine (>8/0) suture. The return of protective sensation depends on the level of repair and axon regeneration.
Proximal interphalangeal joint injuries
This is the joint that causes most long-term complications, owing to stiffness and joint contracture. The proximal interphalangeal (PIP) joint is mechanically complex and is supported dorsally by the extensor apparatus, whereas on the palmar aspect is the strong fibrous volar plate. Lateral stability is provided by the collateral ligaments. Rupture of either the volar plate or the extensor apparatus will result in joint instability and potential long-term disability. Tears in the extensor apparatus may result from relatively minor trauma. Dislocations of the proximal interphalangeal joint invariably displace both structures. Occasionally, the central slip of the extensor tendon or the volar plate avulses a small fragment from the middle phalanx which will be visible on lateral finger X-ray. Reduction of dislocations should be followed by extension splinting and early follow-up. The boutonnière deformity (flexion of the PIP joint accompanied by hyperextension of the DIP joint) is a hand surgeon’s nightmare and ideally should be prevented, as long-term results from reconstructive surgery are poor. These injuries should not be underestimated, and ultrasound can be used to aid in early diagnosis.
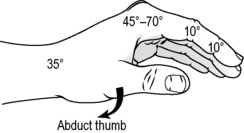
Metacarpal injuries
These injuries are caused by punching, crush injury or falls on to the closed fist. The commonest injury is fracture of the neck of the fifth metacarpal, which is usually best treated conservatively. Correction of significant angulation will only be achieved by open reduction and internal fixation. Spiral fractures of the shaft of a metacarpal will result in shortening of the bone and loss of the contour of the knuckle. Conservative management of these fractures should involve splinting the hand in intrinsic plus (Fig. 4.5.5) with the metacarpophalangeal joint flexed to 70%. The fingers must be splinted straight, with support to the fingertip. Abduction injuries of the thumb may cause a Bennett’s fracture, which is an intra-articular fracture of the base of the thumb metacarpal. Bennett fractures, when displaced, should be referred for internal fixation.
Prognosis
Hand injuries recover best with early definitive treatment, as badly managed injuries can be very difficult to salvage at a later date. Stiffness and loss of function can be avoided if good surgical principles of wound management are adhered to. Appropriate initial splinting and guarded mobilization are the cornerstones of rehabilitation. The injured hand recovers best when splinting has been in a functional position. Whenever possible, the hand should be immobilized with the fingers straight and the MCP joints flexed to 70°. This can be achieved in even the most swollen hand by careful application of a volar plaster slab. Early referral for definitive surgery and subsequent rehabilitation will be essential for severe or complicated injuries. An explanation to the patient of the need to prevent joint stiffness is important when the finger requires dressings for more than 3 weeks.
Prevention
1 Angermann P, Lohmann M. Injuries to the hand and wrist. Journal of Hand Surgery. 1993;18B(5):642-644.
2 de Boer P, Collinson PO. The use of silver sulphadiazine occlusive dressings for fingertip injuries. Journal of Bone and Joint Surgery. 1981;63B(4):545-547.
3 Jabaley M. Technical aspects of peripheral nerve repair. Journal of Hand Surgery. 1984;9:9-14.
American Society for the Surgery of the Hand. The Hand – primary care of common conditions, 2nd edn. Boston, MA: Churchill Livingstone, 1990.
Atasoy E, Ioakimidis E, Kasdan ML, et al. Reconstruction of the amputated finger tip with a triangular volar flap. Journal of Bone and Joint Surgery. 1970;52A:921-926.
Hart RG, Kleinert HE. The hand in emergency medicine. Emergency Medicine Clinics of North America. 1993;11:755-756.
Quinn J, Cummings S, Callaham M, Sellers K. Suturing versus conservative management of lacerations of the hand (RCT). British Medical Journal. 2002;325:299-300.
Stewart C. Hand injuries. Emergency Medicine Reports. 1997;18:223-234.
4.6 Pelvic injuries
Anatomy
The pelvic ring is formed by the two innominate bones and the sacrum. The innominate bones are made up of the ileum, ischium and pubis, and are joined anteriorly at the symphysis pubis and posteriorly at the left and right sacroiliac joints.
Classification of pelvic fractures
The Young and Resnik classification outlined in Chapter 3.8 classifies pelvic fractures by the mechanism of injury and the direction of the causative force. It does not include isolated fractures outside the bony pelvic ring, or acetabular fractures, which are discussed later in this chapter.
Young and Resnik pelvic fracture classification
Anteroposterior compression injuries
Type 2 injuries
Type 2 injuries classically cause an open-book fracture. They involve rupture of the anterior sacroiliac, sacrospinous and sacrotuberous ligaments posteriorly and disruption of the pubic symphysis anteriorly. There is widening of the anterior sacroiliac joint with diastasis of the pubic symphysis by more than 2.5 cm on radiology, and occasionally avulsion of the lateral border of the lower sacral segments. Considerable force is involved to disrupt these ligaments, and neurovascular injuries and complications are common. The pelvis is unstable to external rotation, and external compression will ‘spring’ the pelvis.
Type 3 injuries
Type 3 injuries occur when an even greater force is applied and involve disruption of all the pelvic ligaments on the affected side. Rupture of the posterior sacroiliac ligaments leads to lateral displacement and disconnection of the affected hemi-pelvis from the sacrum. They are completely unstable and are associated with the highest rate of neurovascular injury and haemorrhage (see Fig. 4.6.1).
Injuries associated with pelvic fractures
Genitourinary and bladder injuries
Pelvic fractures are associated with injury to the lower urinary tract in up to 16% of cases. They are more prevalent in males, who sustain a much higher rate of urethral injury. Pelvic trauma may also result in bladder rupture. The bladder is normally protected by the pelvis, and rupture usually indicates significant disruption of the pelvic ring.
Management of unstable pelvic fracture
Stable fractures of the pelvis
Isolated avulsion fractures
Anterior superior iliac spine fracture
The anterior superior iliac spine may be fractured in jumping activities due to powerful contraction of the sartorius muscle. Such injuries cause pain on weightbearing, with local tenderness and swelling at the fracture site. Active flexion and abduction of the thigh reproduces the pain. There is usually minimal displacement of the avulsed fracture on the AP film of the pelvis.
Acetabular fractures
Blackmore CC, Cummings P, Jurkovich G, et al. Predicting major hemorrhage in patients with pelvic fracture. Journal of Trauma. 2006;61:346-352.
Burgess AR, Eastridge BJ, Young JW, et al. Pelvic ring disruptions: effective classification system and treatment protocols. Journal of Trauma. 1990;30:848-856.
Dalal SA, Burgess AR, Siegel JH, et al. Pelvic fracture in multiple trauma: classification by mechanism is key to pattern of organ injury, resuscitative requirements, and outcome. Journal of Trauma. 1989;29:981-1002.
Fallon B, Wendt JC, Hawtrey CE. Urological injury and assessment in patients with fractured pelvis. Journal of Urology. 1984;131:712-714.
Gokcen EC, Burgess AR, Siegel JH, et al. Pelvic fracture mechanism of injury in vehicular trauma patients. Journal of Trauma. 1994;36:789-796.
Kellam JF. The role of external fixation in pelvic disruptions. Clinical Orthopaedics and Related Research. 1989;241:66-82.
Mattox KL, Bickell W, Pepe PE, Mangelsdorff AD. Prospective randomized evaluation of antishock MAST in post-traumatic hypotension. Journal of Trauma. 1986;26:779-786.
Pennal GF, Tile M, Waddell JP, et al. Pelvic disruption: assessment and classification. Clinical Orthopaedics and Related Research. 1980;151:12-21.
Rothenberger DA, Velasco R, Strate R, et al. Open pelvic fracture: a lethal injury. Journal of Trauma. 1978;18:184-187.
Sarin EL, Moore J, Moore E, et al. Pelvic fracture pattern does not always predict the need for urgent embolization. Journal of Trauma. 2005;58:973-977.
4.7 Hip injuries
Anatomy
The hip joint is a large ball and socket articulation encompassing the acetabulum and proximal femur. The hip joint provides a high degree of stability and mobility.
Classification of hip fractures
Intracapsular fractures
Femoral neck fractures
Intracapsular fractures are four times more common in females than males. There are four main causes of this type of injury:
Extracapsular femur fractures
Intertrochanteric femur fractures
Classification
Numerous classification systems are available for intertrochanteric fractures, the simplest of which is by Evans. This divides intertrochanteric fractures into stable and unstable. However, for the emergency physician an anatomical description of the fracture detailing the degree of comminution, subtrochanteric extension and the presence of displaced posterior fragments is adequate (Fig. 4.7.1).
Management
A complete evaluation is essential to formulate an early treatment plan, as intertrochanteric fractures occur most frequently in the elderly. Patients may lose up to 1.5 L of blood from comminuted fractures and are often dehydrated, malnourished and in significant pain on arrival in the emergency department (ED). Systemic analgesia and fluid resuscitation are important in preparation for theatre.
Subtrochanteric femoral fractures
Management
The affected limb should be immobilized in a splint following parenteral analgesia. Suitable splints include proprietary splints such as the Donway or Hare, and fluid resuscitation started as required. The older, more laborious Thomas splint is rarely now used. Orthopaedic referral is necessary for open reduction and internal fixation of these fractures.
Hip dislocation
Posterior dislocation
Closed reduction
Closed reduction of posterior hip dislocations may be performed in the ED under procedural sedation, unless there is immediate access to an operating theatre (see Chapter 22.3).
Anterior dislocation
Management
A thorough general examination looking for associated life-threatening injuries is essential, as these injuries are usually associated with high-energy trauma. Orthopaedic consultation is mandatory because of the high probability of vascular injury and the need for closed reduction under general anaesthesia.
Dahners LE, Hundley JD. Reduction of posterior hip dislocations in the lateral position using tractioncountertraction: safer for the surgeon? Journal of Orthopaedic Trauma. 1999;13:373-374.
Garden RS. The structure and function of the proximal end of the femur. Journal of Bone and Joint Surgery. 1961;43B:576-589.
Hirasawa Y, Oda R, Nakatani K. Sciatic nerve paralysis in posterior dislocation of the hip. Clinical Orthopedics. 1977;126:172-175.
Holmberg S, Conradi P, Kalen R, Thorgren KG. Mortality after cervical hip fracture: three thousand two patients followed for six years. Acta Orthopaedica Scandinavica. 1986;57:8-11.
Jazayeri M. Posterior fracture dislocations of the hip joint with emphasis on the importance of hip tomography in their management. Orthopedic Review. 1978;7:59-64.
Keller CS, Laros GS. Indications for open reduction of femoral neck fractures. Clinical Orthopedics. 1980;152:131-137.
Walden PD, Hamer JR. Whistler technique used to reduce traumatic dislocation of the hip in the emergency department setting. Journal of Emergency Medicine. 1999;17:441-444.
4.8 Femur injuries
Femoral shaft fracture
Classification
The majority of fractures occur in young adults with healthy bones and are transverse fractures. Greater mechanical force usually results in comminution (Fig. 4.8.1). Minimal force with pathological bone tends to produce metaphyseal fractures with propagation into the shaft.
Clinical evaluation
Vascular damage is usually limited to rupture of the profunda femoris perforating branches in closed fractures. The resulting tense, swollen haematoma is limited to the thigh and is not associated with distal circulatory compromise. However, penetrating trauma and open fractures may cause femoral artery disruption with distal circulatory compromise, so repeated vascular evaluations are important. Any evidence of an expanding haematoma or diminished distal pulses requires further investigation with Doppler imaging or arteriography.
Management
Analgesia
Adequate pain relief is essential in the ED. Intravenous opioid analgesia is necessary, titrated to effect. A femoral nerve block is an important adjunct that should be considered prior to fracture reduction (see Chapter 22.2).
Provost R, Morris J. Fatigue fracture of the femoral shaft. Journal of Bone and Joint Surgery. 1969;51A:487-498.
Russell RH. Fracture of the femur. A clinical study (Abridged by Peltier LF). Clinical Orthopedics. 1987;224:4-11.
Taylor M, Banerjee B, Alpar E. Injuries associated with a fractured shaft of the femur. Injury. 1994;25:185-187.
Vanganess C, DeCampos J, Merritt P. Meniscal injury associated with femoral shaft fractures. An arthroscopic evaluation of incidence. Journal of Bone and Joint Surgery. 1993;75:207-209.
West H, Turkovich G, Donnell C. Immediate prediction of blood requirements in trauma victims. Southern Medical Journal. 1989;82:186-189.
4.9 Knee injuries